A growing number of hospital environmental services teams are using fluorescent marking gel systems to measure cleaning thoroughness. The DAZO system from Ecolab is part of the EnCompass environmental monitoring program. Results from the monitoring efforts can be entered into an iPhone app so managers can monitor and benchmark cleaning performance.
Over the past several years, the environmental services (ES) department at Moffitt Cancer Center in Tampa, Fla., has been steadily adding technology to help fight the potential spread of pathogens, measure cleaning thoroughness and improve terminal room cleaning. In addition, the team has standardized processes, using microfiber mops, cloths and wipes to improve cleaning effectiveness and efficiency and to minimize cross-contamination risks.
So, when Vancomycin-resistant enterococci (VRE) levels began to rise in some units of the facility about a year ago, ES, nursing and infection control leaders quickly huddled to strategize on the best way to combat the problem. One of the initial out-of-the-box solutions implemented was to have some of the nurses cohort in VRE isolation rooms to prevent the potential spread of pathogens to non-isolation rooms. The ES team also revised its practices.
“We implemented a process in which our staff clean all the non-isolation rooms first and, once we complete those rooms, we clean the isolation rooms,” explains LaWanda Courtney, director of environmental services. “This practice allows us to minimize cross-contamination risk of environmental surfaces and to reduce the role of the ES department in transmission of health care-acquired infections.”
Combined with the ES team’s other carefully defined protocols, including the use of two ultraviolet (UV) light-disinfection units on high-priority floors like the bone marrow transplant unit, the cohorting process apparently helped to reduce the incidence of VRE in the affected units.
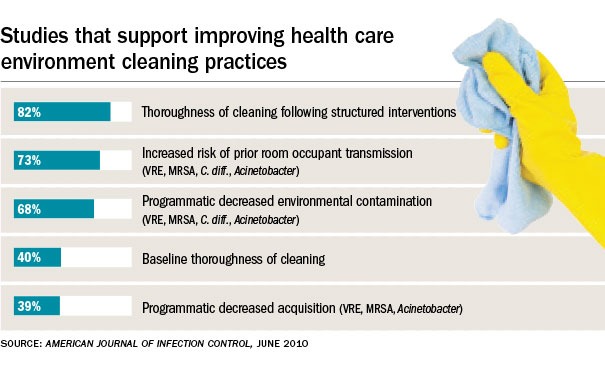
Across the country, more and more ES departments are taking a similar approach. They’re expanding the use of technology to improve patient safety, and measure and monitor cleaning processes and hand-hygiene compliance. In addition, many organizations are deploying handheld computer devices, patient-flow software and other tools to help optimize the efficiency of their teams.
In search of efficiency
With downward spending pressures continuing to mount as hospitals and health systems try to bend the cost curve, many ES departments have endured significant cuts despite their foundational importance in improving safety and patient satisfaction. Many teams find themselves cleaning more square footage with the same number or fewer full-time equivalents in their main campus buildings and in outpatient care facilities that continue to be pushed farther out into communities. These trends present complex management challenges. Thus, it’s not surprising to see many ES departments taking a harder look at technologies that can help them boost safety, performance and efficiency.
Greg May, CHESP, director of environmental services, linens and sustainability at UC San Diego Health System, has issued iPads to all of his managers to carry with them to complete room cleaning inspection reports and other information. Managers open inspection reports from an iShare site that May’s administrative assistant set up. The forms used in the system can be converted easily to Excel files.
“We evaluate the data to see who’s doing well, what our fail rates are and then we report the information to infection control,” May says.
His managers perform a six-point visual inspection of at least 10 cleaned rooms per day. Combined, the managers inspect 200 rooms per week. In addition, the managers use fluorescent marking gel to measure cleaning thoroughness of 18 high-touch points in patient rooms. Managers conduct at least two of these checks a day or 10 per week in discharge rooms or OR suites.
Elsewhere, many organizations have begun evaluating or using automated disinfection systems to enhance safety of their cleaning and disinfection processes. UV light disinfection and hydrogen peroxide vapor systems are turning up in a greater number of hospitals. The systems are designed to offer post-room cleaning implementation to kill bacteria throughout patient rooms, bathrooms, ORs and other areas.
Automating room disinfection
Emory University Hospital Midtown, Atlanta, is among a growing number of facilities that recently have added UV light disinfection to provide an extra level of patient safety. Terry L. Frazier, interim director of environmental services at the 511-bed, community-based, acute care teaching facility, says the organization recently implemented two UV light disinfection units.
“We’re very aware of the dangers of health care-acquired infections such as Clostridium difficile, methicillin-resistant Staphylococcus aureus (MRSA) and Norovirus and, although our facility has not experienced increased outbreaks, we want to put measures in place to reduce the risk and help to prevent these types of pathogens from spreading to patients and staff,” Frazier says.
The ES team currently uses the UV light disinfection units in contact isolation rooms — primarily in C. difficile and MRSA patient rooms. The devices were put into use in August on two shifts and a third shift of use was added in October.
“We have started tracking infection rates and have been pleased with the results so far, but as we’ve only been using the devices for a few months, we look forward to seeing how it will impact our overall infection rates over time. We are doing some adenosine triphosphate testing in coordination with infection control,” Frazier says.
Vennie Henderson of Sodexo and general manager of ES at Sharp Chula Vista (Calif.) Medical Center, helped to oversee the implementation of a UV light disinfection system at his facility several months ago.
“Hand hygiene is still the No. 1 thing we can do to stop cross-contamination, but we asked, ‘What else can we do to lower HAI rates?’ UV disinfection gives us the opportunity to enhance our disinfection efforts,” Henderson says.
Sodexo invested in bringing the technology to the Sharp organization in partnership to reduce the risk of HAIs and protect the health of patients, Henderson says, as an additional precautionary step to prevent the spread of droplet, airborne or contact pathogens. And even though the technology adds 10–15 minutes to room processing times, Henderson believes the effectiveness of the technology in helping to reduce HAIs far outweighs the time it takes to use the equipment.
“When the room has been cleaned, depending on the size, we do a mapping and put the unit in the locations we’ve designated. We put up the arms of the bed, close the curtains and make sure everything is exposed to the UV light in each of the locations,” Henderson says, adding that the UV light is also wheeled into bathrooms and the door is closed while the patient room is being disinfected by the ES associate.
Henderson views the process as one more significant tool to help close the loop on the institution’s infection prevention efforts. He says he’s continually evaluating technologies and equipment to improve performance and patient safety.
Recently, he began exploring a company that makes UV overhead lighting systems to kill bacteria. It’s still early in the technology’s development, but he plans to follow its progress. The medical center also has purchased antimicrobial, recyclable curtains to reduce opportunities for cross-contamination. In addition, the organization is focused on automated, touch-free soap and paper towel dispensers. Finally, the ES team routinely measures cleaning thoroughness of high-touch objects in patient rooms with fluorescent marking gel.
Measuring cleaning impact
Linda Homan, R.N., CIC, senior manager of clinical and professional service at Ecolab Healthcare, reports that growing numbers of hospitals are taking a harder look at measuring cleaning effectiveness.
Ecolab’s EnCompass program helps hospitals to monitor and report data on thoroughness of cleaning with the goal of improving outcomes and reducing HAIs. The company issued its first EnCompass customer benchmark report in 2012. The data included results of cleaning thoroughness on more than 1 million high-touch objects. Since the first report was issued, Homan reports, the data on the number of high-touch cleaning surfaces evaluated has increased more than threefold, and more than 300 hospitals now participate in the program.
“The high-touch objects found to be cleaned most often in the most recent report included the toilet seat and the toilet flush handle. This shows there is a focus on the critical high-touch objects to help prevent the spread of C. difficile,” Homan says. “Interestingly, the high-touch objects found to be the least cleaned in the initial report — the patient room light switch and bathroom doorknob — were reported to have the most improvement in terms of frequency of cleaning when compared with data in the initial report. This shows that when hospitals have access to this type of performance data, they are better able to focus efforts on areas needing improvement.”
Of course, hospitals are focusing on more than just the most sophisticated new technologies to improve performance. May notes that floor cleaning equipment that can strip a floor without chemicals and without damaging the flooring offer inherent environmental and efficiency benefits.
“The other side of patient safety is that there is really good technology today in automatic floor scrubbers that leave hallway floors dry. You can use them to maintain hallways even during the day. They’re so quiet and, in a lot of cases, they are battery-operated,” May says.
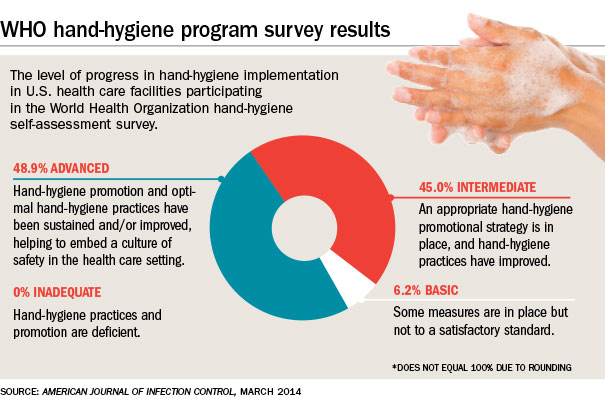
Finally, many experts believe there will be continued adoption of automated systems to dispense hand-hygiene products and to monitor compliance of hand hygiene throughout facilities. The use of real-time locating systems, radio-frequency identification technology and other systems appear to be gaining momentum.
“There’s absolutely no doubt there will be more focus on hand hygiene. You’ve got Enterovirus, D60A, Ebola virus — a lot of areas in which hand hygiene is singularly important,” May says.
is the associate publisher of Health Facilities Management.