
Environmental services personnel play a key role in helping the health care team by reliably maintaining a safe, clean care environment and projecting friendliness and caring during routine interactions with patients.
To be successful in today’s rapidly evolving, consumer-driven health care marketplace, hospitals and health systems must aggressively protect and promote their brand by maximizing the value of the care experience in the eyes of their patients.
This requires identifying the outcomes that matter to patients and engaging every member of the health care team in the ongoing mission to improve those outcomes.
Also in this article |
| How every ES team member can make a difference |
|
|
As is the case for every member of the care team, the contribution of environmental services (ES) departments to the patient centricity of the care experience — and, by extension, to the nurturance of brand loyalty — is unique and invaluable.
Certainly, environmental hygiene is critical to patient safety: Proper and thorough cleaning prevents the spread of infection, waste removal from patient rooms and common areas reduces the risk of patient falls, and waste segregation minimizes pathogenic cross-contamination and transmission of microorganisms.
Above and beyond the cleanliness of a hospital, however, are patients’ perceptions of cleanliness, which affect the hospital’s brand and reputation.
New research emerging from a strategic partnership between Press Ganey Associates Inc., South Bend, Ind., and Compass One Healthcare, through its specialty companies Crothall Healthcare and Morrison Healthcare, suggests that patients’ perceptions of environmental factors are correlated with specific safety, quality and experience outcomes and are an essential variable in the improvement equation.
Specifically, the data show correlations between patients’ perceptions of room cleanliness and the risk of health care-associated infections (HAIs), scores on the HCAHPS "Recommend the Hospital" item and on teamwork indicators.
These data, particularly the link between patients’ perceptions of cleanliness and the risk of HAIs, indicate that patients know clean when they see it. Additionally, the fact that patients are more likely to recommend a hospital they perceive to be clean suggests that cleanliness is an outcome that matters to them and is an important improvement target. For this reason, ES departments should:
- Understand, communicate and take pride in the important role they play in patient safety and clinical quality improvement efforts;
- Consistently assess and improve cleaning methods and procedures to ensure a pathogen-free environment and prevent the transmission of bacteria, viruses and other sources of infection;
- Continually employ audit practices that measure the actual cleanliness of high-touch surfaces;
- Promote staff accountability for cleanliness and encourage self-audit procedures.
Fulfilling expectations
Health care is a team sport, making effective collaboration among staff members who are directly or indirectly involved in delivering patient care a strategic necessity. Each member contributes to the whole of the enterprise in a meaningful and valuable way.
You may also like |
| ES department helps improve HCAHPS scores |
| Improving ES customer service |
| ES patient satisfaction role goes beyond cleanliness |
|
|
ES personnel play a key role in helping the health care team to fulfill these expectations by reliably maintaining a safe, clean care environment; projecting friendliness and caring during routine interactions with patients and families; and communicating and collaborating with the health care team to ensure that patients’ needs are being met.
Patients are not merely impressed by shiny floors, clean bathrooms and clutter-free common areas. They expect this level of cleanliness, and they perceive it as a minimum requirement for safe, high-quality care.
With heightened concerns and awareness regarding HAIs, patients and family members understand why a sanitary environment is important to their healing and recovery, and survey feedback about their perceptions of cleanliness can serve as an early warning system for HAIs.
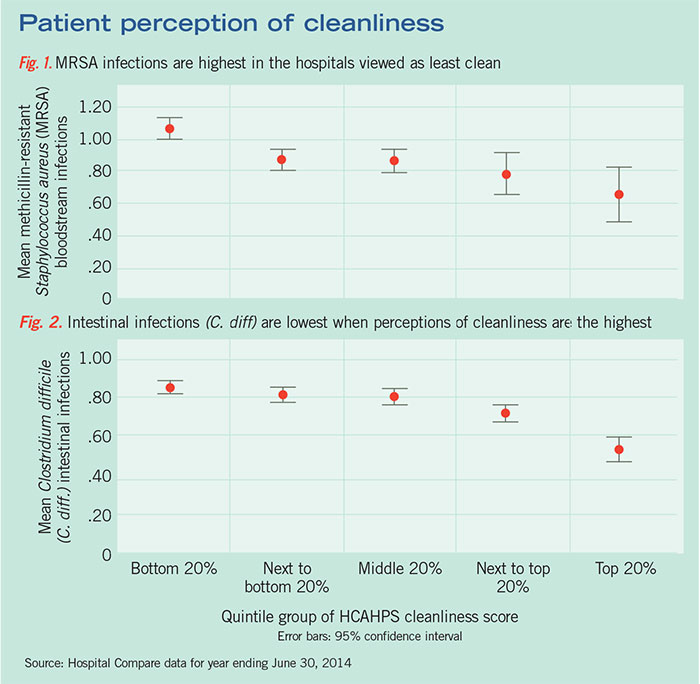
The results of an analysis of HCAHPS patient experience of care metrics and the incidence of specific HAIs as reported to the Centers for Medicare & Medicaid Services (CMS) for the year ending June 30, 2014, show a relationship between patients’ perceptions of cleanliness and HAIs (Figures 1 and 2). Specifically, the data show a clear correlation between patients’ perceptions of cleanliness as measured by the HCAHPS question “How often were your room and bathroom kept clean?” and the incidence of methicillin-resistant Staphylococcus aureus and Clostridium difficile.
Hospitals that scored in the highest quintile for cleanliness had, on average, the lowest number of reported infections. Similarly, hospitals in which patients reported lower cleanliness scores tended toward higher infection rates.
These findings have broad implications for patients’ perceptions of their hospital stays. In qualitative interviews and focus groups, patients often described their assessment of cleanliness as an important barometer of the overall quality of care. “If they can’t keep the hospital clean, what other things that I can’t see might also be neglected?” was a common sentiment expressed by patients.
The strong correlation between patients’ perceptions of cleanliness and HAI rates supports the idea that patients can judge actual cleanliness — a finding that validates the important role ES staff members play in patients' evaluations of their hospital experience.
The relationship also represents an important improvement target. Hospitals can boost outcomes on both measures by:
• Making the consistent assessment and improvement of cleaning methods and procedures an operational priority to ensure a sanitary environment and prevent the spread of infection;
• Recognizing the important role ES staff members play in patient safety and clinical quality improvement efforts;
• Implementing ongoing audit practices to evaluate cleanliness and fidelity to established best practices.
Driving patient loyalty
If a patient’s perception of room cleanliness is correlated with a hospital’s overall HAI rate, it follows that it also affects the hospital’s overall reputation and, importantly, patient loyalty.
In a Chi-squared Automatic Interaction Detector analysis, an analytical technique that determines how variables best combine to explain the outcome of a dependent variable, researchers identified the factors that together explained the greatest variation in patients’ willingness to recommend an institution to friends and family, which is considered a proxy for patient loyalty.
The analysis showed that the third most influential question explaining patients’ willingness to recommend the hospital, behind the questions asking whether doctors and nurses listened carefully, was “How often were your room and bathroom kept clean?” Among patients who reported that nurses and doctors always listened well and the room was always kept clean, 90 percent of respondents would highly recommend the facility.
This analysis has significant implications for a better understanding of how the perception of cleanliness fits into a patient's decision when evaluating health care provider experiences. When patients feel they have been heard and their concerns have been understood, hospital cleanliness rises to the top of their additional concerns.
The connection between patients’ and families’ perceptions of cleanliness and their perceptions of a hospital’s reputation makes sense.
Patients expect hospitals to be clean, and while they are not always able to judge care delivery on the elements that medical professionals use, they utilize surrogate measures such as cleanliness to help them decide how well hospitals are doing.
Imagine the practical reality of these observations. When family members visit a loved one in the hospital, if the room and hallways appear cluttered or dirty, the expectation that the hospital is a sanitary place will be diminished, leaving the visitors to question how well the hospital performs in other areas.
For hospitals working to improve the actual and perceived cleanliness of the care environment, operational practices are central to these efforts. Decisions such as which cleaning agents are most effective in eliminating bacteria and how frequently “deep cleaning” should occur at times when the room is unoccupied are relatively straightforward.
In addition to these operational practices, patients’ perception of cleanliness is correlated with other patient experience factors. Among the HCAHPS survey domains, staff responsiveness and nurse communication are most highly correlated with perceptions of cleanliness.
These findings align with research in the literature that cites the importance of teamwork in delivering an exceptional patient experience, promoting a culture of safety and contributing to other quality metrics, including those related to the care environment.
Interviews with hospital leaders and front-line staff provide additional insights into why teamwork is so critical in improving cleanliness. Nursing, ES and other operational leaders often remark that it requires effort on the part of the entire team to improve cleanliness, including effective hand-sanitizing practices, appropriate disposal of medical waste and even the basic task of picking up after oneself.
Additionally, the communication with and support of ES staff members by clinical colleagues affects the way they view their work, their morale and their productivity.
Identifying a patient's perception of teamwork as a critical differentiator reinforces why it is important to ensure that everyone who directly or indirectly influences patient care has a key role in determining the quality of that care.
Previous studies have shown that teamwork indicators are among the most highly correlated with overall patient experience, and they represent an opportunity for improvement across departments.
The fact that ES staff members are geographically dispersed and spend the majority of their working hours isolated from their departmental colleagues presents unique challenges, but hospital leadership and departmental managers can help teams to overcome these challenges through the adoption of best practices, including:
• Making sure ES employees are recognized as important members of the department/unit where they primarily clean, not just the ES department. This can be achieved through the promotion of supportive, positive interactions with nurses and other clinical professionals with whom they interact daily.
• Involving the ES staff in regular departmental meetings, including huddles at the beginning of every shift, training and development sessions, and monthly staff meetings. This is critical to maintaining morale and keeping the team connected.
• Encouraging frequent rounding and observation on units by ES managers. Rounding with nursing and other ancillary services managers at least monthly demonstrates shared responsibility and models the power of constructive relationships to the front-line staff.
Clear correlation
The clear correlation between patients’ perceptions of cleanliness and multiple safety, quality and experience measures demonstrates that cleanliness is an outcome that matters to patients. It also influences patients’ overall perceptions of the care experience.
For these reasons, hospitals seeking to distinguish themselves from the competition should look for opportunities to help ES staff members understand how the physical environment can influence the patient experience, and they should offer support, education and resources to address deficiencies that might be obstacles on the journey to patient-centered excellence.
In this regard, hospital leaders and departmental managers should:
- Recognize and value ES workers as stakeholders in the delivery of safe, effective, high-quality care;
- Consistently identify and employ evidence-based guidance and practices in ES to optimize the cleanliness and perceived cleanliness of hospital rooms and common areas;
- Reinforce accountability for service excellence among the ES staff;
- Foster a culture of teamwork, communication and collaboration between the staff and the rest of the caregiving team.
By considering the people, processes and places that affect the patient experience, health care leaders can help their organizations to meet important performance goals, and build and sustain patient loyalty.
James Merlino, M.D., is president and chief medical officer of the strategic consulting division at Press Ganey Associates Inc., South Bend, Ind. He can be reached at jim.merlino@pressganey.com. This article is based on a white paper by Press Ganey and Compass One Healthcare titled "Environmental Services: Delivering on the Patient-Centered Promise."





