 The environmental services (ES) team at Advocate Christ Medical Center (ACMC) and Hope Children's Hospital has its hands full at all times.
The environmental services (ES) team at Advocate Christ Medical Center (ACMC) and Hope Children's Hospital has its hands full at all times.
The Oak Lawn, Ill., medical center, now 50 years old, is among the busiest in the Chicago area with 40,700 inpatient admissions in 2010. It routinely operates at 95 percent capacity or higher, with most patients in semiprivate rooms. ACMC's emergency department experiences about 95,000 patient visits annually. Hope Children's Hospital has treated heart patients from every continent.
As a teaching hospital, Level I trauma center and acute care facility, ACMC provides a diverse array of care services to an equally diverse community.
This has created a major throughput challenge for these facilities, which border Chicago's South Side. Maintaining high levels of patient satisfaction can be difficult in the best of times, but particularly now given the facility's age, patient volume and high acuity level, and large visitor population.
Overcoming the challenge
Through it all, though, the ES team under the leadership of Karen Martin, R.N., director of infection prevention and environmental services, isn't looking for excuses — just consistently excellent results in maintaining 1.3 million square feet of cleanable space in these facilities.
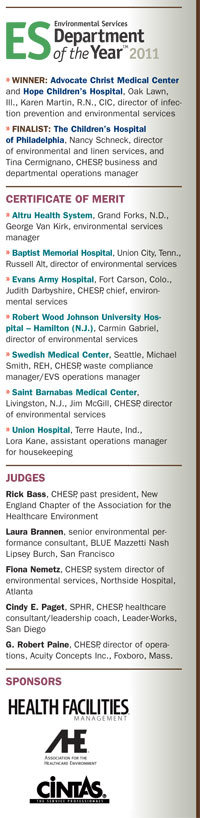
As the winner of Health Facilities Management and the Association for the Healthcare Environment's 2011 ES Department of the Year award, sponsored by Cintas, Cincinnati, Martin's team has delivered an impressive resumé of achievements. Among their accomplishments during 2010:
• The ES team's close working relationship with the infection prevention and nursing teams helped lead to a 55 percent decrease in Clostridium difficile rates at ACMC.
• A comprehensive, evidence-based environmental hygiene program standardized and simplified cleaning practices for 17 high-touch areas in patient rooms and bathrooms. This led to a better than 58 percent improvement in cleaning consistency for these touch points.
• Improved processes and communication drove down room turnaround times from an average of 73 minutes in 2009 to 44 minutes in 2010.
• Focused staff training caused patient satisfaction scores for cleanliness and courtesy from Press Ganey Associates Inc., South Bend, Ind., to spike at ACMC and hit 95 percent for Hope Children's Hospital.
Infection prevention connection
 The foundation for the ES team's success in working shoulder-to-shoulder with the infection prevention team was laid in 2008. A chief nurse executive at the time planned to restructure some departments to help improve throughput. She added the responsibility of the ES department to the clinical support services manager.
The foundation for the ES team's success in working shoulder-to-shoulder with the infection prevention team was laid in 2008. A chief nurse executive at the time planned to restructure some departments to help improve throughput. She added the responsibility of the ES department to the clinical support services manager.
As the restructuring unfolded, the clinical support services director eventually moved to another Advocate facility on an interim basis. Martin, then manager of infection prevention who reported to the director of clinical support services, was asked to manage the ES team during this time. She capitalized on the opportunity.
"Although I had worked with the ES department, now was really my opportunity to align with them," Martin says.
As she was reading a story about Florence Nightingale and how she was able to get nurses to become more valuable assets in patient care, Martin saw a parallel with the ES team. She began attending ES meetings on a more regular basis and tried to connect associates more directly with their purpose.
"I told them, 'It's not just about cleaning a room. You clean a room because you don't want to cause infections,'" Martin recalls. "I went as far as showing them photos of flesh-eating disease, staph infections and C. diff infections, what happens if people don't wash their hands properly and don't clean rooms properly."
Building competencies
Those messages and other efforts, such as conducting mock trials or discussing legal cases involving infections acquired in hospitals, resonated with the 200-plus ES staff. She also focused on building associates' competencies. When the director returned from her interim assignment in 2009, Martin's role in managing infection prevention and ES became permanent.
Martin knew she'd need support in this role and three managers were hired to assist. But they weren't the only ones who had to adapt to the new departmental structure. Martin was used to managing nurses, who tend to be critical thinkers, but the ES team's culture was more task-oriented.
"My first objective was to manage this group in order for them to better understand their role. Much more important than performing daily tasks, they needed to know that they played a key role in the success of measurable outcomes related to infection prevention," Martin says.
Phil Haglund, interim business manager at ACMC, who assumed responsibility for educating staff, developed and implemented a comprehensive new employee orientation program in 2010. The program covers department-specific policies and guidelines, safety and regulatory agencies, infection prevention, medical waste, patient satisfaction and departmental cleaning procedures.
Verifying cleaning results
ACMC and Hope Children's Hospital also became among the first facilities to pilot a new system to standardize and validate environmental hygiene practices. Haglund says deploying St. Paul, Minn.-based Ecolab's PROTECT program had a significant impact on cleaning competency, productivity and reducing room turnaround times. The program uses Lean, Six Sigma and Hazard Analysis and Critical Control Point methodology to achieve consistently superior results.
"Ecolab came in and trained 220 associates on their new microfiber products and equipment. Supervisors were trained on how to do [DAZO] fluorescent gel testing to verify that 17 high-touch objects in patient rooms and bathrooms were cleaned thoroughly," Haglund says.
Testing data for all 17 high-touch objects during the baseline period in the second quarter of 2010 through the first quarter of 2011 topped 85 percent. This reflects an overall increase of 58 percent in cleaning consistency.
This type of feedback, which also is recorded and monitored regularly, provided supervisors and associates with objective performance measurements to help drive more consistent results.
Haglund and Martin say the evidence-based cleaning program and other efforts also contributed significantly to the large decrease in C. diff cases ACMC saw in 2010. They say infection control professionals, the ES team and the nursing staff drew closer together as an initiative began to reduce C. diff rates throughout the medical center. Morning huddles among the groups brought consistent communications about C. diff patients and ensured that cleaning protocols for these rooms were consistently followed.
In March 2010, ACMC entered into a 10-hospital collaborative with the Illinois Department of Public Health and the Centers for Disease Control and Prevention to decrease C. diff rates by 20 percent over an 18-month period. As the program began, the medical center's C. diff rate was 17.6 per 10,000 patient days.
Two units with the highest incidence of C. diff were challenged to implement a comprehensive C. diff bundle that included polymerase chain reaction technology for testing validation, disinfection with a bleach solution on all high-touch areas, monitoring of personal protective equipment usage and hand-hygiene compliance.
To implement the initiative, the ES team chose to clean every C. diff room on those units with a hospital cleaner/disinfectant with bleach on terminally cleaned rooms. A manager rounds on the units twice a day and notes rooms that are indicated for C. diff isolation. The information is relayed to a bed dispatcher and supervisors. When the patient is discharged, the supervisor is notified and only a trained associate can clean the room using the disinfectant/bleach product. A manager tracks these activities on a computer and in a binder.
Sticking to these protocols, ACMC's C. diff incidence rate fell to 7.8 per 10,000 patient days by the end of February 2011 — a 55 percent decrease since the program began. It's always difficult to definitively prove how much impact revised cleaning processes and other factors had on the decrease, but Martin believes it was pivotal.
The Illinois Department of Public Health also was impressed with the improvements and plans to include ACMC in a video shoot about best practices to reduce infections.
Building on success
The ES team has built on its successes in areas outside of reducing infections and improving efficiency. In 2010 it launched a program with one of its vendors to eliminate landfilled sharps waste.
Under the program from Daniels Sharpsmart Inc., Chicago, all sharps waste at ACMC and Hope Children's Hospital is recycled. The program is projected to result in hard cost savings of more than $350,000 over a five-year period.
The team also has implemented technology to allow for chemical-free stripping of floors to minimize strong odors, slip hazards and downtime of patient rooms.
In addition to the combined impact of additional training, new tools and technologies to help associates boost performance, a bevy of recognition programs and other initiatives have translated into higher employee satisfaction. In a survey from last fall, employee satisfaction reached 79 percent.
But perhaps most telling of all about the progress with Advocate's ES team is its commitment to developing a bond with physicians. Some ES team members began rounding weekly with physicians, asking what areas they felt needed improvement. The relationships blossomed. The associates even pitched in and bought a shoe-shine station for the physicians' lounge to show their commitment to a partnership for a cleaner hospital. It was symbolic of the many steps that may help stack the deck in favor of the ES team's continued progress.
• 2011 ES Department of the Year / Finalist •

|
| Front row from left: Terri Wentzell, operations manager for support services; Nancy Schneck, director of environmental services and linens; and Steve Gallagher, operations manager for ambulatory services. middle row from left: Tina Cermignano, business and department operations manager; and Cheryl Henry, operations manager for Colket Transitional Research Building. Back row from left: Twyla Seward, operations manager for inpatient units; and Jonathan Wright, manager for quality assurance and development. |
Setting the standard - Evidence drives Children's Hospital of Philadelphia's success
Nancy Schneck makes no apologies for being a self-described "data person."
"I won't do anything or make a move without knowing where the evidence is to show that this is to our advantage," says the director of environmental and linen services at The children's Hospital of Philadelphia (CHOP), which is part of the organization's clinical team.
Schneck and Tina Cermignano, CHESP, business and department operations manager at Children's, aren't taking any chances in safeguarding the organization's precious young patients and neither are their managers or associates. Any proposed cleaning protocol changes designed to improve performance, enhance safety or prevent infections must have documented evidence of their value.
That deeply entrenched standard continues to pay dividends in performance and recognition, as CHOP's environmental services (ES) team recently received the Health Facilities Management and the Association for the Healthcare Environment's (AHE) 2011 ES Department of the Year finalist award.
Clean and green
When Schneck first came to CHOP in 2000, the organization had not yet begun a formal waste minimization or sustainability program. She began examining data on the weights of compacted material leaving the facilities each day. Waste minimization and recycling programs soon were initiated and impressive results quickly followed.
Hospitals are among the largest generators of waste in the country. CHOP believes that waste is not simply an expensive by-product of doing business but, if consistently managed as a commodity, can ultimately contribute to lowering its patient day costs.
Of its total waste last year, CHOP's recycling rate rose to 46 percent and was virtually financially self-sustaining. The hospital's regulated medical waste continued to trend downward to 3.8 pounds per patient day, representing 5 percent of total waste. Landfill waste dropped to 48 percent. This exceeded the 2010 50 percent landfill reduction sought by the Environmental Protection Agency in a memo of understanding with the American Hospital Association and the American Society for Healthcare Environmental Services (now the AHE), which was originally signed in 2005.
Since 2009, the ES team's waste reduction program efforts have helped the institution avoid more than $845,000 in costs annually when compared with expenses incurred over the previous five years. Similarly impressive results have been achieved in other areas of the department's scope of responsibilities.
An evidence-based, surface cleaning monitoring program, a close working relationship with infection control professionals and other factors have led to sustained reductions in hospital-associated viral infection rates. The hospital's nosocomial viral infection rate was at or below 0.5 per 1,000 patient days for nine of 12 months in 2010.
The ES team closely monitors its cleaning results using St. Paul, Minn.-based 3M's Clean Trace ATP (adenosine triphosphate) system to detect organic contamination on cleaning surfaces that can't be seen. The rapid test allows for assessing, measuring and validating the efficacy of cleaning protocols and performance.
"We have a nosocomial reduction initiative going on and we use the system there," Cermignano explains. "We also use it in conjunction with the clinical team. If there's an outbreak, we'll go out and test the environment to see if it's the [physical] environment or health care workers' hands."
ATP testing also is conducted on select high-touch environments in patient rooms, bathrooms and on mobile equipment. Performing six inspections of 10 items per day provides baseline data that the ES team seeks to continuously improve their daily cleaning. Data is reported to both the ES and clinical teams. Missed items are used as teachable moments in an effort to improve training and future performance.
Throughput on the rise
The ES team achieved these and other results with a consistently high patient census.
"We never go on divert," Cermignano says. "We have a full-capacity protocol, which is when we're over 95 percent census we go into the 'red zone' and we have units [that can accommodate] 104 percent census. Every room has two headwalls and they can be converted to semiprivate rooms; playrooms can be converted into patient rooms."
In this challenging environment, productivity continues to improve due to a series of initiatives. The implementation of a patient-flow command center and appointment of two dedicated ES patient-flow managers brought greater communication and improved bed management capabilities. Also, as part of the CHOP Healthcare network's strategic initiative to improve patient flow, the organization partnered with Epic software to implement a comprehensive system to track and record all patient data.
An ES module in the system aids in bed tracking, with notification instantly sent to environmental and linen services when a bed becomes dirty. Staff are assigned to a sector or zone and cleaning assignments are made through the system. The module also includes isolation precaution information for patients during their stay. This ensures that staff are aware of precautions immediately and don't have to rely on a door sign that can be removed before discharge cleaning is performed.
These and other moves have steadily improved staff efficiency, Schneck notes.
From July 2008 through July 2009, the ES team's annual staffing hours per patient day stood at 4.4. In the ensuing 12 months, this figure was reduced to 3.98, even as the total number of patient days rose by more than 5,000. And from July 2010 through the first quarter of 2011, annual staffing hours per patient day were reduced further to just 3.77 — a 10.2 percent decrease from 2008 to 2009 — while patient days rose 9.1 percent during the same period.
Another move that helps the ES team maximize productivity is the use of part-time labor exclusively for its discharge team.
"I'm a big proponent of part-time labor with regard to working four hours a day. This enables us to maximize our labor resources to ensure that during peak discharge times we are able to 'flex' our staff more effectively and efficiently to reduce patient wait time without compromising quality or safety outcomes," Schneck says.
Building on success
Much of the consistently excellent results achieved by the hospital's ES team can be traced to its hiring and comprehensive orientation and training programs. Unlike many ES team leaders, Schneck isn't big on hiring associates with hospital ES experience.
"We believe it's a lot harder to retrain someone on practices that they may have had elsewhere than it is to train them from scratch our way, with our standards," Schneck says.
New employees are taught CHOP's standards and expectations during a comprehensive three-week orientation program focused on performance excellence. Staff also are required not only to view AHE videos and all other department-based training tools for success, including infection prevention, but practice their skill base and successfully complete post-testing to ensure comprehension.
"The orientation really zooms in on performance excellence to make sure that people understand why they need to do something the way we do it to our expectation levels. And we don't mince words. We say to staff that if you do not do the job correctly … and safely, you have the child's outcome in your hands. You can help or, unfortunately, you can make that child sicker," Schneck says.
That message and the other teachings are getting through loud and clear.
Bob Kehoe is the executive editor of Health Facilities Management.





