 Peg Adamowicz has an unusual role with the environmental services (ES) team at the University of Wisconsin (Madison) Hospital and Clinics. She oversees a simulation training program in which recent ES hires are videotaped as they perform discharge cleaning and other tasks in a mocked-up patient room.
Peg Adamowicz has an unusual role with the environmental services (ES) team at the University of Wisconsin (Madison) Hospital and Clinics. She oversees a simulation training program in which recent ES hires are videotaped as they perform discharge cleaning and other tasks in a mocked-up patient room.
If associates have trepidations — and many do — Adamowicz is quick to offer words of reassurance, especially when cameras are focused on them as they talk to a dummy patient in a bed while working in a simulated space. The exercise is about achieving performance consistency and identifying opportunities for improvement.
"Right now we're concentrating on our new people and having them perform a discharge cleaning, which can be somewhat complicated. Eventually, we plan to put everyone through the program," Adamowicz says, adding that she completes a competency rating form on each employee and reviews the tape with their supervisor. All told, she invests about three to four hours in each employee.
She knows associates probably prep each other for the videotaping, but she figures that's not a bad thing. Her hunch seems to be correct. When a patient inadvertently leaves a personal item in the bed linens, it may not be discovered until the laundry is sorted — too late to match it to the owner. So, Adamowicz started placing a personal item from the dummy patient inside the linens to see if associates would find it when breaking down the linens. Early on, a number of staff missed the item. Now, nearly everyone finds it.
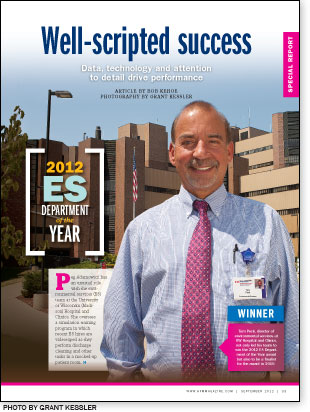
Physicians primarily use the UW Health Clinical Simulation Center for hands-on training for everything from evaluating surgical techniques to how to perform cardiopulmonary resuscitation. It wasn't long, though, before Tom Peck, UW Hospital's ES director, and his colleagues saw an opportunity and requested to use the center's videotaping capabilities.
This is one of a bevy of programs Peck and his supervisors have developed to drive the organization's ES department to peak performance and continuous improvement. It's also one of many examples that led to UW Hospital and Clinics' being selected as the 2012 ES Department of the Year. The award, sponsored by Health Facilities Management, the Association for the Healthcare Environment and Cintas, Cincinnati, recognizes outstanding ES performance in 13 critical areas.
A finalist for the ES Department of the Year award in 2010, Peck and his team continue to strive for a single important goal — to be the best in the country at providing a clean and safe environment for patient care. And with responsibility for more than 2.2 million square feet of space and 566 licensed beds on the sprawling UW Hospital campus, that's a tall order. Regardless, the team is meeting Peck's lofty objectives.
Getting results
Patient satisfaction with ES has continued to improve. Press Ganey scores for room cleanliness (88.5 percent) and staff courtesy (90.9 percent) during the fourth quarter of last year placed UW in the 99th percentile for similar academic medical centers, Peck notes. While he acknowledges room for improvement in boosting Hospital Consumer Assessment of Healthcare Providers and Systems scores for always maintaining a clean room (78 percent), he's developing action plans to meet his goal of 85 percent of patients who say their room is always clean.
Peck routinely posts data just outside his office on patient satisfaction scores and other key performance areas to keep staff engaged. "I think everyone wants to know how they're doing. I could say, 'You're doing a nice job,' and that's okay, but if I say, 'You're doing a great job' and I can show them a graph of data on our surface cleaning results, they see how they're doing," Peck says.
That visual approach has driven positive results in testing high-touch areas for cleaning thoroughness. In 2011, the team began using fluorescent marking gel to test associates' effectiveness in cleaning the top 10 highly touched surfaces in the patient room and bathroom. Results are shared immediately with the area cleaner and used as a positive teaching tool. With a baseline reading of 79 percent of surfaces thoroughly cleaned when the monitoring program rolled out in 2011, numbers have steadily improved every quarter and stood at 90 percent early in the third quarter of this year.
High-tech assistance
Elsewhere, Peck has overseen a steady influx of technologies designed to boost associates' efficiency and effectiveness. The department uses radio-frequency identification tags on critical ES equipment such as wet-dry vacuums and wet-floor signs so they can be located instantly. Central services also tags infusion pumps and other essential patient equipment so that they can be pinpointed throughout the facilities.
"This has dramatically improved the availability of equipment," Peck explains, adding that being able to track equipment helps the organization avoid buying more equipment when it's not truly needed.
Apple iPads and iTouch devices have been assigned to supervisors so that they can plug in data on surface cleaning monitoring results before they leave the patient room. This eliminates paper tracking forms and provides instant results to Peck via his vendor partner (Ecolab Inc., St. Paul, Minn.), which is working with the ES team on quality improvement initiatives.
One of the latest and more promising systems Peck's department has deployed is an ultraviolet (UV) pulsed-light disinfection system from Xenex, Austin, Texas. The unit initially was leased to aid in a facilitywide effort to reduce health care-associated Clostridium difficile.
"We started using it in our pulmonary unit and our cardiothoracic surgery unit last December. We chose those units because we're an extremely busy hospital and turnaround time is critical," Peck notes. "We wanted to be sure that we use it 100 percent of the time in these units and we're using it on every discharge."
After the ES associate performs routine cleaning of the patient room and bathroom in these units, the UV disinfection system is wheeled in and switched on. It's used in the bathroom while the associate cleans the patient room and then is placed in two strategic spots in the patient room. Peck says this adds between 10 and 15 minutes to room turnover times, but the results are worth it.
The cardiothoracic unit has had no incidents of hospital-associated C. diff during the first four months of system use and the pulmonary unit has seen significant decreases as well. Peck has monitored system performance daily and says the results have led him to buy another unit with the administration's support. The new unit is being used in areas where patients who have had organ and bone marrow transplants are treated.

Collaborative efforts
As much as technology and sophisticated systems have helped Peck and his team, their tight collaborative working relationship with the facility's infection control and prevention team and the nursing department is driving improvements in quality and patient safety. The ES team has been a key contributor in a hospitalwide initiative begun in 2011 to increase hand-washing compliance for all employees.
All ES staff were retrained on the importance and frequency of hand washing. Each supervisor is expected to document at least five hand-washing observations each month and report findings. Key personnel were trained to perform hand-washing observation of physicians, nurses, food service staff, pharmacists and others. Peck notes that these leaders observe 200 or more hand-washing cases a month, with compliance tracked by the unit and the overall hospital.
The department collaborates with infection control professionals to ensure proper cleaning of rooms where specific pathogens are present. Specific cleaning and disinfection protocols are employed for rooms where patients with methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci were treated. Staff also practice neutropenic precautions for rooms housing immunocompromised patients.
Greening up
Outside the clinical arena, Peck's team continues to make great strides in reducing regulated and nonregulated waste streams while boosting recycling initiatives. During 2011, UW Hospital and Clinics recycled 456.7 tons of materials, excluding the confidential paper waste stream that also is recycled.
The amount of infectious waste generated continues to drop despite increases in patients, beds, patient days and patient acuity. The number of tons of infectious waste the organization generates monthly was nearly halved between November 2006 and November 2011 and now stands at about 15 tons.
Last but not least, Peck has led impressive efforts to recognize staff and create leadership paths for staff ready to assume more responsibility. The creation of a senior-custodian training program has created opportunities and higher pay for those who demonstrate competency in teaching new employees.
"We take quality assurance very seriously," Peck says. "I tell all new employees, 'We're here for one reason and that's to care for our patients.' When I sit with new employees, I always tell them that our goal is to be the best in the country." That goal never changes.
Bob Kehoe is the associate publisher of Health Facilities Management.
Up to the challenge
Article By Bob Kehoe

The environmental services (ES) team at Blanchard Valley Hospital (BVH), Findlay, Ohio, is always up for a challenge.
After taking to heart some lower than expected Press Ganey patient satisfaction scores for room cleanliness and staff courtesy in 2004, the team set out to better understand what it needed to do to improve performance. Since then, its scores in these areas have more than tripled and have routinely stayed in the upper 90th percentile since 2007. The team's Hospital Consumer Assessment of Healthcare Providers and Systems scores for "always" having patient rooms clean jumped from 75 percent in 2006 to 82 percent in 2011.
The story is much the same on reducing hospital-associated infections at the 150-bed facility with more than 571,000 square feet of cleanable space. Teaming with the pharmacy, nursing, education and infection control professionals on staff, the ES team contributed significantly to the hospital's achieving a better than 22 percent reduction in hospital-associated methicillin-resistant Staphylococcus aureus rates per 1,000 patient days between 2009 and 2011. A similar effort led to a better than 50 percent reduction in Clostridium difficile cases per 1,000 patient days during the same years.
Taking ownership, getting results
Confronted with the need to reduce discharge times to boost patient flow, the team set a goal for unit secretaries to enter all discharges within 30 minutes — a 75 percent reduction in entry time. In 2011, the team and its partners in nursing achieved an 80 percent compliance rate for this target.
If there's a common thread in these achievements, it's that the ES associates have consistently taken ownership and responsibility for their performance, says Robin Cramer, environmental services/communications manager.
"We gave up time, usually a half-hour every Wednesday, to discuss issues. They elected their own team leaders, set their own ground rules and we put these challenges in front of them. They used the time to work through the processes and set the path that we needed to take to get to the 90th percentile in patient satisfaction," Cramer says.
The close proximity of Cramer's office to the infection control and prevention department, has helped to lead to a highly collaborative relationship among leadership of both groups and associates.
"It has been a godsend because not only do supervisors and Robin feel like they can stop in, but when they have their huddles, they're right near my office," says Colleen Abrams, infection preventionist. "All of their people know where I am and how to get hold of me. I look at them as an extension of my eyes and ears throughout the organization."
The ES team has taken a similarly collaborative role with nursing, creating a Hospitality Associates program. The associates can spend time with patients to help them order meals, understand how to operate the TV, how to use safety pull cords, etc. "We did this as a way to complement nursing and be in the patient's room," Cramer says. "It directly allowed us to help the family by informing them how long it would be before the patient was to go down for a CAT scan."
Using a Vocera Communications Inc. (San Jose, Calif.) system to provide more effective communications with ES staff throughout the organization, Cramer and other team leaders immediately can reach associates. It's just one more example of how the team remains accountable for providing excellent service.
"Robin and her team have developed a culture of accountability. They're accountable to their discharge times, [and] their associates are engaged so when Robin sets out the expectations, they follow through," says Kelly Shroll, director of quality and patient safety.
| Sidebar - Environmental Services Department of the Year 2012 |
WinnerUniversity of Wisconsin (Madison) Hospital and Clinics; FinalistBlanchard Valley Hospital, Findlay, Ohio; Certificate of MeritGeisinger Health System, Wilkes-Barre, Pa.; St. Francis Regional Medical Center, Shakopee, Minn.; JudgesJ. Hudson Garrett Jr., Ph.D., senior director, clinical affairs, PDI, Orangeburg, N.Y. Fiona Nemetz, CHESP, MS, director, environmental services, Northside Hospital — Atlanta, Forsyth and Cherokee Greg May, CHESP, director, environmental/linen services and sustainability initiatives, University of California San Diego Health System Doug Rothermel, MBA, CHESP, director, environmental services, St. Joseph's Hospital, Tampa, Fla. |





