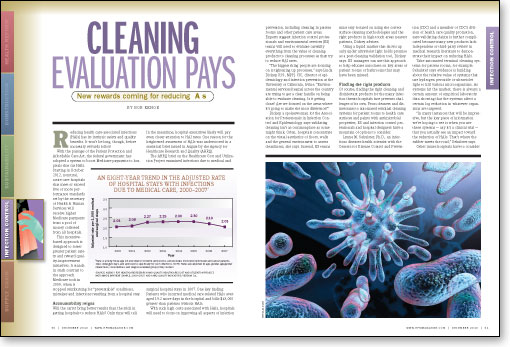
Reducing health care-associated infections (HAIs) has its intrinsic safety and quality benefits. It won't be long, though, before monetary rewards follow.
With the passage of the Patient Protection and Affordable Care Act, the federal government has adopted a system to boost Medicare payments to hospitals that cut HAIs. Starting in October 2012, nonrural, acute care hospitals that meet or exceed five or more performance standards set by the secretary of Health & Human Services will receive higher Medicare payments from a pool of money collected from all hospitals.
This incentive-based approach is designed to foster greater patient safety and reward quality-improvement initiatives. It stands in stark contrast to the approach Medicare took in 2009, when it stopped reimbursing for "preventable" conditions, mistakes and infections resulting from a hospital stay.
Accountability reigns
Will the carrot bring better results than the stick in getting hospitals to reduce HAIs? Only time will tell. In the meantime, hospital executives likely will pay even closer attention to HAI rates. One reason for the heightened awareness of HAIs was underscored in a statistical brief issued in August by the Agency for Healthcare Research and Quality (AHRQ).
The AHRQ brief on the Healthcare Cost and Utilization Project examined infections due to medical and surgical hospital stays in 2007. One key finding: Patients who incurred medical care-related HAIs averaged 19.2 more days in the hospital and bills $43,000 greater than patients without HAIs.
With such high costs associated with HAIs, hospitals will need to focus on improving all aspects of infection prevention, including cleaning in patient rooms and other patient care areas. Experts suggest infection control professionals and environmental services (ES) teams will need to evaluate carefully everything from the value of cleaning products to cleaning processes as they try to reduce HAI rates.
"The biggest thing people are focusing on is tightening up processes," says Linda Dickey, R.N., MPH, CIC, director of epidemiology and infection prevention at the University of California, Irvine. "Environmental services [teams] across the country are trying to get a clear handle on being able to evaluate cleaning. Is it getting done? Are we focused on the areas where it's going to make the most difference?"
Dickey, a spokeswoman for the Association for Professionals in Infection Control and Epidemiology, says validating cleaning isn't as commonplace as some might think. Often, hospitals concentrate on the visual aesthetics of floors, walls and the general environment to assess cleanliness, she says. Instead, ES teams must stay focused on using the correct surface-cleaning methodologies and the right products in high-touch areas nearest patients, Dickey advises.
Using a liquid marker that shows up only under ultraviolet light holds promise as a post-cleaning validation tool, Dickey says. ES managers can use this approach to help educate associates on key areas of patient rooms or bathrooms that may have been missed.

Finding the right products
Of course, finding the right cleaning and disinfectant products for the many infection threats hospitals face presents challenges of its own. From cleaners and disinfectants to automated terminal cleaning systems for patient rooms to health care surfaces and paints with antimicrobial properties, ES and infection control professionals and hospital designers have a mountain of options to consider.
Lynne M. Sehulster, Ph.D., an infectious diseases health scientist with the Centers for Disease Control and Prevention (CDC) and a member of CDC's division of health care quality promotion, says validating claims is further complicated because many new products lack independent or third-party review in medical research literature to demonstrate their impact on reducing HAIs.
Take automated terminal cleaning systems for patient rooms, for example. Sehulster says evidence is building about the relative value of systems that use hydrogen peroxide or ultraviolet light to kill various microorganisms. As systems hit the market, there is always a certain amount of empirical laboratory data showing that the systems affect a certain log reduction in whatever organisms are targeted.
"In many instances that will be impressive, but the key piece of information we're hoping to see is when you use these systems — say it's a clinical trial —that you actually see an impact toward the reduction of HAIs. That's where the rubber meets the road," Sehulster says.
Other issues hospitals have to consider with these technologies, Sehulster notes, is the amount of staff time required in the room cleaning process. Research studies on these products often mention but don't emphasize the need to pre-clean surfaces.
"When you look at the instructions for all of these technologies at the moment, they certainly advise that surfaces to be treated should be pre-cleaned first, and that can be fairly labor intensive depending on how much cleaning is needed to help prepare the room," Sehulster says.
Surface issues
The research picture also is still emerging on the antimicrobial benefits such metallic surfaces as copper and silver have in reducing HAIs, Sehulster says. At the Fifth Decennial International Conference on Healthcare-Associated Infections held in March, the Copper Development Association (CDA) and a team of researchers from the Medical University of South Carolina presented clinical trial results assessing the ability of antimicrobial copper to reduce the amount of bacteria on surfaces commonly found in intensive-care unit patient rooms.
The first phase of the clinical trials, which were funded by the Department of Defense, showed that the most commonly contaminated surfaces were those in closest proximity to patients. High levels of Staphylococcus aureus, methicillin-resistant S. aureus and vancomycin-resistant enterococci were found on bedrails, call buttons and visitor chairs. In the second phase of the trial, copper bedrails, chair arms, call buttons, monitors and IV poles replaced the stainless steel and plastic versions in ICU rooms in three hospitals participating in the study: Memorial Sloan-Kettering Cancer Center in New York, the Medical University of South Carolina and the Ralph H. Johnson VA Medical Center, both in Charleston.
ICU rooms were chosen for a specific reason, noted Michael Schmidt, Ph.D., professor and vice chairman of the Department of Microbiology and Immunology at the Medical University of South Carolina in a release on the study.
"One in 20 hospital patients will develop a hospital-acquired infection; that number increases to 30 percent for patients in intensive care units," Schmidt explained.
The clinical trial results showed copper was effective in significantly reducing the total bacteria load in ICU patient rooms and on many individual objects in those rooms. But the CDA also reported "further study is needed to assess whether copper surfaces can play a role in preventing cross contamination and the transmission of hospital-acquired infections."
The key issue, Sehulster says, is whether future studies will demonstrate that copper-clad surfaces achieve the same stated log reductions of microorganisms over a defined time period in ICUs and other settings.
"There are empiric statements of performance, but what we need to see is whether putting these [surfaces] into daily use has an impact on the transmission of contamination and what happens to the hospital-acquired infection rate. Does it go up, down or stay the same?" Sehulster says.

Emerging infection threats
With threats from multidrug-resistant organisms always present, hospitals can use all the effective weapons they can get. One particularly dangerous and often deadly bacterial threat known as KPC — short for Klebsiella pneumoniae, exhibiting extended resistance to carbapenem antibiotics via carbapenemase, a bacterial enzyme capable of inactivating carbapenems — has caught the attention of infection control and prevention experts.
Earlier this year, 37 health facilities in Chicago reported an average of 10 KPC cases each, up from an average of four in 2009 in 26 facilities, according to the Chicago Tribune. Fortunately, KPC has not become a nationwide problem.
"Thankfully, we're not seeing it broadly across the country, but everyone [in the infection control community] is definitely keeping their eyes on it," Dickey says. "This is exactly what we're talking about in making sure that we have strong processes for [cleaning] devices, strong hand hygiene programs and strong environmental cleaning programs."
The CDC's Sehulster says KPC and the large group of carbapenem-resistant Enterobacteriaceae are disconcerting because they are difficult to treat with third and fourth generations of Beta-lactam antibiotics such as cephalosporin and other relatives of methicillin and penicillin.
"[KPC] is particularly troubling because it often is associated with urinary tract infections, wound infections, ventilator-associated pneumonias or respiratory infections," Sehulster says, adding that these types of infections account for 15 percent or more of all HAIs.
The good news in this situation, Sehulster says, is that evidence developed to date shows that hospital ES teams don't need to do anything appreciably different from following CDC recommendations for cleaning and disinfecting strategies to protect patients and staff. Sehulster says the evidence indicates that the extended spectrum of antibiotic resistance is a phenomenon that is largely independent of a bacterium's ability to resist inactivation via disinfectants. The latter is influenced more by the structural features and surface biochemistry of bacteria and, more often than not, antibiotic resistance is a phenomenon associated with metabolic processes using enzymes. In short, she says, we do not need more powerful disinfectants at this time.
"We might take some steps to ensure cleaning effectiveness with some of the technology that is available. We may do more observation and follow-up to make sure that cleaning and disinfecting are done, but we're not changing what we're doing. We're just doing more of it," Sehulster says.
Bob Kehoe is associate publisher of Health Facilities Management.
| Sidebar - Computers aid fight against HAIs |
| Hospitals that use automated surveillance systems to identify health care-associated infections (HAIs) are more likely than those that rely on manual methods to deploy evidence-based infection control practices. That's the conclusion of a study presented in July at the 37th Annual Conference & International Meeting of the Association for Professionals in Infection Control and Epidemiology. Researchers at the University of California, Berkeley, conducted a survey of quality directors at 80 percent of the state's general acute care hospitals and found that those using automated surveillance systems to identify HAIs were more likely than those who rely on manual methods to have fully implemented research-based practices to reduce:
Automated surveillance technologies, often referred to as "data mining," are designed to collect infection data, thereby allowing infection preventionists to better protect patients by identifying and investigating potential clusters of HAIs in real time. "Our findings suggest that hospitals that use automated surveillance technology are able to put more HAI elimination strategies into place that will ultimately reduce the risk of infection," says Helen Halpin, Ph.D., the study's lead author and professor of health policy at the university, in a release on the project. |
| Sidebar - New CDC tools evaluate cleaning of environment |
| The Centers for Disease Control and Prevention recently posted a series of online tools to help hospitals evaluate options for environmental cleaning. The toolkit includes a white paper by Alice Guh, M.D., MPH, and Philip Carling, M.D., entitled "Options for Evaluating Environmental Cleaning" as well as an environmental checklist for monitoring terminal cleaning and a spreadsheet for monitoring terminal cleaning activities in high-touch areas. The white paper focuses on elements of Level I and Level II cleaning programs, elements of educational intervention and objective methods for evaluating environmental hygiene. All of the tools can be downloaded at www.cdc.gov/HAI/toolkits/Evaluating-Environmental-Cleaning.html. |