UPMC, Microsoft to build tech-driven digital hospitals

Rendering of the new Heart and Transplant Hospital at UPMC Presbyterian, one of three "digital hospitals" planned at UPMC
The University of Pittsburgh Medicine Center (UPMC) is investing $2 billion to build three “digital hospitals of the future.” The academic medical center describes the hospitals as “leading-edge, new specialty hospitals that will offer next-generation treatments in patient-focused, technology-enhanced settings unique to health care.”
The planned hospitals include the all-new UPMC Heart and Transplant Hospital, UPMC Hillman Cancer Hospital and UPMC Vision and Rehabilitation Hospital.
UPMC is collaborating with Microsoft to build on existing research collaboration with the tech company’s Azure cloud platform. Jeffrey A. Romoff, UPMC president and CEO, says that “we will apply technology in ways that will transform what today is often a disjointed and needlessly complex experience for patients and clinicians. UPMC and Microsoft will have more to share in the coming months.”
The hospitals will be situated on the campuses of UPMC’s Mercy, Presbyterian and Shadyside hospitals. Designs for the UPMC Heart and Transplant Hospital and the UPMC Hillman Cancer Hospital will be selected in an international design competition.
Patented technology to bring high-quality telemedicine to rural Texas
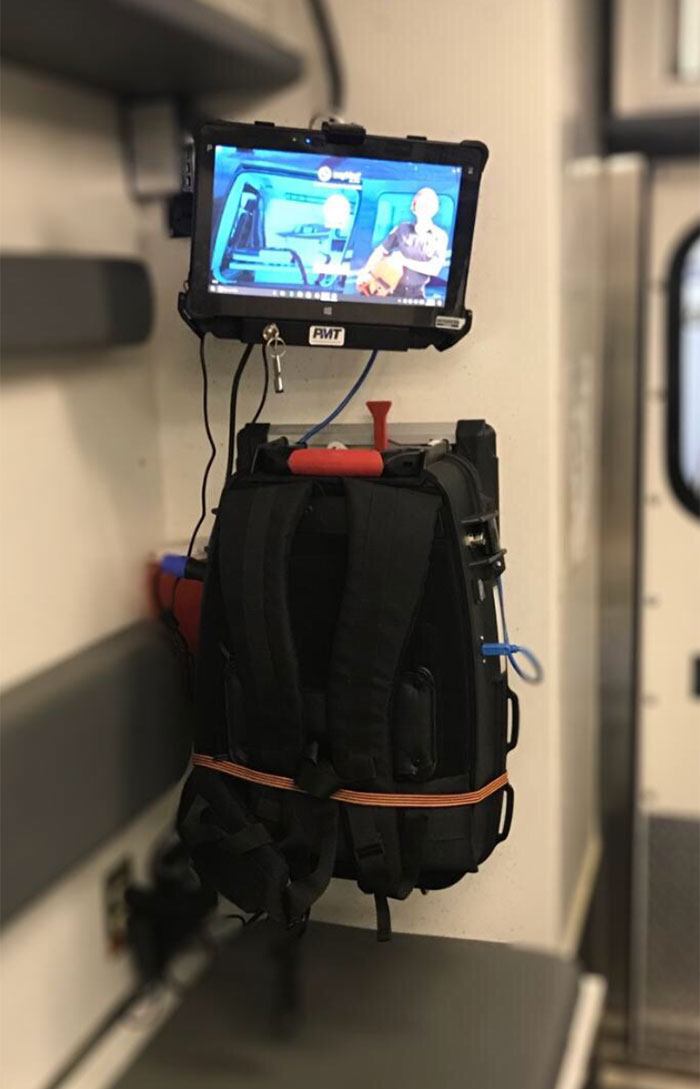
A new initiative is bringing telemedicine directly to ambulances operating in rural Texas.
A new program will bring emergency telemedicine care to rural areas of West Texas. The Commission on State Emergency Communications and Texas Tech University Health Sciences Center are piloting an initiative to implement telemedicine between emergency medical services providers and a select group of rural trauma centers. The initiative is part of the Next Gen 9-1-1 Telemedicine Project, which is initiative aimed at updating the 9-1-1 service infrastructure in the United States and Canada.
The objective of the project, which is being funded by Texas House Bill 479, is to improve patient outcomes by using telemedicine technology and to bring the expertise of trauma surgeons into the ambulances virtually to assess and direct treatment.
swyMed is providing patented data transport protocol and carrier redundancy able to deliver high-quality video even at the lowest bandwidths and in the most remote areas. Its DOT Telemedicine Backpack is being installed in 10 test ambulances, and LTE/4G cellular signal from Verizon and AT&T will be used to link those ambulances to both local trauma centers and University Medical Center in Lubbock. Additional ambulances will added over the next four years.
Those working on the project say that it can help to reduce unnecessary care and reduce health costs. They also say it can help to avoid too common scenarios in which patients are transported sometimes up to 90 minutes via ambulance to the nearest hospital only to find that the facility is not equipped to handle their needs, or end up being airlifted to a Level I trauma center when their injuries could have been handled in a closer local hospital.
ECRI lists top medical technology challenges for 2018
The list for 2018 includes:
- Ransomware and other cybersecurity threats to health care delivery can endanger patients.
- Endoscope reprocessing failures continue to expose patients to infection risk.
- Mattresses and covers may be infected by body fluids and microbiological contaminants.
- Missed alarms may result from inappropriately configured secondary notification devices and systems.
- Improper cleaning may cause device malfunctions, equipment failures and potential for patient injury.
- Unholstered electrosurgical active electrodes can lead to patient burns.
- Inadequate use of digital imaging tools may lead to unnecessary radiation exposure.
- Workarounds can negate the safety advantages of bar-coded, medication-administration systems.
- Flaws in medical device networking can lead to delayed or inappropriate care.
- Slow adoption of safer enteral feeding connectors leaves patients at risk.
The list is available as a free download on ECRI's website.





