One of the most exhilarating and similarly terrifying moments for an architect is facing a blank piece of paper or computer screen.
Where do designers go from there? What happens if the status quo changes? How can the complex requirements for supportive and healing environments be met without relying on past clichés or present fads? How does the industry respond to trends in health care design?
Whether facing typical projects or ones never before encountered, architects need to address each problem with a fresh approach and design without precedent.
What has been created?
Nobody will dispute that health care design has elevated its position and there is a collective understanding of the importance of the built environment as it relates to health care outcomes.
But, if viewed in a historical context, design for the "new institution" in health care has changed every 20 years. A design professional can walk through a hospital and accurately define the era in which a particular building was designed and built. Every generation follows the set of rules that are in vogue at the time, from the evolution of fresh air camps to cruciform plans to "the racetrack plan" on a podium and, more recently, the applications of the Planetree patient-centered philosophy and evidence-based design. At times, it seems health care design has been limited to the creation of fashion and the new institution. Every month, many journals tout innovations—yet the more new facilities are supposed to be different, the more they look the same.
In certain ways, health care designers are bound by the health care metrics that surround them—metrics that are not challenged, just followed. Examples would include the Guidelines for Design and Construction of Health Care Facilities, a myriad of codes, standards and guidelines issued by groups such as the Joint Commission, National Fire Protection Association, American Society for Healthcare Engineering and current philosophies such as evidence-based design, Planetree and sustainability. Suddenly, health care architects are experts in each of these areas, claiming their experience as they respond to the most recent request for proposal (RFP).
Designers tend to follow the same tried-and-true design process of developing a qualitative/quantitative program: Take benchmarking trips to see how someone else did it, consider precedent and rely on practical experience. There are several user meetings during design but here, too, medical professionals are viewing design opportunities from a limited perspective of their own practical experience. While inclusion of these metrics or processes may serve an important purpose, architects need to avoid seeing these as prescriptive and conclusive. Instead, they serve as the compulsories of design, with the "free-skate" still ahead.
What will be faced?
Arguably, one of the most challenging aspects of a health care design practice is keeping current on the ever burgeoning volume of information and changes. New specialized needs and emerging trends are affecting the health care industry. They include the following:
• The exploding cost of health care and the government's involvement to bring it under control;
• The increasingly obese patient population;
• The coming wave of baby boomers, an aging population that is interested in having it their way right up to the end;
• The growing concern of pandemics such as H1N1 or catastrophic events that can travel around the globalized world in minutes and hours;
• Mental illness and the responsibility to take it out of the closet and treat it with the same fervor as "normal" health problems; and
• Energy usage in health care buildings.
Returning to the roots
In considering these emerging trends, what tools and tactics does the health care community need to employ?
The design community has an obligation to face these challenges and possesses the ability to overcome them, but not by continuing the status quo. Architects have the training, experience and capability to innovate.
To make this practical, the following list outlines key opportunities or junctures where design professionals can affect the course of an outcome:
Rethink the players. The health care industry can no longer function in silos as designers, constructors, owners, users and regulatory officials to the exclusion of the patients.
The process of building requires joint ownership of a system that leverages the wisdom, abilities and technology of each stakeholder entity. The industry calls this "integrated project delivery."
Rather than waiting for the attorneys to write agreements, the team needs to go to the owner with a customized delivery that supports the mission, budget, schedule and needs of the institution.
 One of the key tenets of health care reform is bundled services. The architect can lead the way in demonstrating the benefits of bundled services—delivering a project sooner, with fewer problems and better outcomes.
One of the key tenets of health care reform is bundled services. The architect can lead the way in demonstrating the benefits of bundled services—delivering a project sooner, with fewer problems and better outcomes.
In this process, all team members need to be retained at the outset of the project and participate from start to finish. Current and past patients need to be included when evaluating the design needs for their feedback and valuable insight. Finally, an owner is served best when the design professional leads the design process and the constructor leads during the construction phase.
Rethink the investment. Every stakeholder in the health care industry must manage a profitable business. Whether it is leveraging technology, evaluating effective teams to better produce product or looking for ways to cut overhead, architects must understand what it takes to make a business work. It is no different for the health care owner. Thus, design professionals must understand how their recommendations positively affect the bottom line of their health care clients.
The industry continues to think that the key cost factors of a health care building are the bricks and mortar. However, the real cost is in health care delivery and processes. Rather than retreat to the same old patterns, the integrated team needs to take a new perspective and critique the delivery of health care and the mission that the hospital embraces to invest in the future.
In an imaginary scenario, a hospital is like an assembly line that takes sick people in at one end and sends healthy people out the other end.
What can be done differently? Would departments function in that model? Can the same thought process be applied to the inefficiency of territorial boundaries, multiple registration points and the inherent repetition in the health delivery process today?
The estimation of the amount of area built for these spaces as an initial outlay, added with the lifetime cost of multiple full-time equivalents (FTEs) performing the same function at a utilization rate of 65 percent, plus the lost opportunity cost of a space that could be used for patient care, results in a staggering impact to the bottom line.
Rethink the key drivers. By not accepting the "new institution" or current fad, designers can step back and treat each design problem as an opportunity to explore what really matters. This does not suggest the creation of a research project, but rather expanding beyond the limitations of the guidelines and precedent. One advantage some designers have is the opportunity to work on multiple building types: Outpatient surgery centers are using restaurant-type pager systems while inpatient areas are created with hospitalitylike ambience.
Elements of other building types can be transferrable to the myriad of functional requirements of a health care facility. For instance, people spend the night there, so it's a hotel; people eat there, so it's a restaurant; energy is created and distributed, so it's a power plant; materials are managed and processed, so it's a factory; supplies are distributed, so it's a distribution center; data is stored and managed, so it's a data center; people are trained, so it's an educational facility; business is transacted, so it's a corporate office building; large crowds move through every day, so it's a transit station; and life and death are faced every day, so it is a spiritual place.
Most important, a hospital is a place for the care and healing of people and for those who take care of them. Rather than limits, the definition of a hospital needs to expand.
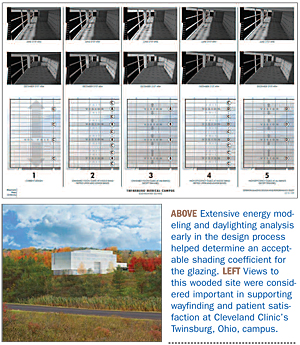
Rethink the energy. Health care facilities are the biggest users of energy (second behind food preparation facilities). Mechanical-electrical-plumbing systems represent 40 percent of the construction cost and generally affect a significant portion of an operating budget for a health care facility. Engineers need to be engaged at the start of the design process, with an equal voice.
The same consideration that is put into programming and design should be put into the basis of engineering design. The end product should be the focus, not the number of Leadership in Energy and Environmental Design points, which is simply a guideline to what designers should be doing as a prerequisite.
Additionally, a cost model should be created to maintain a level of quality necessary to accomplish goals. The communication of real benefits with the owner avoids trading the quality of the HVAC system in a value-engineering exercise late in design.
Finally, commissioning should be viewed as an opportunity to not only achieve the desired system performance, but also demonstrate the impact on the hospital's long-term operating budget. The most successful way to implement this approach is to properly represent to the C-suite the impact of a design's value to the bottom line.
Rethink the implementation. As health care environments are viewed by how they affect the outcomes of the delivery of care, design becomes the product of a changed process. But this is of little value without the involvement and support of the entire project team. Challenge the project team to define a short list of measurable goals at the outset of a project. Revisit those goals throughout the design and construction of the project.
Start today
Considering the momentum that has been generated already, the design profession has a great opportunity to further its mission by returning to its roots and designing without precedent.
Emerging trends and challenges lie ahead. Start today. If not now, when? If not architects, who?
Phil LiBassi, AIA, ACHA, is principal at the firm of Westlake, Reed, Leskosky in Cleveland. He can be contacted via his e-mail address at pliba@WRLdesign.com.
| Sidebar - Problem-solving progression |
| As the health care industry faces today's unprecedented challenges, each facility project presents an opportunity to design without precedent, to question and challenge in order to answer and solve. To implement this process, architects should use the following progression: |





