An emergency power (EP) system's role in patient safety is critical to hospitals and regulators. Each hospital EP system must power what the health care facility needs, when and for as long as it needs it.
That is a tall order and one that likely will become more complicated as new requirements and technologies increase the demands on these systems.
So, how can hospitals prepare for these challenges? What measures should they take? Of what dangers should they be aware? These questions can be answered by exploring and analyzing six critical areas of emergency power management.
1. System reliability
Reliability continues to be one of the most important challenges in health care facility EP systems. Needs are growing as budgets continue to shrink. How do facility professionals inspect, test and maintain more with less operating funds? How do they meet more restrictive codes and standards with smaller capital budgets?
Tightening construction budgets results in a focus on "Is it code-required or not?" Facility professionals often see the disparity between code-required minimums and what it really takes to keep a hospital operating effectively.
Some wish for tighter codes so they will be able to argue for features they want in their new EP systems, such as transfer switch bypass/isolation functions and larger generator sets. Others argue against tighter codes because of higher capital cost, and because their operational budgets simply cannot afford the increasing emphasis on testing and maintenance. A strong groundswell also is building within the health care industry against any code changes that are not supported by sufficient empirical proof of value.
Many concerns with EP reliability parallel the requirements found in the new critical operations power systems (COPS) requirements that first appeared in the 2008 version of the National Fire Protection Association's NFPA 70, National Electrical Code®.
While many hospital power systems are not necessarily classified as COPS, the COPS requirements cover many issues that are important to EP reliability. They include: risk assessments; identifying hazards and undertaking hazard mitigation strategies; performing documented load testing and documented maintenance; commissioning new power systems; providing surge protection and selective coordination; using bypass-isolation transfer switches; selective load pickup and load shedding; keeping at least 72 hours of on-site fuel storage; providing means to connect portable generator sets; providing both physical security and physical protection; separating between normal power and EP; limiting possible equipment locations; considering exposure to the 100-year floodplain; clear labeling; fire protection; and many other requirements.
The Joint Commission issued its "Sentinel Event Alert, Issue 37: Preventing adverse events caused by emergency electrical power system failures" in 2006. Since then, many hospitals have performed an EP gap analysis that considers what is powered from EP and what is not. Moreover, many hospitals have performed vulnerability analyses and risk assessments of EP reliability. However, many other hospitals have not performed these assessments.
An industry ListServ has seen many recent discussions about the pros and cons of running a hospital's generators weekly, including finding incipient failures sooner vs. the impact of increased cycling from more starts each month.
Some states require it; many do not. Some generator manufacturers recommend it. There are good arguments on both sides of the issue, particularly about following manufacturers' recommendations.
2. Maintenance and shutdowns
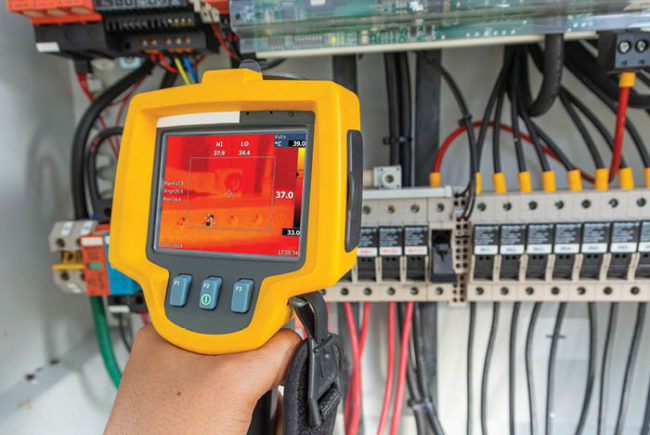
How many hospitals actually conduct power shutdowns to perform maintenance? What backup provisions are considered when equipment is de-energized for maintenance? Safe electrical maintenance requires turning off the power, and with the changes in the 2009 edition of NFPA 70E, Standard for Electrical Safety in the Workplace, there has been an increasing focus on electrical arc-flash safety.
How many hospitals keep their electrical one-line diagrams updated to reflect current system configuration? Without updated documentation, how do hospitals plan to manage internal electrical failures effectively? There are parallels between activities required for successful planned shutdowns and emergency management procedures for unplanned failures.
Hospitals that are not fortunate enough to have bypass-isolation transfer switches find it difficult to maintain their transfer switches, because doing so safely requires de-energizing the branch fed by the switch. As a result, transfer-switch maintenance in those cases is often minimal at best.
3. Circuit breaker testing
Emergency power circuit breaker exercising requirements generally have been enforced inconsistently in the past. However, some Centers for Medicare & Medicaid Services-contracted state organizations have started enforcing these requirements during surveys.
This situation has caused consternation for facilities that previously have not been held to them. The 1999 edition of NFPA 99, Standard for Health Care Facilities, requires that the essential electrical system (EES) "main and feeder circuit breakers shall be inspected annually and a program for periodically exercising the components shall be established according to manufacturer's recommendations."
Based on the EES definition, one might infer that the requirement for periodic exercising extends not only to the breakers between the generator and related transfer switches (which is the limited scope of a somewhat similar 1999 NFPA 110, Standard for Emergency and Standby Power Systems requirement), but also the life-safety branch and critical-branch circuit breakers on the load side of the transfer switch. Feeder breakers can be found in electrical distribution systems down to and including main breakers on the lowest-level panelboards.
But what about facilities in which the generators are paralleled with the incoming utility service? In those situations, depending on the design, the power to the emergency loads might go through the hospital's main switchboard. So, it is possible that the requirement for periodic exercising might extend to most or all of the circuit breakers in the higher distribution system levels. Facilities, therefore, should be careful in system designs and boundary definitions or they may be in for a surprise from an authority having jurisdiction (AHJ).
There has been some pushback about this requirement from health facilities professionals who believe exercising (opening and closing) an EES circuit breaker can cause substantial disruption within the hospital.
 |
| LEFT Five Cummins Power Generation generator sets — four gas and one diesel — installed at a hospital. RIGHT This paralleling switch from Generac Power Systems allows the main power leads of each generator to be connected together at a common point. |
4. Fuel oil storage
Although many hospitals have more than the minimum required on-site storage of fuel oil as a result of years of focused emergency-management planning, those intending to make changes in existing EP systems or to install new EP systems could be affected by the change in fuel oil storage requirements in the 2010 Guidelines for Design and Construction of Health Care Facilities.
Whereas the 2006 edition required only 4 hours of fuel storage, the 2010 edition now requires storage capacity that permits continuous operation for at least 24 hours. The required on-site EP fuel oil storage capacity is different for different states, and is sometimes even different depending on the locality.
Regardless of the on-site storage capacity, hospitals continue to face the question of how much fuel to have on hand and how to manage that stored fuel oil according to NFPA 110 requirements.
5. Failure planning
As more clinical, support and infrastructure-management functions become electronic, the EP system importance continues to grow. For instance, has the increasing importance of the electronic health record been matched by equally robust contingency planning for internal electrical failures?
Hospitals should ensure that their internal EP component and system failure contingency plans are effective and that user responses also will be equally effective. Most hospitals have failure procedures for generator failures. Many also have practiced those procedures. If a generator fails during a utility outage, there likely will be clinical and support service impact. Those protocols should be determined and practiced as well.
Other than generator failures, there also can be such internal failures as a transfer switch or the critical branch riser in a patient tower. Transfer switches are complex electromechanical devices that fail from time to time. Riser failures have been caused by events such as sprinkler head damage or contractor core drilling. It is wise to have predetermined responses for these internal failures that could have severe impact on patient care.
6. Construction and modifications
Without clear EP system branch marking and strong construction management policies, it is easy for ongoing changes in hospitals to lead to improper connections of new equipment and modifications.
Many hospitals find equipment connected to the wrong branch (e.g., life-support equipment connected to the life-safety branch). Hospitals also report that they are surprised to find red outlets that go dead when normal power drops out.
Sometimes such situations occur with new construction or renovation projects and could have been corrected with a concerted commissioning effort. Sometimes this situation is long-standing and the culprit cannot be determined.
Without an effort to field-validate the existing EP system, these situations are hidden from view until an internal failure exposes them. At that point one can only hope that there is no negative patient-care impact.
Another impact of ongoing construction and renovations is the impact on the loading that will be seen by the transfer switches and generators under worst-case conditions, also known as peak demand loading. Because monthly load tests often are scheduled for low-activity times, load test readings usually do not represent real peak demand load.
Some state AHJs require that hospitals know and report their existing EP peak demand loading before modifications are approved. However, most do not. Most hospitals do not have permanently installed metering to facilitate that process. There are a number of approaches for accurately determining EP peak demand loading.
Some also have expressed concern not only about not being able to predict EP load growth over years, but also after utility power has been off for days. Some have reported that upon investigation, existing transfer switches and even generators have been found to be overloaded for worst-case situations. In fact, EP load growth actually has surprised some health facilities after disasters occurred.
Substantial electrical system modifications also could invoke the need to update existing electrical system selective coordination studies and the corresponding arc-flash hazard energy analysis. Electrical systems with poor selective coordination can have outages that are more extensive than necessary.
The selective coordination issue has been and still is controversial, and some NFPA code-making panels have been attempting to deal with it.
David L. Stymiest, P.E., CHFM, FASHE, is a senior consultant at Smith Seckman Reid Inc., Nashville, Tenn., and chairman of the NFPA Technical Committee on Emergency Power Supplies. His e-mail is DStymiest@SSR-inc.com. The views and opinions expressed in this article are the author's own and not the official position of NFPA or any of its technical committees and should not be considered to be, or relied upon to be, a formal interpretation. Readers are encouraged to refer to the entire text of all referenced documents and NFPA members can obtain staff interpretations of the various standards by logging on to www.nfpa.org.
| Sidebar - Resources on the web |
| The resources below were used by the author to prepare this article. National Fire Protection Association (www.nfpa.org) documents: American Society for Healthcare Engineering (www.ashe.org) resources: Health Facilities Management magazine (www.hfmmagazine.com) articles: |