About the 2014 Emergency Management SurveyHealth Facilities Management (HFM), the American Society for Healthcare Engineering, the Association for the Healthcare Environment, and the Association for Healthcare Resource & Materials Management surveyed a random sample of 911 hospital and health system executives to learn about trends in health care emergency management. The response rate was 10.6 percent. HFM thanks the survey sponsor, Grainger, Lake Forest, Ill. How this survey was conductedThe online Emergency Management Survey, conducted in April 2014, comprised 21 questions on emergency management including current procedures and policies on preparation for tornadoes, hurricanes, earthquakes, floods, winter storms, tsunamis and other natural disasters. It also included questions about terrorism preparedness and mass casualties, adequacy of emergency supplies and equipment, and recent emergency events. Of the respondents, 88 percent said they are members of their facility's emergency management/disaster preparedness team and 91 percent said they worked for a hospital or health system. About a third of respondents were in rural areas, 30 percent in urban areas and 23 percent in suburbs. The states with the most respondents were California, Pennsylvania, New York, Texas, Florida and Illinois. |
Over the past five years, hospitals in nearly every region of the country have been challenged by extreme weather. Hurricane Sandy; the Joplin, Mo., tornado; upper Midwest flooding; and crippling winter storms across the East, Midwest and South are just a few examples of unpredictable and tragic natural events that have required hospitals to plan for the worst.
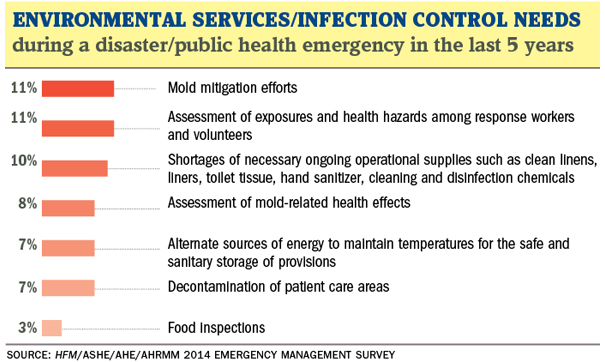
And natural events aren't the only threat. In January, a hazardous chemical spill into a West Virginia river sent more than 30 people to area hospitals and caused state authorities to deem the water undrinkable and unusable for medical procedures. The incident led Charleston Area Medical Center to enact its emergency response plan and forced hospital leaders to replace the average 7,200 gallons of water the facility uses each weekend for patient care.
Throughout these incidents and others like them — from hospitals temporarily losing power to disasters involving mass casualties and total facility destruction — health care organizations have learned valuable lessons and implemented important changes to help them better prepare for future emergency situations. Some of the lessons:
• Even the best-laid communication plans among internal and community partners can be improved, and it often takes a real-life emergency to pinpoint weak spots in plans.
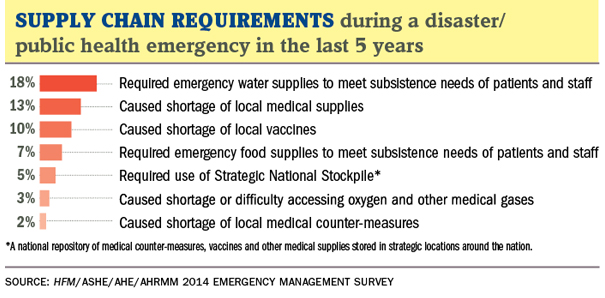
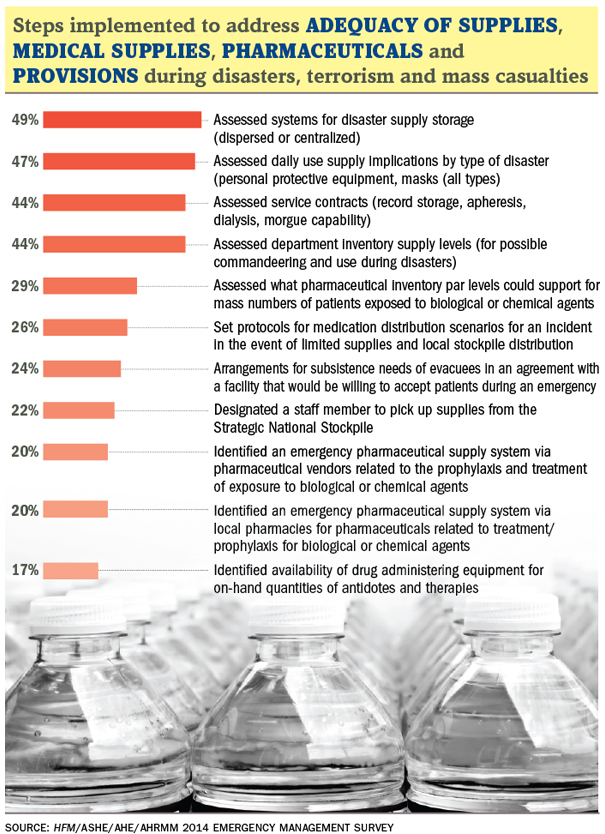
• All area resources that can be utilized in an emergency should be identified. This includes mapping out all supply chain logistics for ensuring that wireless communication, water, food, bedding, linens, fuel for generators and other items can be brought quickly on-site.
• Emergency exercises should be coordinated carefully with local authorities, including public health systems, if an organization is to perform optimally during an emergency situation.
• Surge capacity contingency plans should cover sleeping accommodations and other needs of staff when they must remain in place.
These are just some of the key points underscored by respondents to the first Emergency Management Survey conducted jointly by Health Facilities Management, the American Society for Healthcare Engineering (ASHE), the Association for the Healthcare Environment and the Association for Healthcare Resource & Materials Management (AHRMM). The survey was sponsored with an unrestricted educational grant from Grainger, Lake Forest, Ill.
Stormy weather
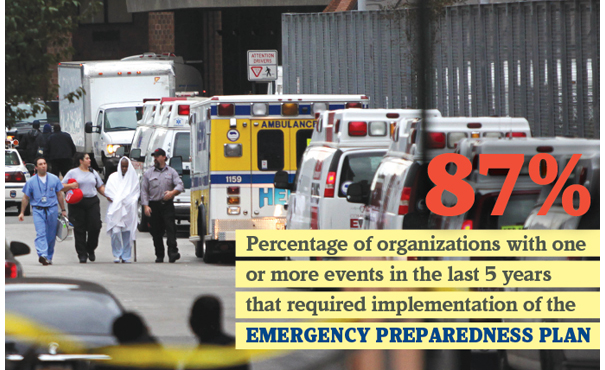
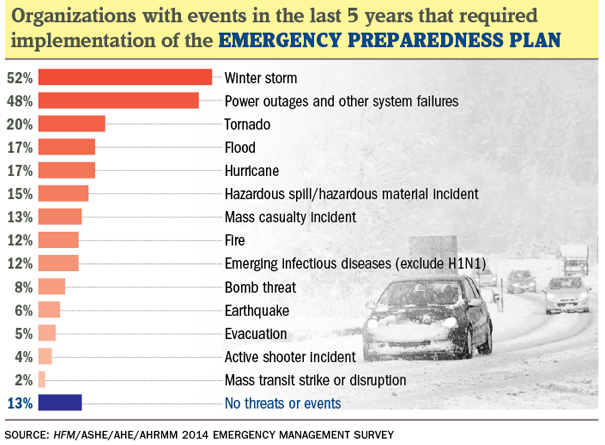
In all, more than half of survey respondents — 52 percent — said they had experienced a winter storm in the past five years that required implementation of their emergency operations plan.
Meanwhile, 48 percent said a power outage or system failure required activation of emergency management protocols. And 20 percent and 17 percent, respectively, indicated tornado and hurricane as initiators of emergency operations plans in the past five years.
In a related question, 58 percent of respondents said they went to emergency power in the past five years because of an emergency event.
Winter storms were among the most common emergency situations. In January, for example, a winter storm brought the Atlanta region to a standstill, and required hospitals to activate their emergency plans. Fiona Nemetz, CHESP, director of EVS, security and safety for 537-bed Northside Hospital in Atlanta, said the snowstorm showed the importance of thinking about the hospital in the greater community context.
"During a storm, people who aren't sick or injured come to the hospital because it is a place to stay warm and dry," Nemetz says.
Contingency planning
Many people in the Atlanta area were stranded on the roads, at work and at schools on that day. Many who were at the hospital for outpatient surgery had no way to get home because the roads were closed. Additionally, staff couldn't get home so they also stayed at the hospital. Ultimately, the hospital collaborated with local police to assist with transportation needs.
"Don't limit yourself to preparedness for patients," advises Nemetz, who grew up in the Bahamas so is no stranger to natural disasters. "You need to look at your employees, too, as well as the needs of the community during a disaster."
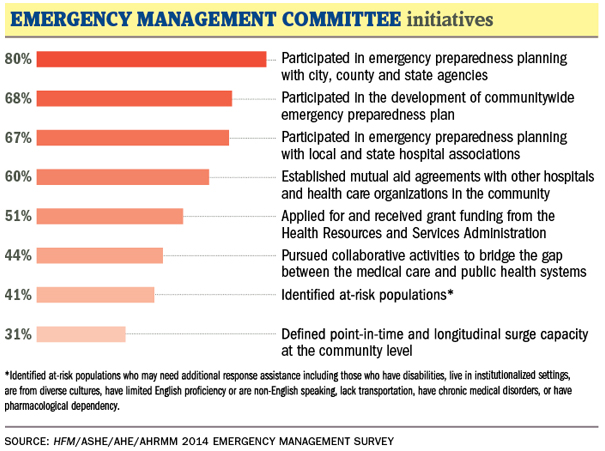
Collaboration with local authorities and other health care facilities is required by the Joint Commission. The vast majority of survey respondents — 80 percent — said they had participated in emergency preparedness planning with city, county and state agencies. And nearly 70 percent said they conduct emergency planning with local and state hospital associations and have developed communitywide preparedness plans.
Sixty percent said they have established mutual aid agreements with other hospitals and health organizations. Less common is pursuing collaborations to bridge the gap between medical care and public health systems, at 44 percent; identifying at-risk populations, 41 percent; and defining point-in-time and longitudinal surge capacity at the community level, 31 percent.
Michael Schiller, CMRP, director of supply chain at AHRMM, says hospitals should seek greater integration within the community, including nontraditional partnerships with hotels and restaurants, which can supply food and linens during emergencies.
"The more you reach out and work with the community, the better prepared you will be," Schiller says. "Are we looking outside the walls of health care to identify all the resources available?"
In situations in which a hospital must evacuate rather than take in patients, the majority of hospitals in the survey have policies and procedures in place to make that happen. Sixty-four percent of respondents have arrangements with other hospitals to receive patients and 55 percent have a system of medical documentation that preserves patient information and ensures privacy and security. Some 43 percent have electronic health records backed up both inside and outside of the immediate geographic region, while 41 percent said they have logistical assets to transport mass casualties to collection points and other facilities.
"These are high numbers," remarks Chad Beebe, deputy executive director of advocacy at ASHE. "This is where you see the success of hospital response to Hurricane Sandy. You can see that a lot of evacuation protocols are in place, and Sandy response reflected that."
Roughly 1,300 patients were evacuated from New York and New Jersey hospitals during 2012's Hurricane Sandy, the second costliest hurricane in American history.
"If you look at what happened during Hurricane Sandy, the success of evacuations without injuries or death is pretty remarkable," Beebe says.
Lines of communication
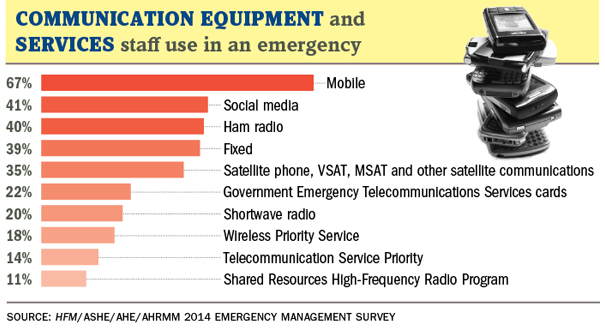
Communications equipment is a hot topic in emergency management, and survey respondents use a variety of phones and other devices during emergencies. By far, the largest usage was via smartphones and other mobile phones. In the event of an emergency, 67 percent of respondents said they use mobile devices, while 41 percent said they use social media.
Close to 40 percent use ham radio and fixed radio, and 35 percent use satellite phones. Respondents could choose all that apply for this question. In open-ended comments to this question, many respondents said they had two-way radios and emergency radios on hand.
Schiller of AHRMM says he was surprised by the high response rate for mobile devices. "I don't think people should be banking on these working during an emergency," he said. "This was one of the biggest things that struck me in this survey. In true emergency planning, you have to expect there will be no IT available."
Caution about the reliability of mobile phones was reflected in comments by one survey respondent, who wrote: "One of the biggest lessons was in IT/communications outage due to cut fiber-optic lines. We found out no matter how much you think you are ready, a hospital runs on IT. We have beefed up some of our systems, but are still vulnerable to the same scenario because of being in a rural location. In our case, the cut actually took out all but one major cellular carrier so the only communication we had was good old-fashioned, hard-wired analog emergency phones."
Some hospitals and health systems have embraced a variety of communication systems in addition to mobile devices for emergencies.
Sanford Health, based in Sioux Falls, S.D., is hooking up its incident command centers in five states to iPads using state grant funding. The system allows emergency response teams to be out monitoring disaster events and reporting back to command centers in real time. It also allows staff in other locations to run incident command if one location isn't able to manage an event, and help to divert resources to the troubled site.
Sanford Health, serving the Dakotas, is no stranger to natural disasters. Ellen Rasmussen is manager of emergency preparedness for Sanford Medical Center in Fargo, N.D., a city that experiences annual flooding from the Red River. The hospital was last evacuated due to flooding in 2009. Each year, the hospital starts flood preparation in January and finishes in mid-April.
"When flooding happens in North Dakota, it's so flat that it can take weeks for the water to recede," Rasmussen explains. "We do a lot of flood planning."
Rasmussen said the iPad project is just one part of a multifaceted communication plan for Sanford Health. In Fargo alone, for instance, there are 27 ham radio operators. All participate in the hospital's annual flood preparedness planning, and they have a ham radio station on-site at the hospital.
Additionally, North Dakota has a bioterrorism communication network that includes all hospitals and public health departments. It works like videoconferencing, but it is on its own network and operates independently of local power sources. The hospital also keeps 14 days' worth of supplies on hand, and has its own water pump system separate from the city of Fargo. "During flooding, we close the gates that connect us to the city and we go to our own pump system," Rasmussen says.
Some other hospitals are introducing ham radios as well. A tornado and storm in April 2011 in Alabama caused one hospital to install a ham radio in its incident command center. "We had two visible tornadoes that could be seen from the hospital windows at various times of the day," the respondent wrote. "We were also being inspected by the Joint Commission on this date. The list of things we learned was lengthy."
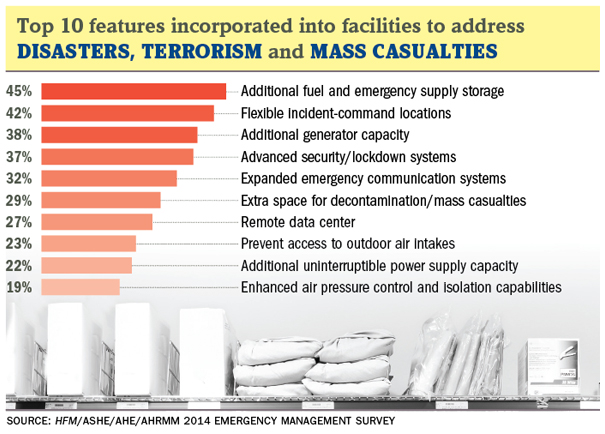
Like communication, many hospitals have added infrastructure resources to address disasters, terrorism or mass casualties. Forty-five percent of respondents have additional fuel and emergency supply storage, while 42 percent have flexible incident command centers and 38 percent have additional generator capacity.
"Contingency planning is an increasingly important consideration across a wide range of enterprises," says Kym Orange Jr., manager of Grainger's health care marketing segment. "During emergency situations, hospitals must be able to rely on their established partners to communicate with them effectively so that they can better prepare, respond and recover from these situations safely and quickly."
Meanwhile, 37 percent of respondents have advanced security and lockdown systems. Beebe says active shooters, or lone gunmen, are a hot topic in health facility management today. Hospitals are looking for ways to protect staff and patients from random shootings in the wake of the Sandy Hook Elementary School massacre in Newtown, Conn., in December 2012 and the University of California Santa Barbara drive-by shootings in May. In the survey, 38 respondents out of the total 911, or 4 percent, said an active shooter incident had resulted in emergency operations plan activation in the past five years.
Preplanning can stop incidents from escalating, according to Ryan Tuchmayer, emergency preparedness and response manager at Cedars-Sinai Medical Center in Los Angeles. "Early activation of the hospital incident command system can prevent small incidents from turning into large emergencies," Tuchmayer responded on the written portion of the survey form. "This also allows for earlier control of situations. Single utility failures can have cascading effects. For instance, loss of water will result in loss of HVAC and eventually power; loss of HVAC will close clinical and support areas."
Exercising the plans
A common theme of respondents was the importance of exercising the plans that are put in place, and the challenges in doing so.
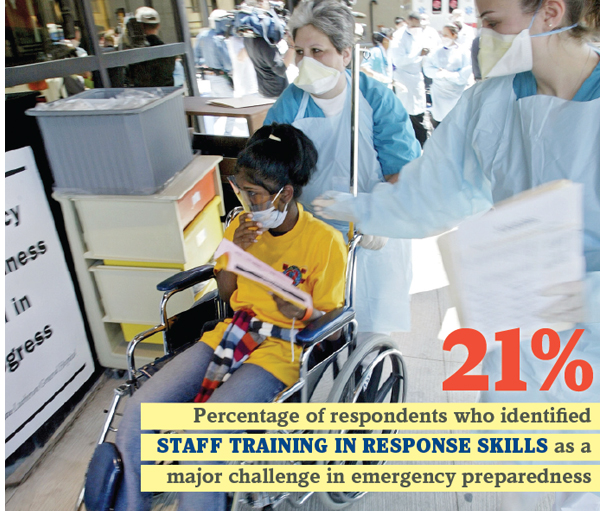
Even with all the equipment and planning available to Sanford Health, Rasmussen says there is room for improvement. "Staff training is a huge challenge for us," she says. "It can cost the health system a lot of money in time for staff to be away from the job in training."
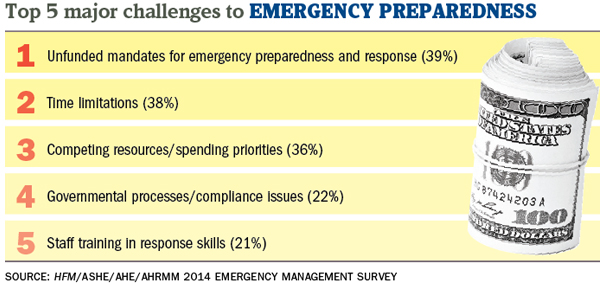
Twenty-one percent of respondents identified staff training in response skills as a major challenge in emergency preparedness and another 54 percent said it was a minor challenge. The largest challenge identified among respondents was unfunded mandates for emergency preparedness, with 39 percent calling this a major challenge.
One survey respondent commented: "Each activation of the emergency operations plan includes an after-action review that results in a corrective action plan. These plans have identified improvements for communication, emergency lighting, surge capacity, fatality management and staff support services."
Nemetz of Northside Hospital in Atlanta identified one training challenge as making sure off-shift staff are as prepared as day-shift workers because fewer drills are generally scheduled for off-shift workers.
The preponderance of written comments from survey respondents makes clear the importance of overcoming such obstacles to reap the benefit of emergency management drills:
- "You can never be prepared enough or practice enough."
- "We treat emergency management and response as a continuous learning process and have always taken away lessons learned during the critiques of both our drills and our real-world responses."
- "You must practice and check and recheck your readiness."
- "You can be general in your writing of the emergency management plan, but you must drill for specific disasters."
- "You can never train too much or too often."
- "[Tabletop exercises] do not work because they do not find the flaws in the system and they do not take into consideration real human actions at the time."
"You get better every time you activate your plan," agrees Susan B. McLaughlin, FASHE, CHFM, CHSP, founding partner of MLS Healthcare Consulting, Barrington, Ill., which helps hospitals get up to speed on emergency management and other regulatory issues. "That is an important thing to remember."
Rebecca Vesely is a freelance writer based in San Francisco. Suzanna Hoppszallern is senior editor of data and research for Health Facilities Management's sister publication, Hospitals & Health Networks.
Hospitals adopt multifaceted approach to preparedness
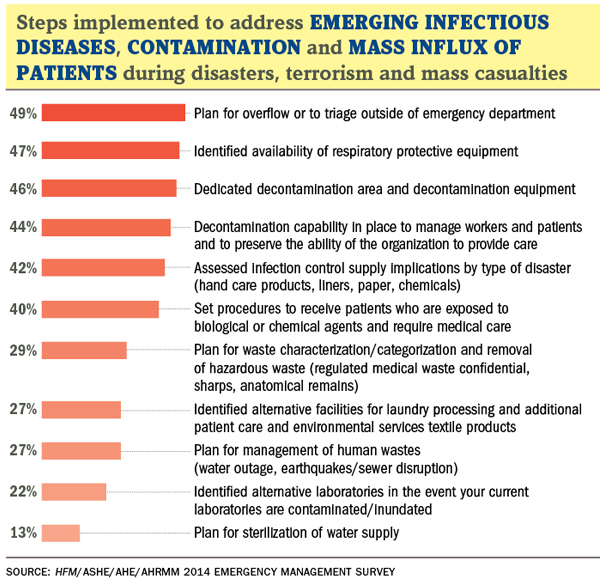
Emergency department (ED) design has incorporated multiple features to address disasters, terrorism and mass casualties, according to Health Facilities Management's 2014 Emergency Management Survey.
But the features widely adopted tend to be those that serve functions well beyond emergency management, according to survey results.
For instance, more than half of respondents — 56 percent — said they have in place information technology systems that can track patients and patient records in real time. Another 12 percent of respondents said they plan to implement these systems in the next 24 months. And 33 percent said they have the ability to share encrypted data with sanctioned medical, public safety, military and governmental agencies. Ten percent said they plan to implement this feature in the next 24 months. The ability to securely collect, store and share patient records is largely a result of achieving meaningful use requirements of electronic health records.
Cross-contamination and cross-infection prevention safeguards are also popular features, with 45 percent of respondents saying they already have this in place, and another 8 percent saying they plan to implement in the next 24 months. Infection control is also an important part of payment reform. In 2008, Medicare stopped reimbursing providers for health care-associated infections and conditions, and private insurers followed suit.
Facilities seem split on the value of some emergency management features for the ED. For instance, about 43 percent said they have radiation detection in their EDs, while 28 percent said they have no plans to implement this. Similarly, 39 percent said they have modular scalability to serve many patients on a daily basis and then expand to larger numbers in minutes, while 28 percent said they have no plans to implement.






