It's not often that new hospital programs are envisioned by a physician's mom, but it happened in the geriatric emergency department at St. Joseph's Regional Medical Center in Paterson, N.J.
When Chairman of Emergency Medicine Mark S. Rosenberg's mother experienced surgical complications and suffered kidney failure in 2002 and 2003, she often had to visit the emergency department near her home in South Florida's Broward County. "She was so afraid to be in the ED because of the gang-violence patients and the screaming and people in pain," says Rosenberg, a doctor of osteopathic medicine. "She would sometimes even lie to [ED staff] just to get out of there. She said to me, 'Why don't we build an emergency department that's designed for seniors, just like we do for kids?'"
So Rosenberg met with his mother, two aunts and friends from her bridge group to talk about what they'd like to see in a senior emergency department. After a few years in planning, St. Joseph's opened the first iteration of its geriatric ED in April 2009. The 11-bed space was located on the hospital's third floor and featured natural lighting on three sides. It provided a quieter, less chaotic environment than a typical adult ED.
 |
Patient satisfaction went up, while return visits and admissions went down. "Overall we considered it very, very successful," Rosenberg says.
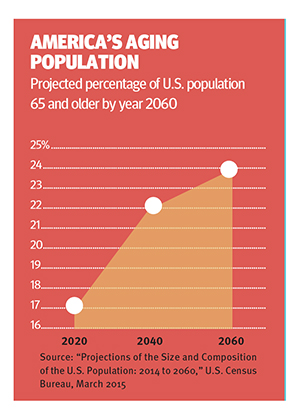
In its attention to senior patients' specific needs, St. Joseph's was on the leading edge of a growing trend. The burgeoning senior population, the shift toward outpatient care and payment for value, and changes in Medicare reimbursements are sparking innovations in geriatric care at many hospitals. In addition to geriatric EDs, the innovations encompass senior-oriented service line adaptations and wellness programs.
Extra care in the ED
In 2012, St Joseph's relocated its geriatric ED downstairs in 2012, next to the adult emergency department, and expanded the unit to 24 beds. The environment remains calm, aided by harpists and aromatherapy, and still boasts features that meet seniors' needs, such as thicker mattresses to guard against pressure ulcers.
Most importantly, the actual delivery of care has been adapted. Most patients come to the geriatric ED for unscheduled urgent care and usually arrive during daylight hours. At St. Joseph's, senior ED patients are put into a bed almost immediately. The typical time between a senior patient's arrival and when he or she is seen by a doctor is 14 minutes, Rosenberg says.
Since the geriatric ED launched, the percentage of its patients who are admitted has fallen from 54 percent to 34 percent, Rosenberg says. Avoiding hospitalization for low-complexity patients frees up beds for high-complexity patients who need them the most. It also cuts costs for coverage plans, patients and the health system as a whole.
Service line adaptations
To improve the quality and experience of care for senior inpatients, some hospitals are bringing geriatric expertise to particular service lines, depending on their populations' needs.
To help seniors with serious behavioral health needs, Thomas Jefferson University Hospital in Philadelphia has a 12-bed inpatient unit staffed by geriatric psychiatrists. Soft, warm wall colors are intended to calm patients, while wide, tiled floors make movement safer for elderly patients with wheelchairs or walkers.
In Wheat Ridge, Colo., Lutheran Medical Center opened a senior behavioral health program in 2013. "We were seeing a great deal of behavioral health patients who had clinical medical comorbidities," says Grant Wicklund, president and CEO of the medical center, part of the SCL Health system. "Patients ended up as inpatients but scattered around the hospital. It was very difficult to treat them from both a social-psychological standpoint, as well as a clinical-medical standpoint simultaneously."
The 20-bed unit is managed by the system's West Pines Behavioral Health, a psychiatric facility on the same campus, but it is housed in the medical center. Its acute care location means the unit can admit sicker patients because they can be transferred quickly to a higher level of medical care if their physical conditions deteriorate.
With a growing senior population and an already successful geriatric ED, the medical center was looking for other opportunities to differentiate its care and improve seniors' hospital experience and launched a senior surgery program in 2013.
Because elderly patients' skin often is fragile and prone to bed sores, staff use extra cushioning while positioning patients to protect vulnerable areas. Heated air is circulated through elderly patients' gowns to keep them warm.
Other amenities include soft room lighting, reading glasses, magnifiers and pocket talkers, small units that amplify sound and reduce background noise for people with hearing impairment
Outside the hospital walls
Health reform and Medicare payment changes have spurred some hospitals to offer services outside the traditional inpatient and emergency realms.
More hospitals are forming partnerships with fitness centers and YMCAs to offer wellness and exercise programs for the elderly, she notes. Other hospitals provide such programs in their own wellness centers.
Mount Sinai Hospital in New York City houses its outpatient geriatrics practice and senior wellness services in its Martha Stewart Center for Living, which opened in 2007. It also is involved in a broader falls prevention program as one of the sites for the STRIDE clinical trial, sponsored by the National Institutes of Health and the Patient-Centered Outcomes Research Institute.
"It has been an evolutionary thing that has happened over the years one layer at a time," says Albert Siu, M.D., professor and system chair for geriatrics and palliative medicine at Mount Sinai's Icahn School of Medicine. "We've tried to complete the continuum of care all the way around."
Read the original article from our sister publication, Hospitals & Health Networks for more information on how hospitals are addressing the health care needs of older patients.





