|
|
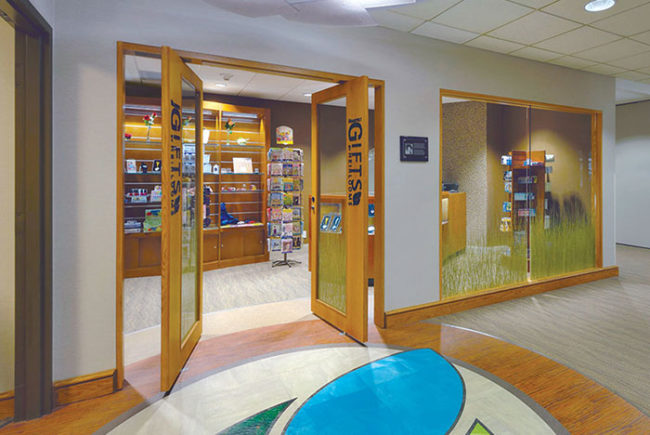
Photo courtesy of the Neenan Co. HealthProMed’s new 44,200-sq. ft. clinic addresses critical service gaps in an underserved neighborhood, where patients traditionally obtained care in the hospital emergency department by providing access to expanded care services. |
In the United States, the health care system has evolved based on insurers' reimbursement protocols. In the past, insurers' reimbursements typically followed a simple formula: the higher the acuity level of the health care setting, the higher the reimbursement. As a result, episodic illness — in many cases, the result of chronic conditions like high blood pressure, heart disease and diabetes — often was treated in the inpatient setting. Over time, this health care delivery model turned hospitals into "profit centers."
Over the past few years, this delivery model has changed dramatically as acute care costs increased and associated insurance reimbursements decreased. Health care organizations have responded by analyzing specific market needs and adjusting their supply channels to meet patients' needs at the most appropriate care setting — a hospital, clinic, primary care physician's office or one or more specialist offices. And they are increasing their focus on prevention, community health and wellness to reduce the incidence of disease.
Truly innovative health care organizations are taking a step further, employing information technology and facility design to support new models of patient care. Their goal is to transform health care services delivery – ensuring better access to care, increased quality and safety, and better outcomes for their patients; essentially, improved operational efficiency and reduced cost for their organizations. And many are succeeding.
Here is a closer look at three key strategies used by health care innovators to achieve this transformational goal: shifting care from inpatient to outpatient environments; patient-centric, wellness solutions; and the application of hospitality and Lean enterprise concepts and digital modeling to redefine health care operations and redesign facilities.
Shifting care from the hospital and emergency department to outpatient environments
Hospitals are anchored in tradition and process. Health care organizations must make strategic and operational changes to enable the shift to non-acute patient care, when medically appropriate, from the hospital to outpatient environments. They must analyze the unique needs of each of their markets and deploy their resources accordingly.
Payment, technology and patient-access forces have powered this change. In particular, the high costs of emergency department (ED) visits for routine care and in-hospital surgery admissions for noncomplex procedures are the impetus for the rise of urgent care centers and the accelerated growth of outpatient surgery centers. In both instances, payment structures are motivators; additionally, innovation in technology, care protocols and facility design enable the shift. Changes in physician referral strategies and patients' improved service access have contributed to making the shift possible.
For example, HealthProMed built a new outpatient urgent care clinic in San Juan, Puerto Rico, with the specific goal of addressing critical service gaps in an underserved neighborhood, where patients traditionally obtained care in the hospital ED. A review of the data indicated that a vast majority of the hospital's ED visits could have been treated in an outpatient setting, underscoring the waste of professional resources and the exorbitant cost of delivering primary and urgent care in an acute care setting.
Patients also have access to expanded care services at the new 44,200-sq. ft. clinic, including primary care, diagnostics, lab, dental and mental health services. Wellness and health education programs were also introduced to help patients prevent illness and manage common chronic conditions like high blood pressure, heart disease and diabetes.
HealthProMed's performance data are evidence of the benefits:
- The number of patient visits has increased from approximately 50,000 to 75,000.
- The number of patients served has increased from 14,000 to 16,000.
- The number of providers has increased from 10 to 15.
- The number of staff supporting wellness and education programs has increased from 15 to 25.
Patient-centric solutions: the patient-centered medical home and wellness model
Health care organizations are shifting from provider-centric to patient-centric models of care. The patient-centered medical home is a way of organizing primary care that emphasizes effective communication among patients and caregivers and coordination of all facets of a patient's care. Medical homes have the potential to provide higher-quality care at lower costs, and to improve the experience of care for both patients and providers.
 |
|
Photo courtesy of the Neenan Co. Sutter Gould Medical Foundation’s Turlock Care Center operates on the principles of a patient-centered medical home. The care center offers urgent care, family medicine, internal medicine, pediatrics, specialty care, radiology and laboratory services. |
A patient-centric medical facility locates patient registration and discharge at the point of care and not at the front desk. Similarly, it brings services like phlebotomy, ultrasound and portable diagnostic imaging to the patient instead of sending the patient out for these services.
This model requires a reorganization of the traditional roles and responsibilities into a collaborative care team, which integrates health care providers and support staff under new protocols, responsibilities and tasks. The care team model reduces the number of staff positions, including appointment scheduling, reception and discharge, increasing efficiency and reducing costs. More importantly, it enables comprehensive coordination of the patient's care along the entire continuum of care — over time, among various places of service, and among various providers — and introduces new health education, wellness and counseling programs.
Effective use of electronic health records (EHRs), other digital technologies and performance metrics support this operational shift. These new tools are transforming health care delivery from patient access and diagnostic testing to generation of billing and performance metrics.
A patient call center or service portal (accessed by telephone, often via a toll-free number, or via the Web) is essential for this new operational model, serving to integrate appointments, medical records, triage, performance metrics and communication processes. Access to digital information enhances productivity and transparency. The new electronic data bank is HIPAA-compliant and satisfies portability needs.
These tools and processes also create vastly different patient and staff flows, which require innovative space solutions.
For example, the Sutter Gould Medical Foundation's Turlock (Calif.) Care Center, which opened in August 2014, operates on the principles of a patient-centered medical home. The care center offers urgent care, family medicine, internal medicine, pediatrics, specialty care, radiology and laboratory services.
The Turlock Care Center optimizes the use of EHR technology, Lean workflow processes and architectural solutions that sustain care team operations, including the concentrated point-of-care approach. Digital tools continue to be introduced to improve diagnostic and treatment protocols.
The Turlock Care Center is supported by a central patient navigation and information center, which is staffed at 0.5 per provider. Compared with the traditional distributed appointment system and patient triage/information center, the patient call center is a far more efficient way to manage patient flow and pre-visit and post-visit data.
Applying hospitality and Lean enterprise concepts and digital modeling to redefine health care
Sutter Gould Medical Foundation is projecting improvements in the application of hospitality and Lean enterprise concepts and digital modeling to redefine health care operations and redesign facilities.
 |
|
Photo courtesy of the Neenan Co. The Turlock Care Center optimizes the use of electronic health record technology, Lean workflow processes, and architectural solutions that sustain care team operations. |
As part of the transformation of health care into a patient-centered, efficient process, innovative health care organizations have adopted best practices from the hospitality industry and Lean enterprises.
The hospitality industry is a worldwide leader in customer focus and guest satisfaction. It has created customer-centered services, as well as expanded guest services menus, such as cafeteria, fitness, office center and concierge. The industry also has introduced architectural and interior design innovations to improve the guest experience, including universal access (for able-bodied and disabled guests), better wayfinding, greater privacy and comfort, broadband digital connections and environmental sustainability.
Innovative health care organizations are adopting many of these hospitality concepts to increase market share and improve patient satisfaction.
The Lean enterprise movement, which originated in the automobile manufacturing industry, has swept across all industries, and has applied the concepts to eliminate all forms of waste and achieve continuous improvement in performance. As a result, they have increased efficiency, profitability and customer satisfaction.
Innovative health care systems are applying Lean concepts through digital modeling technology to redefine operations and redesign facilities. Digital modeling enables 3-D visualization of facility design and operational variables, such as patient flow and physician/staff workflow, and quantify (4-D and 5-D) the effects of design and operational alternatives on their objectives. These organizations are finding many opportunities to use modeling and the associated performance data harvested from models. These include: anticipating the impact of moving from paper to digital work environments; testing and improving building performance and sustainability (e.g., energy efficiency); assessing staffing needs and redefining skill sets; and developing efficient just-in-time supply chain processes.
Hospital leaders have used Lean concepts and digital modeling to redefine their organizations and work processes and redesign facilities to support their migration from the traditional distributed model — a private office, exam room(s) and medical assistant for each physician — to a collaborative, care team model, achieving the objectives for safety, quality, access, efficiency and cost as a result.
For example, St. John's Clinic in Rolla, Mo., built a new three-story, 106,862-sq. ft. outpatient facility to house a multispecialty clinic practice, an ambulatory surgery center and other outpatient services. They collaborated with their design-build team in applying Lean concepts and modeling tools to support the transformation of the traditional provider-centric operations into a patient-centered care team model and to design a facility that supports the new operations. Innovations included elimination of private physician offices as well as the reception and the waiting room, while adding in shared provider work spaces, and point-of-care patient registration, services and discharge.
St. John's performance data show the gains in productivity and efficiency compared with that of a traditional model:
- Overall building: total space reduction of 13 percent (from 124,167 sq. ft. to 106,862 sq. ft.)
- Overall clinic space: reduction of 20 percent (from 76,945 sq. ft. to 61,113 sq. ft.)
- Initial construction savings: $3.8 million
- Overall capacity: increase of 16 percent (from supporting 49 providers to supporting 57 providers)
- Annual rent savings: approximately $450,000
- Annual operational savings: approximately $183,000
- Annual savings per provider: approximately $3,400 per provider per year
- 50 percent increase in recruiting success
It's not just about cost
With total U.S. health care expenditures above 17 percent of the gross domestic product, American health care innovators have developed and applied these three strategies out of economic necessity to deliver health care at a lower cost. But as these strategies are put into place, health care innovators have seen improvement in quality, safety and patient satisfaction by increasing health care access, expanding services and growing capacity.
Miguel Burbano de Lara, AIA, NCARB, served as AIA Colorado North Chapter president in 2005 and is a member of many professional and civic organizations. He has worked at the Neenan Co. since 1999, where he focuses on Lean theory, design innovation and accelerated delivery. For more information, visit www.neenan.com.