IN BRIEF |
| • Health care organizations are shifting their care to team-based ambulatory models. •To support this trend, ambulatory facilities must be designed to accommodate these teams while still providing patient privacy. •Training also is essential if clinical staff are to get the most out of these new facilities. |
As health care systems shift their care models to be more responsive to patient-centered care and to support population health more effectively, ambulatory care teams need to be positioned to operate efficiently and effectively. In response to health care reform, anticipated physician and nurse shortages, and the development of patient-centric care models, team-based care is becoming more prevalent.
The transition to multidisciplinary, team-based care models requires all health professionals to work together in more innovative ways by establishing new lines of collaboration, communication and cooperation to serve patient needs better.
While these major care delivery changes are underway, there is also an increased focus on how the physical environment in outpatient settings can drive down costs. Maximizing utilization of revenue-generating spaces while minimizing the amount of space dedicated to nonrevenue-generating activities is one of the most straightforward ways that programming and planning can help to reduce costs.
New ambulatory spaces
Several attributes are critical to the success of the new ambulatory workplace. Care teams need to work together, have conversations, document notes and make phone calls within close proximity to the points of care. However, they also need space to allow for privacy and focused work.
Operationally, private physician offices in clinical spaces are increasingly seen as obsolete. Many organizations are recognizing the lost efficiency and potential lost revenue from using valuable hospital real estate for faculty and administrative purposes.
 For example, the new University of Minnesota Health (UMN Health) Clinics and Surgery Center in Minneapolis, scheduled to open this month, has been designed around the premise that workers in the building, with few exceptions, do not require a full-time, dedicated workplace. As a result, various environments have been created to enable activities to occur wherever and whenever they are needed. This is an open and flexible workplace with a high priority placed on caregiver collaboration.
For example, the new University of Minnesota Health (UMN Health) Clinics and Surgery Center in Minneapolis, scheduled to open this month, has been designed around the premise that workers in the building, with few exceptions, do not require a full-time, dedicated workplace. As a result, various environments have been created to enable activities to occur wherever and whenever they are needed. This is an open and flexible workplace with a high priority placed on caregiver collaboration.
Similarly, construction of the new Froedtert & Medical College of Wisconsin (MCW) Center for Advanced Care in Wauwatosa provided an opportunity to start transitioning physician office space off campus. While clinical and faculty office space historically has been located throughout the hospital, ambulatory growth requires that hospital facility space be used to its highest potential in support of the clinical enterprise. So, MCW decided to move a majority of faculty office spaces into a professional office building (POB), currently under development on the MCW campus. In the new Center for Advanced Care, minimal private offices are provided for clinic administration, and open-office work rooms have been introduced as an alternative.
You may also like |
| Eight ambulatory models of care |
| New generation of ambulatory care facilities |
| New York leads wave of ambulatory care construction |
| |
For some time, workplace typologies in corporate environments have utilized strategies to support a mobile workforce and collaborative work environments while maximizing the use of technology. These workplace design strategies are now taking hold in health care. Typically, both in-clinic and out-of-clinic activity must be accounted when developing alternatives to private office settings.
In-clinic activity. Spaces that facilitate in-clinic activity are potentially the most difficult workspaces to design because they need to accommodate many different functions. Input from many users is required to understand the ideal location of work spaces in relation to the exam rooms, as well as the configurations and options that should be available to workers in these spaces to accomplish different types of tasks.
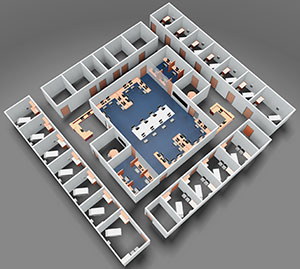
At the UMN Health Clinics and Surgery Center, collaboration spaces are located in the middle of each clinic module and used by the care and research teams while they are in the clinic seeing patients. These are spaces where work related to patient care, including teaching, research, treatment plans and interprofessional collaboration, is conducted. The environment is designed to support a variety of activities, including collaborating in multidisciplinary teams, reviewing and editing patient records, discussing specific cases and teaching residents. Patient privacy is protected by doors. The spaces are designed to permit the flow of caregivers between exam rooms and are centrally located to enable such interactions.
Each collaboration space is identically configured with furniture solutions based on a 42-inch wide module. Within a given collaboration space, there are fixed seated-height workstations as well as height-adjustable workstations to accommodate worker preference. Computer monitors are mounted to adjustable arms, and overhead shelves house shared materials. LED lighting is provided on dimmers, and task lighting is provided at each workstation. Additionally, each collaboration space has a printer cabinet.
At the Froedtert & MCW Center for Advanced Care, which opened in October, multiple work rooms centrally located in each of the facility’s six clinics accommodate faculty and staff. These spaces position staff in the hub of clinic activity. This central location creates shorter travel distances for staff and quicker access to patients. The work rooms offer shared workstations for staff while they are in the clinic. The workstations are not assigned or dedicated to any single person. They also utilize modular furniture to promote flexibility to accommodate the needs of staff in a particular clinic as it evolves over time.
While the work rooms vary in size and shape, each is highly flexible and includes different zones to support the different activities that need to take place:
• Stations located immediately outside the work rooms often are reserved for medical assistants who monitor activity inside and outside the clinics, helping to quickly locate clinical staff as needed and facilitate patient flow through the clinic.
• Inside the work rooms, conferencing areas focused around large, wall-hung monitors create teaming spaces for faculty and staff to discuss patient cases and collaborate as needed.
• Workstations without divider panels around the perimeter of the work rooms can be used for general clinical activities such as patient charting and diagnostic review.
• Segregated areas contain workstations with divider panels between them and can be used by staff to make phone calls or perform dictation.
• Physicians are permitted to use these areas depending on their preference, need to collaborate or need for speech privacy.
Additionally, each zone has adjustable lighting and temperature controls that can be altered by the users based on their activity. For example, a space used by a nurse practitioner may be fully illuminated to support charting and phone calls, while a physician work area may be dimmer to allow for imaging review between cases.
Out-of-clinic activity. Just as important as supporting in-clinic functions are the spaces that support out-of-clinic functions. These spaces provide areas for respite, informal meetings or work. At the Froedtert & MCW Center for Advanced Care, the centralized work rooms are designed to support both in- and out-of-clinic work. Additionally, shared locker rooms and staff lounges provide space for personal item storage and staff respite.
Finally, the new POB under development will be fully accessible by bridge to the hospital buildings on campus, so retreating to private offices also will be an option.
At UMN Health Clinics and Surgery Center, the staff lounges on each floor are vertically connected, promoting a sense of community within the building. These spaces are designed with flexibility to host large staff meetings and also to serve as formal conference rooms. The staff lounges allow for interactions with others who work in the building that otherwise may not occur, serving to break down silos and promote a collaborative environment.
In the same building, touch-down spaces that wrap the building’s exterior create access to daylight and views. These spaces are used by the care and research teams as well as other support staff to conduct quiet, focused work that is done outside of the clinic, such as after-hours charting or dictation, patient follow-up and phone calls. These spaces support both privacy and communication and are flexible, accommodating a wide range of activities. Personal storage lockers are provided that allow for backpacks and other personal items to be kept close at hand. The touch-down workstations follow the same 42-inch workstation module as that of the collaboration spaces, providing maximum flexibility for the facility.
Transition planning
For many organizations, emerging care delivery models that depend on redefining clinician roles are in conflict with the organization’s traditional culture, making change management challenging. Any time a move occurs, and in particular one with radical change in operations, a transition plan is a necessary component to manage the change. Too often, it is overlooked or starts too late in the process. There are several activities to consider when implementing a transition plan.
A communication and adaptation plan should include various written and formal presentations relevant to the new workplace design. It serves as an orientation and educational forum for all staff. The purpose of the plan is to provide a bridge for staff to adopt and adapt to the future state workplace model. The plan should include specific ideas for early adoption, allowing staff to enter the new building prepared for what to expect.
A workplace orientation plan includes presentations of the new workplace design to orient staff about how the furniture and technology solutions support the overall building intent. Mock-ups of various workplaces can be used to simulate activities and gather valuable input during the design process. As part of this process for the UMN Health Clinics and Surgery Center, a collaboration space was mocked up, and staff members were invited to visit and complete a survey of their preferences related to layout, furniture and amenities. The survey provided a better understanding of current workflow and needs. It also gave staff a preview of some of the changes to come.
An implementation plan serves to define the overall structure and schedule for implementing the workshops and educational events. The plan should include a roster of those who would be engaged as well as the type of activities recommended to occur.
Creating a users’ guide is a helpful way to assist employees with the features and amenities of their new workplaces and the building.
A post-move process should be defined to address any user-requested changes. It is often beneficial to have a cooling-off period to allow staff to adjust to the new workplace before making any changes. A formal process to manage requests and accept changes is an important component of any change-management plan.
Measuring impact
For emerging ambulatory workplaces to be the most effective, they must be paired with operational changes that have been communicated to staff and implemented in an organized fashion.
The new environments should be flexible enough to help staff transition to new operational protocols. For example, in open work areas, furniture can be used to create more private conditions during the first stages of a transition.
As staff become more comfortable with their new environments, changes that accommodate greater flexibility can be made as necessary. Working with administration and end users is critical to success for these massive change-management efforts.
Finally, designers must continually measure the impact of emerging solutions. Because it is unlikely that there will be a return to private office settings in the near future, designers must help health organizations to figure out a new ambulatory workplace that meets their needs.
Jocelyn Stroupe, CHID, EDAC, IIDA, ASID, is principal at CannonDesign, Chicago. She can be reached at jstroupe@cannondesign.com.
Design considerations for in-clinic work spaces
Designing flexible, adaptable in-clinic work spaces with few dedicated workstations presents several challenges. Here are a few things to consider in the design of collaborative work areas:
• Storage of personal belongings. Staff members often need more than one option for personal storage. For instance, the University of Minnesota Health (UMN Health) Clinics and Surgery Center in Minneapolis addresses this with two types of lockers. The building is designed with locker rooms at points of entry on each floor. While these are good for coats and boots, they are farther from where employees spend their day. Consequently, smaller personal lockers for backpacks or purses were placed in open touch-down areas and serve as a way to separate the area visually. All storage components in the building — lockers, file cabinets, storage cabinets — are designed with a programmable locking system that eliminates keys and allows for multiple users.
• Storage of clinical materials. Within in-clinic work spaces, storage for materials used while in the clinic are required. These include paper forms and literature as well as anatomical models used to teach residents and patients. Storage cabinets and shelving over the workstations may need to be provided.
• Flexible and adaptable workstations. The typical workstation should be designed to be minimal and universal, comprising a kit of parts with interchangeable components. A combination of fixed seated-height and adjustable-height workstations should be used to allow the workstation to adapt to multiple users. Accessories to support specific work requirements should be identified and added on an as-needed basis.
• Privacy and sound control. With the advent of open, collaborative spaces close to the point of care, concern for impact on the patient experience should be considered along with strategies that promote control and patient privacy.
• Realistic technology adoption. Technology is evolving at a rapid pace, making it difficult to determine the impact on an organization’s care model in both the immediate and more distant future. More technology sooner is not always better, particularly if a given technology does not add appropriate value. New technologies should be considered through the lens of their operational, financial and facilities implications before an investment is made.