IES professionals should follow key steps to ensure that the UV technology is effective.
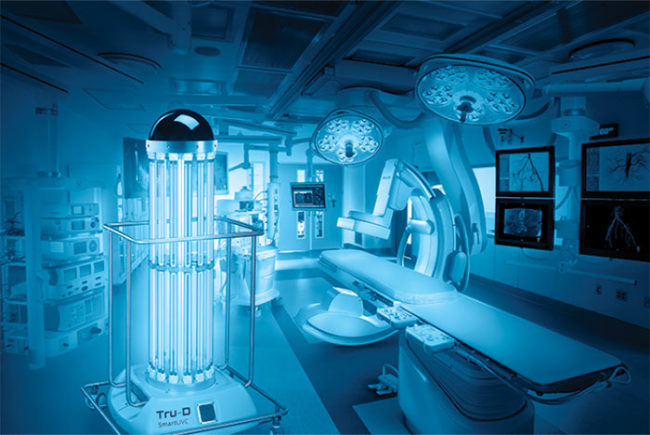
Environmental services (ES) professionals have new tools available to combat health care-associated infections (HAIs) by incorporating ultraviolet (UV) disinfecting technology into their cleaning protocol.
UV technology basically works by producing a high-intensity UV light that passes through the cell walls of bacteria, viruses and bacterial spores. The DNA, RNA and proteins inside the microorganism absorb this intense UV energy and the pathogens are destroyed.
You may also like |
| Automated disinfection systems help reduce HAIs |
| Focus intensifies on UV disinfection research |
| Hospitals turn to automation to aid in cleaning |
|
|
There are generally two types of UV systems available today — whole pulse xenon UV and continuous UV. Both types of systems are reliable, but are only effective if correctly introduced and incorporated into the ES department’s infection control plan.
Steps to follow
ES professionals should follow key steps to ensure that the UV technology being considered for purchase is effective in reducing the rate of HAIs in their health care facilities.
Failure to follow these steps can reduce and jeopardize the success of any UV technology implementation.
1. Acquire funding. UV technology is expensive, but the cost of HAIs to any medical facility can be enormous. ES professionals should speak with their infection control department to gather information on the annual expense of HAIs.
One major Midwest academic medical center recently determined that eliminating only four HAIs would pay for the cost of one UV device. This information should be shared with the finance department of the facility to provide valid documentation on how the UV equipment will save the institution HAI-related expenses.
A documented quick return on the investment will greatly enhance the ES department’s probability of securing the needed capital to complete the purchase.
The ES professional should speak with peers who are already using the UV technology to gather documented successes that demonstrate how using the technology reduces HAIs.
2. Conduct research. ES professionals should invite at least two UV technology companies to the facility to discuss and review the effectiveness of their equipment.
ES professionals also should ask for industry research results and customer reviews. Can companies demonstrate and verify success in reducing health care-associated Clostridium difficile and methicillin-resistant Staphylococcus aureus infections in the field? Will they provide a complete training of the staff? Will they be available to provide on-site support? Can data from the UV equipment be downloaded directly to the ES management staff for daily review?
The ease with which the ES professional can access utilization data from the UV device cannot be overly stressed. Ideally, ES professionals should be able to access the data from their desks.
ES professionals also should request names of current customers and contact them personally. They should see the current users about successes and failures and learn about staff buy-in to the UV process in their daily cleaning routines.
Supervisory staff, front-line staff, infection control professionals and nursing representatives should be involved in these initial discussions. Staff input and involvement from the start is critical and beneficial in ensuring a successful UV technology program.
Prior to making a decision, ES professionals should have the selected UV technology company representative provide a presentation to the facility’s infection control committee. Most facility infection control committees have representatives from nursing and other clinical areas.
It is important that members of the infection committee and medical staff understand and buy in to the new disinfection process.
3. Conduct training. After the company and UV equipment have been selected, a thorough training program is imperative. Every member of the ES department responsible for cleaning direct patient care areas must be trained thoroughly.
The ES professional should insist that the selected company invest the time and resources needed to familiarize the ES staff with the UV technology. Depending on the number of ES staff, one to two weeks of ES training and orientation may be required for a UV disinfection system. The training program should provide documentation that the ES employees understand the UV technology and have shown competence in using the technology in a patient care setting. ES staff need to have a strong sense of ownership in the new technology. Without their commitment and thorough training, the UV program will not be successful.
4. Implement trial period. Many ES departments first commit to purchasing only one or two UV devices. Further purchases will be premised on initial outcomes. HAIs must be reduced to justify a further expansion of the UV disinfection program.
The ES professional should meet with the infection control department to determine which patient care areas have the highest HAI rates. They should choose the patient areas where the UV technology will have the biggest impact and greatest chance of success. Once those patient areas have been selected, meetings with both the nursing and the ES staff assigned to these areas need to be undertaken. The scope of these meetings should include:
- When will the UV equipment be used? Typically, the UV disinfection equipment will be used after patient discharges. This technology cannot be used when the patient is present. The UV technology can be used only in rooms or areas that are not occupied.
- How will the new UV technology impact the patient admission process? The facility's occupancy level must be considered. If occupancy is high, delaying the admission process will have a negative impact on patient satisfaction and the facility’s financial bottom line. Typically, using the UV equipment during the patient room discharge cleaning process will increase the cleaning turnaround time by 10 to 15 minutes. A well-trained ES staff with nursing support will ensure that delays in the discharge process are minimal and will not impact the patient admission process.
- Can other areas of the patient unit benefit from using UV technology? The UV device may have limited use on the third shift. Many patient units have holding rooms for medical equipment and wheelchairs. Nursing staff can be trained to use the UV technology in these holding rooms when the device is not being used by the ES staff.
5. Update discharge cleaning protocols. The most important information to convey to the ES staff is that current cleaning protocols still must be used.
UV technology does not replace rigorous disinfection cleaning practices; it only improves the final outcome. All patient room surfaces still should be thoroughly disinfected, and patient safety practices must be followed.
The UV technology should not be considered a shortcut to a thoroughly disinfected room. For patient areas where the UV technology is to be used, ES professionals should follow this new process in the discharge cleaning protocols.
A sample update should include these additional steps:
- After a patient room has been prepared for cleaning (i.e., all equipment, waste and soiled linen removed), ES staff should bring the UV device and safety signage to the room. If the device is being used by another staff member, he or she should be asked to bring it to the room when finished.
- ES staff should set up the UV device’s safety signage outside the room. This will alert other staff not to enter the room while it is being used. ES professionals should enter their own assigned cleaning password on the device. This information will document when and where the UV device was used.
- ES staff should clean the patient room bathroom first. When the bathroom has been completed, the UV device can be placed in the bathroom, the bathroom door closed and the device activated.
- ES staff should complete the cleaning of the patient room, while the bathroom is being disinfected by the UV device. They should place a card in the room indicating to the next patient that UV technology has been used in the room. This improves patient satisfaction because the patients know the most up-to-date technology is being used to ensure their safety.
- Once the patient room has been completed, the UV disinfection of the bathroom will be completed. ES staff should set up and correctly position the UV device in the patient room, exit the room and activate the UV disinfection process.
- While the UV disinfection process is being completed in the patient room, ES staff should set up for cleaning the next assigned room. They also should ensure that all safety signage is in place before leaving.
- After the UV device has completed disinfecting the patient room, it should be returned to its assigned storage space and properly secured and locked.
Documenting UV programs
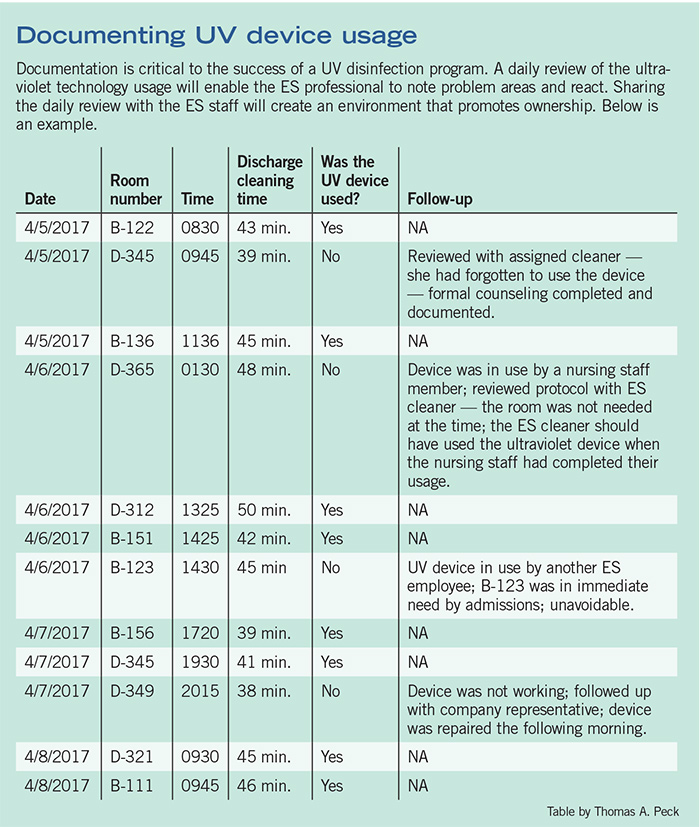
A daily review and documentation of ultraviolet technology usage will enable the ES professional to note problem areas and react. Download this PDF of a sample UV documentation.6. Monitor progress. For the UV technology to succeed, it must be closely monitored.
A plan should be developed that ensures daily utilization monitoring of the UV disinfection technology. On a daily basis, ES professionals should download the utilization data from the device. Completing this daily download at the same time every day will help to ensure compliance.
ES professionals should have the UV utilization review as part of their daily agenda. They should determine whether the UV device was used as intended following every patient discharge on the selected patient units. They also should follow up on any discrepancies. If the UV device was not used as intended, they must follow up with the ES employee and supervisor. A chart can be used to conduct this daily review [see table, Page 49]. While 100 percent usage is not realistic, ES departments should strive for at least 90 percent.
On a monthly basis, ES professionals should review HAI rates with the infection control department. Have HAIs been reduced on the patient units in which the UV technology has been utilized? Monthly infection rates should be charted by patient unit. If the UV technology is successful, the chart will depict a downward trend on the patient units that are utilizing the UV disinfection device. These results should be shared at every infection control committee meeting.
A positive reduction in HAIs that can be directly linked to the use of the UV technology will be a powerful tool for justifying an expansion of the UV technology throughout the facility. Successes in reducing HAIs also should be shared with the finance department.
Achieving the goal
The goal of introducing UV technology into the environmental services department is to provide each patient a clean and safe healing environment and to reduce the significant expense of HAIs. Following these steps will significantly improve the ES professional’s success in achieving this goal.
Thomas A. Peck is an environmental services consultant based in Madison, Wis. He can be reached at tandtpeck@icloud.com.