 Instead of embracing options like stun guns and tasers, hospitals working to protect patients, staff, property and data are increasingly relying on the latest technology to meet their ever-intensifying security challenges.
Instead of embracing options like stun guns and tasers, hospitals working to protect patients, staff, property and data are increasingly relying on the latest technology to meet their ever-intensifying security challenges.
But adopting technology such as radio-frequency identification (RFID) and digital Internet protocol (IP)-video surveillance systems means hospital security and information technology (IT) departments must work together closely to design, install and maintain the sophisticated security systems that require resources from both.
While challenges remain and the definition of "integration" is not always consistent, hospitals are making strides in synchronizing those systems to maximize efficiency, according to the nationwide 2012 Hospital Security Survey conducted in June by Perception Solutions for Health Facilities Management (HFM) and the American Society for Healthcare Engineering (ASHE).
Of the 874 respondents — 85 percent facilities, security, safety and support services professionals; and 15 percent IT/chief information officers (CIOs) — more than 82 percent reported having an integrated security plan that addresses all critical access and controlled areas within the hospital. Meanwhile, 62 percent reported that physical and logical security were integrated at their facilities. The survey was sponsored by Boca Raton, Fla.-based Tyco Integrated Security.
 While not surprised that hospitals dealing with increasing crime, tightening regulations and economic challenges are embracing technology, ASHE president Jeff Arthurs, CHFM, CHSP, FASHE, director of facilities management and safety officer at Illinois Valley Community Hospital, Peru, Ill., says he's pleased with the strides they are making toward integrating those systems.
While not surprised that hospitals dealing with increasing crime, tightening regulations and economic challenges are embracing technology, ASHE president Jeff Arthurs, CHFM, CHSP, FASHE, director of facilities management and safety officer at Illinois Valley Community Hospital, Peru, Ill., says he's pleased with the strides they are making toward integrating those systems.
"Hospitals continue to deal with societywide pressures that heighten security risk, and technology increasingly offers very effective solutions," Arthurs says. "I'm pleasantly surprised by the growing level of coordination between security and IT in improving overall security. The manpower doesn't seem to be changing dramatically, but the way we manage our facilities is definitely evolving."
On the same page
While more hospitals are making progress toward integration, experts say the survey numbers are more optimistic than what they are seeing in the field.
Part of the issue, according to Mac McMillan, co-founder and CEO at CynergisTek Inc., Austin, Texas, is a matter of semantics. "Right now, a security guy might tell me the facility has an integration plan and the IT guy might tell me they don't, so it's a matter of definition," McMillan says "What I find is that most facilities have pieces or parts of a plan."
"Everyone would say they have an integrated security plan, at least in their heads," adds Jeff Bell, director of client services, CareTech Solutions, Troy, Mich. "Many of these plans are not truly optimized."
A true integration plan documents all facility controls and explains how they tie together, overlap and work from one central network, says McMillan, who estimates that less than 50 percent of hospitals he sees have such a plan. In terms of physical and logical security, Hank Monaco, vice president of customer marketing at Tyco Integrated Security, says about 20 percent of the facilities he sees are truly integrated.
"If you've had theft of a laptop, security people have to realize it's not just loss of equipment, it's the loss of data," Monaco says. "To achieve true integration between physical and logical, security and IT have to be on the same page, and we're not always seeing that."
For example, when asked whether the IT department has assigned staff to support security systems, 39 percent of respondents said "yes" while 47 percent said that there are no plans for assigned IT staff. "If there is true integration, IT is involved in every decision," says McMillan.
Overcoming barriers
Integration is a long, complicated process that varies from facility to facility, according to the survey. Likewise, survey data show varying levels of participation by security and IT on all levels of coordination and resources allocation.

|
| Click above image or here for PDF
|
Asked who performs access management changes for security systems, 28 percent of respondents said IT while 43 percent named security. When asked to rank IT's involvement in security systems planning and operations, 32 percent of all survey respondents said "rarely," 28 percent said "occasionally," while just 6 percent said "always."
This data accurately reflect what experts are seeing in the field, Monaco says.
"Security and IT executives tell us there is a divergence about who is involved, to what degree and when," Monaco explains. "IT tends to feel they're much more engaged than facilities people think they are. There is a communication breakdown that needs to be addressed on both sides."
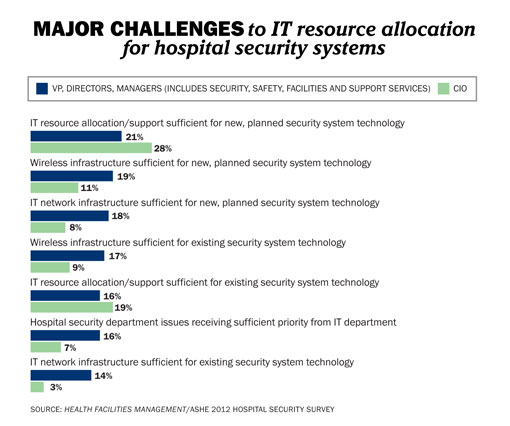
That disconnect was reflected in survey feedback. When classifying their challenges and barriers to hospital security systems and capabilities, 22 percent of all respondents indicate that IT resource allocation/support for new, planned security systems technology is a "major challenge." Other leading major challenges respondents noted included having a sufficient IT wireless infrastructure for new and planned security systems (18 percent) and having a sufficient IT network infrastructure for new or planned security technologies (17 percent).
A big factor is the growing workload placed on IT staff, says Arthurs. "Health care reform initiatives like meaningful use and electronic health records are already part of IT responsibilities," he says. "Adding security is adding more responsibility and, like a lot of departments, they are stretched to their limit."
"I'm sure IT would like to give security matters top priority all the time, but that isn't possible," adds Monaco, who says more facilities are turning to outside firms to fill their high-end integration needs.
Technology in the works
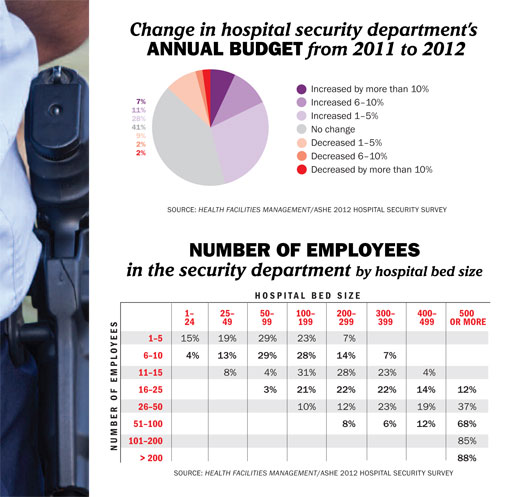
Although security budgets largely remained flat in 2012 — more than 41 percent of respondents indicated their budget had no change from the year before — many facilities plan to fortify their security programs with new technology.
The survey shows that about 61 percent of security budgets are allocated to security staff/employees and contracts while about 20 percent are dedicated to facility modification and security technology. Regulatory issues and upgrades to current systems or staffing levels are cited as the main factors driving budget changes.
In terms of the systems their organizations plan to implement in the next two years, those most often cited by respondents include digital IP-video surveillance, visitor management systems and RFID for tracking equipment, supplies, staff and patients — including infants. While infant abductions are rare, RFID technology combining a bracelet worn by an infant with a software package that issues an alert and locks down exits if necessary, is growing in popularity.
"This technology has been truly effective in stopping infant abductions and is a great way to be proactive," says Bryan Warren, CHPA, president, International Association for Healthcare Security & Safety (IAHSS) and senior manager, corporate security, Carolinas Healthcare System, Charlotte N.C. "We always say, ‘Detect it, deter it rather than defeat or defend it.'"
Bell says larger hospitals are moving toward identity and access management (IAM) systems that ease the administrative burden of adding or removing employees, and improve security and compliance.
And although just 27 percent of respondents have implemented a physical security information management system (PSIM), McMillan says the technology is critical to connecting systems. "If you have a PSIM deployed, we know there is a good chance you are moving toward achieving integration," he says.
Incidents spike
As far as crime, hospitals generally reported incident levels in line with those from 2011.
Over the past year, 25 percent of respondents report an overall increase in attacks and assaults compared with more than 7 percent reporting a decrease; 34 percent report an increase in patient/family violence against emergency department staff, while 7 percent report a drop; and 26 percent report a rise in patient/family violence against other staff, compared with 6 percent reporting a decline.
Warren says when organizations report an increase in crime, it is partly due to greater reporting of incidents — particularly with patient violence toward staff who may not have been as willing to document these incidents previously. "Staff are saying that getting bitten, punched and kicked are not part of their job, so they are reporting more incidents."
Another factor is the closure of psychiatric institutions providing specialized settings for patients, says Arthurs. "As more of these institutions close, these patients stay in hospitals longer, increasing the number of incidents."
Even with some of the more prominent incidents of violence against hospital staff members, respondents overwhelmingly say their institutions aren't looking to arm security personnel.
Eighty-two percent of respondents say they have no plans to use stun guns and 74 percent have no plans to arm security officers with guns. When the topic came up at the June 2012 Workplace Violence Prevention Summit put on by the Emergency Nurses Association and IAHSS, Monaco says a very small minority favored using such weapons. "Most don't want guns in a hospital in the first place," he notes.
Overall, 16 percent of respondents said specific individuals on the security team are licensed to be armed; 4 percent noted that only off-duty police officers working for their hospital are armed.
Human touch still critical
Hospitals turning to technology, risk assessments and strategic planning to maximize their security protocol in the coming year will continue to rely on staff who are the backbone of the department. More than 80 percent of hospitals do not plan to change their security staff levels in the next year while 16 percent plan to increase their staff.
Warren stresses that hospitals should use technology to supplement security rather than use it as a replacement for manpower. "Technology has to be a tool to enhance support, but it cannot take the place of security personnel," he says.
Health facility professionals also urge hospitals to keep on track in terms of security and risk assessments. The survey shows that nearly 81 percent of respondents perform a physical security assessment at least annually; more than 41 percent say that their security strategic plan has been updated in the last six months.
Warren also encourages security staff to seek out the training and certification programs available to them, including those through IAHSS.
"Security is its own profession," Warren says. "It's up to you to take advantage of the knowledge and training out there to increase your potential. In turn, that makes for safer hospitals."
Beth Burmahl is a freelance writer based in Oak Park, Ill., who specializes in health care-related topics, and Suzanna Hoppszallern is senior editor of data and research for Health Facilities Management's sister publication, Hospitals & Health Networks.
| Sidebar - Violence + overcrowding remain ED concerns |
|
Workplace violence, overcrowding and throughput issues continue to be the biggest challenges facing hospital emergency departments (EDs), according to health care safety professionals who say the issues are interrelated. As more hospitals and EDs close, patient levels increase at those in operation. Wait times have increased as more unemployed and uninsured patients seek basic care, worsening overcrowding and throughput problems. Emotions run high when patients in crises or pain must wait longer for care, creating situations ripe for violent incidents — often targeting hospital staff. "A survey of our membership covering the last few years shows that most ED nurses have experienced physical or verbal abuse on the job — many have experienced both — and that the frequency and volume of these assaults have not decreased," says Gail Lenehan, R.N., 2012 president of the Emergency Nurses Association (ENA). According to the most recent ENA report from November 2011, in one seven-day period, more than half of ED nurses experienced verbal abuse and more than one in 10 had experienced physical abuse, Lenehan says. More than one-third of the respondents reported an increase in patient/family violence against staff in EDs while nearly 7 percent saw a decrease in these incidents, according to a nationwide security survey conducted in June by Perception Solutions for Health Facilities Management and the American Society for Healthcare Engineering, and sponsored by Boca Raton, Fla.-based Tyco Integrated Security. One percent reported an increase in ED shootings, survey data showed. Calculating the numbers is tricky considering the confluence of factors involved and the overall increase in reporting of incidents, says Bryan Warren, CHPA, president of the International Association for Healthcare Security & Safety (IAHSS) and senior manager, corporate security, Carolinas Healthcare System, Charlotte N.C. "We know ED violence is not decreasing, but we don't know that the rate of increase can be effectively measured," Warren says. In a press briefing earlier this year during a conference exploring ways to reduce ED violence, Warren and other leaders noted that underreporting of incidents by ED staff is a major concern. Technology will continue to play a major role in ED safety as hospitals embrace systems, including electronic access control with bar-coded name tags, wired and wireless panic alarms, video surveillance and radio-frequency identification (RFID) for patient tracking. Computerized flagging of a patient's record to alert staff of a previous disruptive or violent incident is another option, Lenehan says. Strategies for combating overcrowding and improving throughput are also critical considering the enormity of the problem. In a survey of nearly 300 health care leaders, almost half (46 percent) say their ED is overcrowded, according to a 2012 HealthLeaders Media report. Along with speeding the process of transferring patients to a limited number of inpatient beds, EDs are using hallways, waiting rooms and other areas to accommodate more patients, Lenehan says. "And with a seeming increase in the number of patients who may be dangers to themselves or others, facilities will need to consider more ED rooms that can quickly be converted into safe rooms," she says. Options for improving throughput include a fast-tracking area for less acute illnesses or injuries, a triage medical evaluation process, coordination with inpatient floor nurses and a streamlined registration process, according to the HealthLeaders Media report. Knowing how and when to diffuse potentially violent situations is also critical. "A comprehensive violence prevention program, which includes training for staff, has been recognized as essential to the prevention of violent incidents in the health care setting," Warren says. "ENA's surveys reveal that the incidence of violence is significantly reduced when hospitals have a zero-tolerance policy with regard to violence," Lenehan says. IAHSS and the Occupational Safety & Health Administration promote comprehensive violence prevention programs while ENA and the American College of Emergency Physicians have issued policy statements recommending that hospitals educate staff on handling violence. |