Monthly tests under no-flow for electric motor fire pumps is proposed revised language but not a new requirement.
An attentive audience of health facilities professionals filled a ballroom for nearly three hours at July’s American Society for Healthcare Engineering (ASHE) Annual Conference and Technical Exhibition in Denver as they learned about sweeping changes to the Joint Commission standards and survey process.
The presentation by George Mills, director of engineering for the Joint Commission, expanded upon changes previously announced in Joint Commission publications and at the National Fire Protection Association’s (NFPA’s) Conference & Expo in June. Other changes were newly announced or clarified.
You may also like |
| ASHE, Joint Commission collaborate on portal |
| Joint Commission announces major changes at ASHE conference |
| ASHE coordinates advocacy efforts for design and operations |
|
|
They included changes in the Environment of Care (EC) and Life Safety (LS) standards as well as in survey procedures, statements of conditions and scoring.
Major changes
Major changes undertaken by the Joint Commission include the following:
Clarifications. Prior to the survey, hospitals will need to complete a required documentation checklist and sign an attestation to its accuracy. An EC/LS pre-survey checklist also will be required. Given the attestation, documents that were not available at survey will not be accepted for clarification post-survey. Surveyors will require all documentation to be available during the designated document review session and likely will not have time to review them if they are not produced until later during the survey.
Insofar as possible, clarifications will be addressed in real time via a phone call with the Joint Commission’s Standards Interpretation Group for any difference of opinion between the organization and the surveyor. Such a call should be requested by the organization, if necessary. The only clarification that will be made following the survey is for those findings that the organization believes have been made in error and are not document-
related. No documentation clarification requests will be accepted post-survey.
Standards. The 2017 standards will reflect deletion of the tags for A and C standards, direct and indirect impact, measures of success and risk, as have been previously announced. However, the tags for documentation required (Circle D) and situational decision rules (Triangle 2) will remain. This will make all standards equal in terms of surveyor evaluation; there will be no identified opportunities for improvement on the survey report, and surveyors will operate under a “see it-cite it” methodology.
By removing A and C classifications of the elements of performance (EPs), the question of preventive maintenance completion rates remains. Previously the category A EPs needed to have a 100 percent completion rate, with category C EPs requiring a minimum of 90 percent completion. This will be addressed with the addition of new notes regarding preventive maintenance in both the medical equipment and utility standards. These notes will require a 100 percent completion rate for high-risk equipment and components (including infection control components for utilities), whether or not under an alternative equipment maintenance strategy. Non-high-risk equipment in both standards will carry a note of an expected 90 percent preventive maintenance completion rate. So this expectation will be the same as always.
The following changes will be made to the standards in the future (numbers are subject to change):
- Environment of Care chapter: 13 new EPs; 31 modifications of existing elements; and one additional deletion.
- Life Safety chapter: 21 new EPs; 32 modifications; and five deletions.
These follow several deletions that went into effect on July 1 as part of the Joint Commission’s Project REFRESH.
Proposed standards modifications are currently being reviewed by the Centers for Medicare & Medicaid Services (CMS). The CMS K-tags are being expanded from 29 to 48 pages to accommodate the adoption of the 2012 edition of the Life Safety Code. Accordingly, additional new EPs are anticipated.
Among the proposed standards modifications are the following issues, with exact language remaining to be determined:
- EC.02.02.01: Waste anesthetic gas and lab rooftop discharge signage.
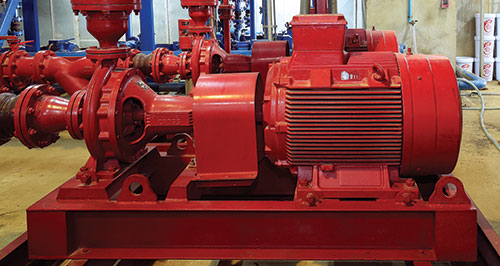
- EC.02.03.05: Definitions of supervisory signals; electromagnetic-releasing devices clarified as door-releasing devices; monthly fire pump test under no-flow for electric motor fire pumps; fire extinguisher access, monthly inspections and annual maintenance; annual door maintenance; and inventory of all devices.
- EC.02.05.01: Identification of controls to be labeled for emergency shutdown; noncritical area ventilation, temperature, humidity and pressure relationships; medical gas storage and manifold rooms; and emergency power supply system environment and maintenance.
- EC.02.05.03: Application of NFPA 99 (2012) if Type 1 or 3 essential electrical systems upgraded since 1983; essential electrical systems have life safety, critical and equipment branches; emergency power transfer within 10 seconds; and generator location requirements.
- EC.02.05.05: During repairs or maintenance (not just construction or renovation), a process is in place to manage air quality, infection control, utilities, noise, odor, dust, vibration and other hazards; high-risk and infection control preventive maintenance completion rates at 100 percent; and non-high-risk completion rate at 90 percent.
- EC.02.05.07: Weekly inspection of the emergency power supply system; during monthly load test, the generator cool-down period is not part of the 30-minute run time; and annual load bank requirements reduced to 90 minutes.
- EC.02.05.09: Policy on gas cylinder handling, storage and labeling; prohibition of transfilling in patient care compartments; emergency oxygen supply connections; clarification of testing of the piped medical gas system; and bulk oxygen systems in locked enclosure and appropriate signage.
- LS.01.01.01: Building assessments for Life Safety Code compliance; current and accurate life safety drawings; 60 days to correct deficiencies or a time-limited waiver; and existing features of fire protection that are obvious to the public must be maintained or removed.
- LS.01.02.01: Evacuation or fire watch is required when fire alarm system is compromised for four out of 24 hours or sprinkler system is compromised for 10 out of 24 hours; and Interim Life Safety Measures (ILSM) elements of performance reordered.
- LS.02.01.10: Added reference to NFPA 101 (2012) Chapter 43 for building rehabilitation; fire protection ratings for openings; blocking or wedging fire doors prohibited; and removal of requirement on unapproved protective plates.
- LS.02.01.20: Compliant locking based on security; exit enclosures not used for anything not supporting the enclosure; notes on wheeled equipment and fixed furnishings; subdivision and separation of suites; second exits from suites; and larger size of sleeping suites.
- LS.02.01.30: Hazardous areas EP revised; limited cooking; alcohol-based hand rub EP added; clarification of corridor separations in new and existing construction; sleeping rooms have windows; and window sill height in new construction at 36 inches.
- LS.02.01.34: Ceiling membrane must be intact.
- LS.02.01.35: Escutcheon plates must be installed; availability of six spare sprinkler heads; sprinkler protection in closets; fire extinguisher mounting; and a Class K extinguisher placard requirement.
- LS.02.01.70: “No Smoking” signage in medical gas storage areas; ash trays and ash containers in indoor smoking areas; and 96-gallon containers for clean waste.
Because these EPs are proposed by the Joint Commission, and are being vetted by CMS, it is anticipated that the 2017 Joint Commission standards will not be published until early 2017.
Statement of conditions. Perhaps the most impactful changes involve the Statement of Conditions. The Joint Commission has been working with CMS for some time on CMS-mandated changes and now they are here.
CMS, per 42 CFR 488.28(d), requires compliance with identified Life Safety Code deficiencies within 60 days, however, the time may be extended for significant issues. The Joint Commission now will comply with this requirement, making the plan for improvement (PFI) optional effective Aug. 1, 2016. It still will be available for use as a tool for the management of deficiencies within the organization. This tool will not be reviewed by the surveyor and open PFIs will not be printed on the survey report. Open PFIs listed on previous survey reports will not be reviewed by surveyors.
Any deficiencies identified during the survey will be cited as recommendations for improvement (RFI) with a required 60-day completion date. These deficiencies will be entered on a survey-related PFI (SPFI), which will also feature a dropdown menu to identify which ILSM will be implemented for each deficiency. This process will be monitored electronically. Failure to complete the SPFIs within the time frame can generate a decision of Accreditation with Follow-Up Survey.
There is an option to apply for a time-limited waiver (TLW) if extended time is needed. The TLW must be requested within 45 days of survey, so that it can be cleared through both the Joint Commission and CMS within the 60-day period. TLWs for non-deemed status organizations will be approved only by the Joint Commission. Upon approval of the waiver, a receipt will be issued, and that receipt may be presented to a surveyor during any follow-up survey. The requested scheduled completion date must be considered as a “not to exceed” date; there will be no grace period and no extensions on the TLWs. Time requests for TLWs must be kept “reasonable.” To accommodate this process, new and revised EPs have been proposed under LS.01.01.01:
- EP 1: “The organization assigns an individual to assess compliance with the Life Safety Code and manage the Statement of Conditions when addressing survey-related deficiencies.”
- EP 2: “In time frames defined by the hospital, the hospital performs a building assessment to determine compliance with the Life Safety chapter.”
- EP 3: “When the hospital plans to resolve a deficiency through an SPFI, the hospital meets the 60-day time frames. NOTE: If the corrective action will exceed the 60-day time frame, the organization must request a TLW.”
Where previously, hospitals have completed the Basic Building Information (BBI) and the PFI, the new documents required will be the SPFI and the TLW. The information previously entered into the BBI now will be captured during the survey application process.
Historically, identified deficiencies for inaccessible dampers have been added to the PFI with six-year completion dates when the space was renovated and extensions were granted. Under the new requirements, these dampers must be resolved by working with the state fire marshal or accessibility must be created. Requests for equivalencies only will be considered if they are related to a survey finding, not proactively.
Scoring changes. The Survey Analysis for Evaluating Risk matrix, as announced in the Joint Commission Resources’ Environment of Care News newsletter, will score deficiencies based on the likelihood of harm and the scope of the issue in question. This method will make distinctions in various aspects of compliance.
For example, “EC.02.03.05, maintenance, testing, and inspection of features of fire protection,” has both a test-performance and a documentation component. If an organization has not performed a test, that will be evaluated with a higher likelihood of harm than disorganized or incomplete documentation.
Findings in the higher-level boxes on the matrix will require answering questions about sustainment of and responsibility for the corrective action submitted as part of the organization’s evidence of standards compliance post-survey. Any issues scored in the uppermost box as “immediate threat to life” will require expedited correction.
All survey findings, with the exception of those indicated as “immediate threat to life,” will have a 60-day period in which to submit evidence of standards compliance.
Moving forward
The changes are extensive but proactively managing Life Safety Code compliance will be key to success as health facilities professionals strive to improve performance and patient safety.
Susan B. McLaughlin, FASHE, CHFM, CHSP, is managing director of MSL Healthcare Consulting Inc., Barrington, Ill., and a former associate director of standards interpretation at the Joint Commission. She can be reached at smclaughlin@mslhealthcare.com.