 |
|
Interactive television systems can be integrated with nurse calls, electronic health records and other systems. Photo courtesy of TeleHealth Services |
Building systems, medical equipment and information technology (IT) devices all have unique operational needs.
However, basic vendor testing and standard punch lists do not address the configurations required to meet the operational needs of health care technology systems.
Defining the operational configurations, functional testing parameters and commissioning requirements for these diverse technologies and complex integrations is required.
Industry drivers
An overabundance of new medical technologies and systems are flooding health care facilities and most have complex setup, configuration and testing requirements. Special building systems such as sound monitors, room status devices, real-time locating systems (RTLSs), integrated nurse call systems and integrated closed-circuit television (CCTV) solutions require detailed implementation plans and rigorous startup testing.
Several of these health care technologies such as nurse call, access control, code blue and infant security have some limited vendor commissioning requirements and standards.
However, most health care technologies deployed today have owner-defined operational configurations, interoperabilities and integrations that bridge multiple systems and infrastructure. These include integrated surgical video, nurse calls, interactive televisions, RTLSs, distributed antenna systems, telemetry, patient beds, physiological monitoring, automated medication dispensing and wireless telephones.
Many of their integrations are often mistakenly assumed to be plug-and-play, but those assumptions may create serious operational and patient safety issues that can result in death. For example, the 2014 Top 10 Health Technology Hazards list by ECRI Institute, Plymouth Meeting, Pa., names alarm hazards as the No. 1 risk. Many of these risks are created by false alarms and nuisance alarms generated by failed integrations and improper configurations. Commissioning of these many complex technologies requires a specialized focus.
Commissioning challenges
Traditional commissioning doesn't fully address health care technology, leaving the owner with incomplete solutions. Commissioning is focused only on contractor-furnished items and typically ignores the necessary integrations with owner-furnished medical technologies and the clinical requirements necessary for full functionality to meet staff needs and expectations.
Many assume medical technology vendors address these needs but the vendor functional testing requirements do not address operational intent. Vendor testing ensures that the light comes on and data are transmitting, but on the vendor's end only. Their contracts typically do not span the multiple systems needed to meet the hospital's functional requirements.
Owners now should begin incorporating detailed commissioning requirements into vendor requests for proposals (RFPs) and purchasing contracts to help ensure proper implementation and activation.
Facilities and design teams are accustomed to evaluating operational requirements and total cost of ownership for energy management systems. Unfortunately, this process is not being applied to the many complex technologies in hospitals today.
In a recent health care construction project, a facility discovered a year after opening that it had spent $240,000 on an RTLS that was being accessed only by three people in the biomedical department to find equipment to be serviced. The technology champion that led the RTLS charge during the project design phase to maximize staff efficiencies was no longer at the facility, and only a generic specification for the system was developed during his tenure.
The contractor turned over a fully tested solution as it was specified, but no operational configurations were required by specification so the system configuration defaulted to the biomedical department to determine and utilize. The original operational intent was to maximize staff workflow through the system's tracking capabilities, but the necessary complex software solution was not implemented as planned. Defining the proper commissioning requirements early in the design would have helped to avoid underutilizing the technology and would have maximized the return on investment.
Detailed operational intent often is overlooked in medical technology planning. Assuming that this has been addressed by somebody else, such as the design team, contractor, vendor or IT department, creates a negative impact to staff workflow and patient safety. Facilities must move beyond selecting technology and devices. Similar to building management system planning, they must spend time early in the design process defining the overall operational intent for the health care technologies to be implemented. This process and its resulting documentation are needed to ensure that operational intent is incorporated into the owner's RFPs and specifications as required.
Medical device integration is another daunting challenge with which most facilities struggle. These integrations can have extremely complex and diverse requirements. For instance, a smart bed can provide wired and wireless capability to autopopulate the electronic health record (EHR) with patient information, incorporate clinical protocol reminders on separate software and integrate with the nurse call system, television system and wireless phones to assigned caregivers. Likewise, some ventilators will autopopulate the EHR through bedside gateway devices by a middleware vendor, as well as utilize separate clinical software with alarms sent to the assigned caregiver's wireless telephone. Additionally, physiological monitors and telemetry integrate with the EHR, sending waveforms to wireless devices utilizing the hospital's wireless local area network, which can ride on a shared distributed antenna system.
Each of these examples touches multiple systems, implementation teams, departments, users, contractors and vendors that must be carefully orchestrated during the design process — not when the system goes live. Assuming that medical devices are plug-and-play or that the biomedical department or IT department is solely responsible for the devices has caused many failed implementations. Building commissioning addresses the cabling infrastructure, but doesn't tackle the clinical requirements of medical devices. Facilities must embrace a comprehensive integrated health care technology activation philosophy and a plan that spans well beyond commissioning.
Strategies and solutions
Health care technology commissioning requires complex planning from the beginning of the project. It must begin with a detailed health care technology master plan that incorporates the facility's technology vision for the future. Hospitals and health systems often overlook incorporating these goals into overall facility master planning, which creates substantial strains on project startups that missed the operational needs. This approach helps to reduce the technology surprises that many new projects face.
Team responsibilities often are assumed when it comes to health care technology planning and commissioning. Facilities should determine the gaps early in the design stage so that roles and responsibilities are defined clearly.
Defining who provides the systems, infrastructure, medical devices, IT devices, telecom devices and special systems is only the beginning of this process. The facilities professional must determine the department heads, consultants and vendors who will configure the entire solution to meet the operational intent. Next, the professional will need to assign responsibilities to those who will test the individual items in order to provide a complete solution, and select the people who will manage medical equipment interoperability so that it aligns with the clinical goals.
The facilities professionals also should define who will ensure that the complete solution across multiple building systems, technologies and medical devices is fine-tuned before, during and after the system goes live.
Finally, a specialized team focused on health care technology will need to be formed to achieve real success and avoid gaps that many projects overlook. Given the multifaceted technology requirements, this team must engage and incorporate key project leadership from the design team, general contractor, biomedical department, IT, facilities department, security and administration.
 |
|
Traditional nurse call system commissioning requires testing to confirm visual and audible communication of patients and staff, but not integrations with other systems. Photo courtesy of Rauland-Borg Corp. |
Traditional commissioning plans for contractor-furnished items primarily focus on energy management systems and basic building systems to achieve substantial completion and meet the overall building's functional goals. A specialized technology team also must handle the complex owner-furnished medical technologies that fully address the operational and clinical goals.
Many of these technologies, special systems and medical devices offer excellent clinical solutions that support staff efficiencies and better patient outcomes, but must be set up and configured to meet operational requirements.
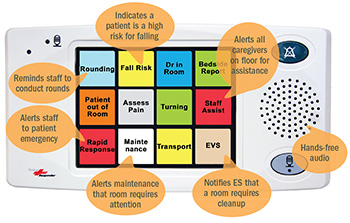
Something as basic as a touch-screen nurse call staff terminal offers custom event-driven workflow solutions that must be programmed to meet each unit's specific needs, which can range from rounding reminders to room-clean notifications, security alerts and blood-draw requests with electronic health record integration for lab result notifications. Another consideration is determining which IV pump alerts should be selected for routing through the nurse call system and to which assigned caregivers. Each of these examples requires clinical input to develop proper configurations.
Facilities should establish focused user-configuration meetings to define and develop operational narratives as well as workflow and device configuration diagrams that align with the overall health care technology vision. This detailed information should be incorporated into an owner's vendor RFPs and project construction documents to avoid the typical scope gaps that challenge most installations. These items become the foundation for developing the technology commissioning plan and help to narrow down the integrations that need to be addressed.
Technology integration management is a critical part of technology commissioning. Some of the hundreds of medical technology integrations that must be managed include infusion monitoring to wireless telephones; interactive televisions to the health information system; physiological monitoring to wireless devices; nurse call systems to wireless telephones; pharmacy robotics to the medication management system; and RTLS to wireless telephones. The specifics for these integrations will have been captured during the user configuration meetings.
It is important that facilities professionals evaluate these technology integration points and manage progress and vendor changes up to opening day. Ongoing health care technology commissioning meetings should be established proactively to help manage these integrations, equipment and systems, including determining required software interfaces, managing middleware requirements, coordinating systems and equipment with EHR for direct data capture, testing interfaces, achieving vendor certification, capturing network ports, obtaining Internet protocol addressing requirements and identifying IT security requirements. A project technology integration map should be developed to give the team an overall perspective of scope that can be reviewed as potential changes occur.
The shelf life of medical devices, IT devices and special systems is short, and technology utilization changes quickly. Thus, reviewing submittals for hospital-purchased technologies is extremely important in coordinating the integrations as new versions or software updates are released. These items should be reviewed by the specialized team for compliance with project vision and with the agreed commissioning standards. Regular technology commissioning team meetings should be established to track schedules and the progress of implementation for owner-furnished technology, proactively coordinating contractor infrastructure and integration requirements.
Facilities professionals also should consider establishing periodic technology steering team meetings to help ensure that the defined integrations and technologies still align with the facilities' overall technology vision.
Ultimately, the final stages of activation bring the biggest challenges in health care technology commissioning. Clear definition of final vendor testing and documentation expectations helps to soothe implementation woes. Medical technologies and special systems have specific requirements for proper testing, and operational intent must be incorporated into final vendor testing, documentation and system configurations. In addition, emergency mode procedure must include all health care technologies.
The technology is not necessarily functional just because the power re-engages it. The multiple layers and overlaps in infrastructure shared by health care technologies must be properly sequenced and tested to ensure proper startup when power is lost. Facilities professionals must develop a rigorous testing plan for all technologies that go beyond basic functional testing.
Thorough training and orientation is another key factor to the successful implementation of these intricate technologies. Many facilities professionals default to the standard contracts for training needs, but that typically only covers minimal requirements. Many of these medical technologies should include a series of training events from initial orientation to on-site training to post-occupancy, follow-up training.
Both staff and maintenance team training is needed for medical technologies. The technologies maintenance team should include superusers who can support clinicians on the units on a daily basis, including coordinating pertinent manufacturer certifications. Ongoing staff requirements and resources to properly maintain and service the technologies also should be discussed. This will ensure that staff training for proper technology utilization not only meets accrediting agency requirements, but also meets overall operational goals.
Ensuring success
Building system commissioning has been an industry standard for years, but the complexity of health care technologies and the corresponding operational configurations now demand more specialized commissioning as well.
Medical equipment, IT devices and special systems require long-term planning and complex project management processes for proper implementation.
In addition to the standard commissioning agent, a team dedicated to technology commissioning will help to ensure project activation success and maximize the facility's return on its technology investment.
Ted Hood is senior vice president and chief operating officer at GBA, a health care technology consulting firm based in Franklin, Tenn. He can be reached at ted.hood@gbainc.com.
Integrating new technologies with legacy systems
A recent patient tower addition project integrated an existing wireless phone system with the new nurse call system and physiological monitoring. The goal was staff efficiency through direct patient communication and alarm notifications to assigned caregivers.
The contractor was providing the nurse call system and structured cabling, the hospital's information technology (IT) department provided the wireless local area network access points, the hospital's biomedical department provided the monitors, and the hospital's telecom team provided the wireless phones.
Each thought its vendor had the rest under control, but no one thought about who would test the system from monitor through the nurse call system to the wireless phones, and who would configure the operational settings on each technology. During activation phase, these assumptions created last-minute scrambling of the entire team.
Eventually, they understood that an integrated approach was required and they were able to adjust quickly. They determined that the existing wireless phone software system was unable to transmit the physiological monitoring and nurse call alerts. Although this caused additional project costs and rework, they were able to coordinate an integrated implementation to provide a working solution in time for opening day.
After the system went live, however, new challenges arose. The technology was functioning, but system configuration omissions and improper alerts were causing disruption in patient care. The entire team regrouped to assess the issues. Although each team member had discussed his or her individual configurations with the clinicians, they hadn't clearly conveyed the complete end-to-end solution to the users. They determined that a comprehensive team configuration planning effort with the users was needed to fine-tune the system.
Once they realized the clinicians' expectations, it only took a couple of days to make the final configuration adjustments to meet the operational needs.
By Ted Hood, senior vice president and chief operating officer at GBA, Franklin, Tenn.
Devising fixes after occupancy
During a post-occupancy assessment of a small community hospital that had recently completed new construction, it was discovered that the nurses detested the real-time locating system (RTLS), nurse call system and wireless phones. Issues included dropped calls, incorrect patient room alerts to wrong caregivers, excessive alerts and notifications.
Evaluation determined that the systems had been programmed and configured incorrectly to meet the facility's needs. The nurse call system was receiving workflow reminders from the RTLS, but call escalation times had been modified to provide quicker response to patient care.
It was discovered that the nurse call system was programmed with durations so short that, in most instances, the nurse was physically unable to get to the room in which the call was initiated before another reminder alert was sent. In addition, if the nurse was caring for a patient, the system would escalate the alert to nurses on the floor within minutes, creating unnecessary staff frustration. Simply adjusting the duration by three minutes resolved the issue.
The staff also complained that the nurse call system and wireless phone communications to patients were not working. Dropped calls and incorrect calls from unassigned patients in other units were occurring daily, even though the phone system was working correctly. The issues were twofold.
First, wireless phones were occasionally being shared between units, but not all patient rooms were unassigned from previous units, causing calls to be misrouted. Laminated wireless phone assignment cheat sheets were provided at each nurse master console, which immediately limited improper phone assignment issues.
Second, it was determined that the dropped call issues were related to the owner's wireless local area network settings. Simply adjusting the system to prioritize wireless phone traffic resolved the problem.
By Bill Miles, PE, project manager at GBA, Franklin, Tenn.





