In this era of closer scrutiny of cost and quality of care, patient safety is front and center even before construction starts and the design is still in the planning stage.
The stakes are higher than ever due to changes in federal reimbursement rates impacted by readmissions and patients’ perceptions of care. Adverse events, including falls, medication errors and health care-associated infections (HAIs), affect reimbursements.
Because research shows that the construction process and choice of design and materials used in a facility can impact the frequency of adverse events, builders and designers are heavily involved in the patient safety equation.
You may also like |
| Improving patient safety through design |
| Patient safety during construction |
| Cleaner and safer health care interiors |
| |
“Patient safety has increasingly become a consideration since the publication of the Institute of Medicine reports about harm in the 2000 era,” says Ellen Taylor, AIA, EDAC, director of research, Center for Health Design, Concord, Calif. “Now that outcomes are included as part of the Affordable Care Act (ACA) and reimbursement, patient safety has even more focus.”
Fortunately, an expanding base of knowledge as well as new technology and products are available to help builders and especially designers protect patients. Joint Commission construction requirements and the 2014 Facility Guidelines Institute (FGI) Guidelines for Design and Construction of Hospitals and Outpatient Facilities further inform the process to protect patients during and after the work is done.
Taylor says the FGI Guidelines for construction and design requires that a safety risk assessment be conducted early in the design process, which proves invaluable for designers. The risk assessment is conducted by an interdisciplinary team that might include facilities, interior designers, architects, infection preventionists, nurses and others, she says.
“This is for multiple patient safety components, including infection control, medication safety, falls, patient handling, injury of behavioral health [patients], security and immobility,” Taylor adds.
Similarly, the Joint Commission, Oakbrook Terrace, Ill., requires builders to conduct a Preconstruction Risk Assessment (PCRA) and an Infection Control Risk Assessment (ICRA) prior to beginning a project.
An ICRA addresses the risk of infection caused by harmful particulates that may flow from the construction site, whether outdoors or inside, to patient areas.
“You take every step possible to isolate and separate construction-related activities from patient care,” says Russ Korcuska, director of national health care projects, Kitchell Contractors, Phoenix.
One trend that benefits both patients and builders is the increased use of prefabrication for parts of the patient room or entire spaces within a facility, Korcuska says. Reducing on-site production eliminates noise and airborne particles at the construction site.
Kitchell is exploring the use of prefabrication on mechanical-electrical-plumbing racks, bathroom pods and exam rooms on a major emergency department expansion at Phoenix Children’s Hospital and built exterior walls for one project in Las Vegas, he says.
Additional resource |
 |
| The Center for Health Design has developed a comprehensive interactive microsite that shows how to use design strategies in a variety of health care rooms to improve patient safety . |
As challenging as it may be, the trick is to make construction inconspicuous. “The idea is to be as invisible as possible to the public. We try to make ourselves blend in,” he says.
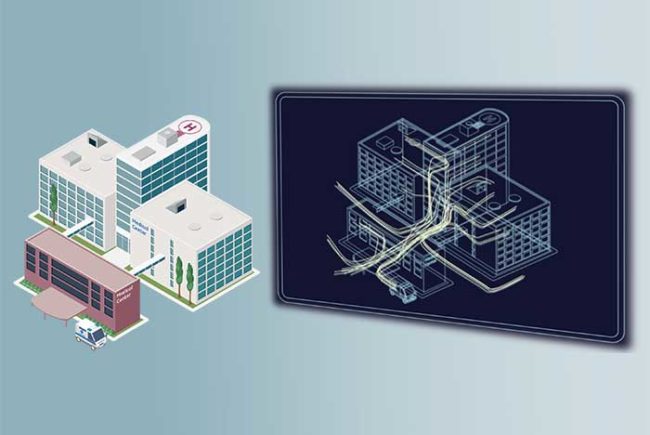
Software monitoring
Skanska USA Building achieved that objective on at least one of its projects, according to Andrew Quirk, senior vice president and national director, Healthcare Center of Excellence. HCAHPS scores at a hospital in central Ohio actually went up 2 percent during the construction project.
“We were very cognizant of proactive communication, wayfinding and cleanliness so as not to impact the daily activities of patients and staff,” Quirk says.
He also credits the success to the use of Insite, a software system that provides remote asset monitoring to aid in maintaining patient safety.
“The system allows you to monitor conditions in multiple locations on a job site. We install sensors that continuously monitor conditions — dust, noise and vibration — and send the information live to smart devices as well as record it on a dedicated server,” Quirk says.
The company sets a threshold for each condition and the system sends a notification before it becomes a problem so that corrections can be made, he says. Skanska shares the information with the hospitals where it is working.
For designers, patient safety poses a challenge because of the increasing complexity of health care facilities and the varied patient population they serve.
New products, materials and ongoing research, especially involving evidence-based design (EBD), help designers with their decision-making process.
“While the complexity may make decisions harder, the considerations become better informed,” Taylor says. “Using available research, educated designers and hospital owners can prioritize and understand the benefits and trade-offs. So, EBD plays an important role in designing for safety.”
Given this patient safety and outcomes role, a recent study reports that EBD makes good business sense, too. “Evidence-Based and Value-Based Decision Making About Healthcare Design: An Economic Evaluation of the Safety and Quality Outcomes,” a study by researchers from Cornell University, Ithaca, N.Y., concluded that investing in EBD can cost more initially and during the operation phase, but lead to fewer patient injuries and infections and generate cost savings over time.
Lead researcher Hessam Sadatsafavi, department of design and environmental analysis at Cornell, says one case study in the research showed that converting a neonatal intensive-care unit with 36 beds to single-patient rooms cost the hospital $2.7 million. The change reduced the rate of sepsis infection from 58 cases per year to 22, or 62 percent fewer, and saves the hospital about $1.7 million annually.
Research also shows that designing spaces that optimize staff efficiency and supports their workflow improves patient safety, leading to fewer medical errors, says Laurie Waggener, IIDA, AAHID, EDAC, research and evidence-based design director, WHR Architects, Houston.
“If you design to facilitate the front-line practitioners’ workplace needs, you can contribute to patient safety,” Waggener says. “If we’re providing the nurses what they need at the time they need it, that’s creating an efficient environment and it is known to reduce medical errors and expedite care delivery.”
That means supply cabinets and medication ideally should be at arm’s length in the patient room and not down the hall, she says. Less walking and searching will simplify patient care and reduce fatigue and mistakes.
Ana Pinto-Alexander, IIDA, EDAC, principal and director of health group interiors, HKS, Dallas, advocates what she calls inform-based design such as keeping the bathroom close to the patient bed and installing hand rails where feasible to reduce falls.
Rubber flooring reduces use of chemicals for maintenance and is less slippery than other materials, so it can make the room healthier and safer for patients, but doesn’t get the shine some hospitals prefer, designers say.
Carpeting offers acoustic and possible fall-reduction benefits, but needs immediate cleaning or regular replacement to satisfy patient expectations, resulting in about a 50/50 trade-off with hard surfaces, Waggener says.
Excessive floor shine is out for a host of reasons, she says. “Shiny can equal glare and glare can contribute to a patient fall. Too much glare — cumulative surface luminance — in the workplace can cause visual fatigue to workers,” Waggener says.
Lighting plays a role in patient safety, too. Correct illumination can help to reduce medication errors by staff, and systems with sensors for night lighting can reduce patient falls at night, designers say.
Seamless walls and counters can aid infection prevention by making it easier for environmental services staff to clean surfaces, Pinto-Alexander says.
Introducing no-touch technology, such as automatic door openers and faucets with sensors, reduces the risk of pathogen transmission, Waggener says. The size and location of sinks can eliminate splashing and encourage staff to practice proper hand hygiene, she adds.
Mixed reaction to antimicrobials
Use of antimicrobials in materials continues to proliferate, but they get a mixed reaction from designers because evidence of their effectiveness is incomplete. Plus, their use may send a wrong message to environmental services staff.
“We don’t want to add antimicrobials to surfaces because that’s not necessarily going to keep it clean and it may even cause staff to think that they can clean less,” says Jean Hansen, LEED Fellow, FIIDA, CID, EDAC, sustainable principal, HDR Inc., San Francisco.
For the most part, the use of copper in high-touch areas gets a vote of approval from designers because research is solid, though long-term effectiveness is unknown. Upfront cost remains a barrier for many hospitals, designers say.
That’s a misperception, according to Michael Schmidt, director, Office of Special Programs, and professor and vice chair, department of microbiology and immunology, Medical University of South Carolina, Charleston.
He was a lead researcher on a copper effectiveness study conducted for the Department of Defense and published in 2013. Results showed that there were 58 percent fewer infections in patient rooms where copper was used to cover high-touch objects such as bed rails, overbed trays and nurse call buttons compared with rooms without copper surfaces.
Considering that each HAI case costs a health care facility $43,000, or about $100 billion nationally, copper is a bargain, Schmidt says. Copper alloy added to the six objects in the patient rooms in his group’s study cost about $3,000 per room, he says.
Research into copper’s efficacy continues. Grinnell (Iowa) Regional Medical Center is conducting a clinical trial using CuVerro solid-copper alloys made by Olin Brass, Louisville, Ky. Sentara Healthcare is undertaking a clinical trial with copper surfaces and copper-embedded linens in a patient tower at Sentara Leigh Hospital, Norfolk, Va.
Sometimes, eliminating an item can contribute to infection prevention. One study shows that privacy curtains quickly become contaminated with potential pathogenic bacteria after cleaning.
A new hospital in Indiana eliminated almost all privacy curtains after Pinto-Alexander warned of their potential for contributing to HAIs. She says some European countries no longer install them for that reason, a trend she hopes will take place here.
In the end, there is no panacea that guarantees patient safety. “There are no silver bullets or easy answers,” Taylor says. “Different organizational goals, models of care, operational policies and procedures, and patient populations may warrant different design solutions,” she says.
Despite the challenges, Taylor is optimistic that education will continue to provide new solutions. “While the complexity of heath care design may make decisions harder, the considerations become better informed,” she says. “Using available research, educated designers and owners can prioritize and understand the benefits and trade-offs.”
Jeff Ferenc is a senior editor at Health Facilities Management.
Construction checklist for patient safety
The following is a list of steps builder Skanska USA Building, takes before and during a health care facility construction project to ensure patient safety, according to Andrew Quirk, senior vice president and national director, Healthcare Center of Excellence, Skanska.
Meet with health care facility leadership so everyone understands the project’s scope and to develop a plan that will protect patients. Major subcontractors are commonly included in the discussion.
Proactive management of the construction site by utilizing Insite software to monitor and manage dust, noise and vibration before it becomes a problem.
Post signage that assists patients, visitors and staff with clear and easy wayfinding.
Frequent verbal and written communication aided by use of a proprietary, customizable app called Project Corners that keeps patients, visitors and staff updated about the project.
Keep construction activities removed from regular hospital operations, specifically patients, visitors and staff. Make work as “invisible” as possible through use of barriers, fencing or temporary walls.
Offer the health care facility an opportunity to survey patients about the impact of construction on their visit. Feedback is used to change anything that patients find unacceptable.
For more information
The following resources were consulted for this article and offer valuable information regarding construction and design methods and materials to address patient safety.
• The Center for Health Design has an in-depth online safety risk assessment tool available to designers at https://www.healthdesign.org/insights-solutions/safety-risk-assessment-toolkit-pdf-version.
• The Center for Health Design also offers an online tool that includes interactive diagrams of patient rooms that give designers the ability to access evidenced-based design concepts and recommendations at https://www.healthdesign.org/insights-solutions/design-insights-strategies-tool.
• The American Society for Healthcare Engineers offers provides a way for facilities professionals to determine the level of construction-related infection prevention precautions required based on the type of construction and the risk-level of nearby patients with a tool called Infection Control Risk Assessment Matrix of Precautions for Construction & Renovation, which is available at www.ashe.org/resources/tools.
• The Facility Guidelines Institute offers more information on the 2014 FGI Guidelines for Hospitals and Outpatient Facilities at http://www.fgiguidelines.org/guidelines2014_HOP.php.