For most hospitals, capturing controlled-substance waste is a challenging process that poses high risks to health care networks and their stakeholders.
The growing number and increasing use of pharmaceuticals throughout widely dispersed health care networks has heightened the urgency for hospitals to manage controlled-substance waste more safely and effectively. Four factors make this especially challenging:
- Many health care facilities lack formal processes for the proper disposal of controlled-substance waste that are effective in preventing diversion.
- Hospitals must comply with complicated, confusing and costly regulations from different agencies regarding waste disposal.
- The abuse of controlled substances is skyrocketing, which increases the risks for diversion (i.e., used or expired drugs taken by unauthorized persons).
- Flushing, the most common current practice for controlled-substance waste disposal, is costly due to staff time and can harm the environment.
Also in this article |
| Proactive drug disposal strategy |
|
|
A 2012 national survey on drug use found that almost twice as many Americans abused pharmaceutical controlled substances than the combined number of users of cocaine, hallucinogens, heroin and inhalants. It also estimated that nearly 110 Americans die every day from drug-related overdoses, and about half of those overdoses were related to opioids, a class of drugs that includes prescription painkillers and heroin, according to a Sept. 8, 2014, notice by the Drug Enforcement Administration (DEA).
A new responsibility
For most hospitals, capturing controlled-substance waste is a challenging process that poses high risks to health care networks and their stakeholders, particularly in regard to regulatory compliance, patient safety and reputation management. Pharmacy directors and other health facilities professionals are now responsible for ensuring that leftover or unused drugs and drug waste are not taken or used by anyone other than the intended patient.
As the opioid epidemic continues to rise and regulators clamp down on prescribing requirements, hospitals are becoming bigger targets for diversion of controlled substances.
Detecting diversions, however, can be difficult because people have numerous opportunities to access these medications throughout the hospital and at various stages of patient care and waste disposal. The increasing prevalence of drug abuse heightens the risk that clinicians or staff could be affected by diverted controlled substances while caring for patients.
Workers who abuse controlled substances while at the hospital will have impaired judgment and skills, further increasing the risk that their actions could have an adverse effect on patients.
Confusing regulations
The first challenge in developing strategies for the proper handling and disposal of controlled substances is to understand the regulatory requirements. A 2014 regulation by the DEA states that “the controlled substance dispensed for immediate administration … remains under the custody and control of the registered institution even if the substance is not fully exhausted (drug wastage) ... such remaining substance must be properly recorded, stored and destroyed in accordance with DEA regulations and all applicable federal, state, tribal and local laws and regulations.”
The DEA’s Disposal of Controlled Substances final rule in 2014 remained unclear to many hospitals, prompting a “Dear Practitioner” letter that emphasizes the important distinction between practitioner inventory and pharmaceutical wastage. It also notes that after a prefilled syringe or single-dose vial is administered to a patient, any remaining substance is not required to be destroyed. However, although part 1307 in the final rule does not apply to pharmaceutical wastage, the DEA “strongly encourages all practitioners to continue to adhere to security controls and procedures that ensure pharmaceutical wastage is not diverted.”
In a survey on pharmaceutical waste-management regulatory challenges published by Pharmacy, Purchasing & Products magazine in February, hospital pharmacy professionals cited the complexity of regulations as their No. 1 concern, closely followed by staff training. Specifically unclear regulations for controlled substances and lack of in-house expertise are also drivers for waste stream-management partnerships.
In practice, many hospitals dispose of excess medications by flushing them or placing down a drain, though the DEA requires two witnesses for the disposal and documentation of the event. Although flushing is still allowed under the new rule, hospital and pharmacy leaders should be aware that, on average, about 5 percent of pharmaceutical formularies are drugs regulated under the Environmental Protection Agency’s (EPA's) Resource Conservation and Recovery Act (RCRA) as hazardous materials and less than 1 percent of most formularies consist of controlled substances, some RCRA-hazardous. The EPA can levy penalties up to $37,500 a day for each violation.
Controlled substances also are subject to DEA regulations for packaging, inventory and transport, and those considered hazardous waste must follow Department of Transportation (DOT) hazard classification requirements. Practitioners whose primary focus is patient care are finding it increasingly difficult to stay current with and adhere to all these evolving regulations.
Diversion prevention
To comply with these regulations and, more importantly, minimize the growing risk of drug diversion in the workplace, hospitals need to initiate more effective practices for managing the disposal of controlled-substance waste. Ideally, such disposal programs should:
- Be easy for everyone to use and understand.
- Prevent diversion by immediately deactivating controlled-substance waste and making it irretrievable.
- Be cost effective and adaptable to meet a hospital’s specific needs regarding waste volume, current operating practices and space limitations and configurations.
- Offer multiple levels of safety and security for disposal of tablets, capsules, liquids and patches.
- Incinerate all drug waste to keep it out of water systems and landfills.
- Provide a comprehensive solution that includes personnel training and reports.
Although the DEA does not yet mandate hospitals to have formal processes for the disposal of controlled-substance waste, many expect it to do so in the near future. In fact, a number of hospitals [see sidebar, Page 46] have taken steps to prepare for this by implementing new waste-disposal solutions on the floors.
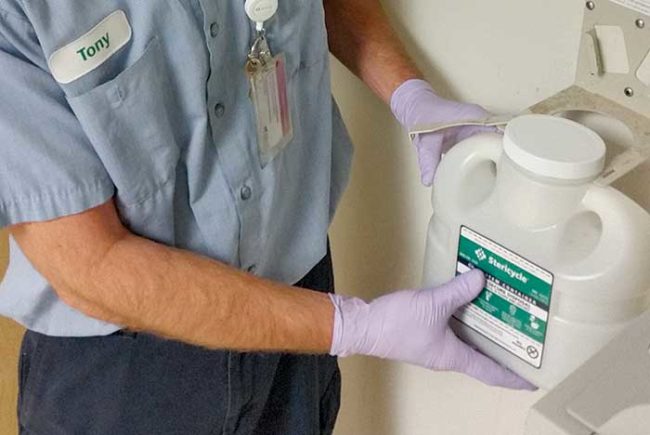
These systems can be a safe and secure way to dispose of all controlled-substance waste generated on the floors or in operating rooms. Hospitals using these systems consider it diversion-resistant in many ways.
For any facility considering the use of containers for the disposal of controlled substances, it’s critically important for staff members to understand how these containers can prevent diversion.
They also need to be trained on how to use the right size and type for all pharmaceutical waste containers and other disposal procedures.
Training should be documented and provided as often as needed to meet regulatory requirements. For example, the DOT requires employees to be trained within 90 days of taking on a task and every three years thereafter.
An integral need
Hospitals today have large formularies that typically range between 1,400 and 4,000 drugs and face intensifying scrutiny regarding the waste practices for these pharmaceuticals.
Health care leaders are starting to build comprehensive programs to address challenges related to compliance, safety, drug diversion and the amount of medications in public water supplies.
Because hospital pharmacists have identified the lack of in-house expertise as one of their top compliance-related challenges, many of these leaders seek counsel and support from companies experienced in all aspects of pharmaceutical waste management.
Although managing this waste stream in specifically labeled, controlled-substance containers is new to most hospitals, this needs to become an integral part of any health care facility’s pharmaceutical waste-management initiative.
Gerry van Domelen is senior manager of Rx Waste Compliance for Stericycle, Lake Forest, Ill.