About the Health Facility Design Study |
|
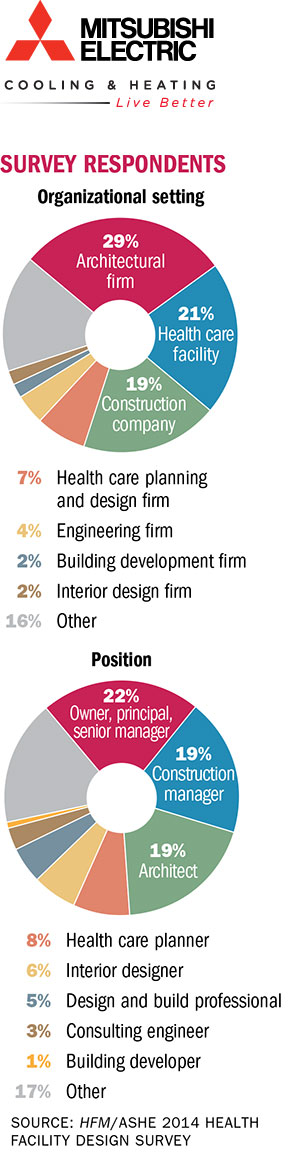
Health Facilities Management (HFM,) and the American Society for Healthcare Engineering of the American Hospital Association surveyed a random sample of 9,370 health care architecture, facilities and construction professionals to learn about trends in health care design. The response rate was 6.2 percent. HFM thanks the sponsor of this survey: Mitsubishi Electric Cooling & Heating. |
Enhancing operational efficiencies, improving patient and caregiver safety and integrating health information technology (IT) are major influences driving changes to health care facility design, according to the Health Facilities Management/American Society for Healthcare Engineering 2014 Health Facility Design Survey.
The Affordable Care Act (ACA) is having a major impact on nearly every aspect of health care — and facility design is no exception, according to the survey, which was completed online by 582 participants in July.
Enhancing efficiency
“The biggest thing that surprised and excited me was the word ‘efficiency’ and the major focus on technology,” says Andrew Quirk, Skanska USA senior vice president and national director of its Healthcare Center of Excellence. “Those were the two big ideas circulating through this survey.”
Enhancing operational efficiencies edged out improving patient and caregiver safety and improving patient satisfaction as the top factor in driving changes in health care facility design, with 91 percent, 89 percent and 88 percent of respondents, respectively, choosing these as the major influences.
The ACA is causing hospitals to seek all possible ways to become more efficient, and to provide better care and service to the community, Quirk says. “It was a perfect storm of the economic downturn, reimbursement cuts and the Affordable Care Act. Fiscally, you just have to be more responsible, and building facilities has gotten more expensive.”
The ACA’s focus on reforming payment models from volume-based care to value-based care is “a very strong driver for facility design in the near future,” says Joseph G. Sprague, FAIA, FACHA, FHFI, principal and senior vice president at HKS Inc. an architectural/engineering firm in Dallas.
With the rise of accountable care organizations and other payment-reform models brought to the fore by the ACA — as well as non-reimbursement for never-events and greater transparency on medical errors — patient quality and safety are more paramount than ever, experts say.
As for the focus on patient satisfaction in design, intense competition for customers is one factor. Additionally, patient satisfaction scores are playing a greater role in reimbursement, so more attention is being paid to making sure patients and families have a good care experience than ever before.
“There are very few fundamental drivers in health system facility design,” says D. Kirk Hamilton, FAIA, FACHA, EDAC, professor of architecture at Texas A&M University, College Station. “Hospitals look to improve efficiencies wherever they can; far too many patients suffer from infections or safety issues; and transparency in reporting is something we are seeing more than ever before.”
Some prior trends seemed to be old hat this year. For instance, a third or fewer respondents said that hospital mergers (33 percent) and acquisition of physician practices (31 percent) are important factors driving change. Aside from a few notable exceptions, most communities already have experienced large hospital mergers in years past, so these are not current design issues.
“Our health networks are pretty well-established,” says Scott Reifeis, director of design and construction at Nationwide Children’s Hospital in Columbus, Ohio. “What is happening is more movement into communities and building ‘hospitals within other hospitals’ to serve neonatal patients.”
Outpatient facility design was a hot topic in the design survey results [see sidebar, Page 24]. Some 60 percent of respondents said that creating “facilities that are easy for the community to access” was a major influence in design.
“Some things we do to improve safety and satisfaction are counter to improving efficiencies,” Reifeis says. “When we look at a design challenge, we have to have balance. We balance patient experience, cost and available space with efficiencies.”
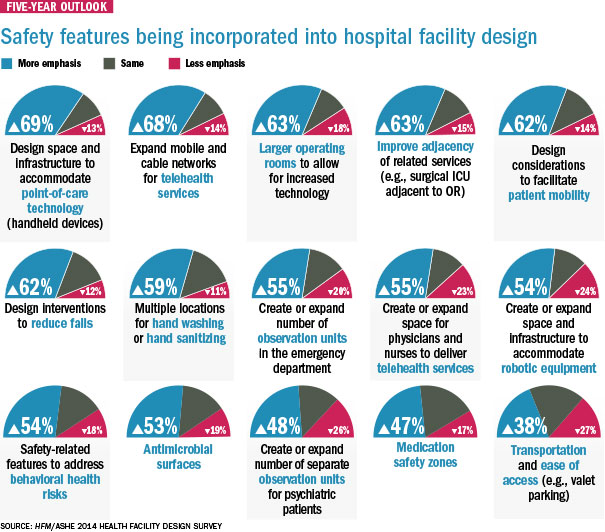
A safe experience
Patient safety and patient experience features will have a big influence over facility design in the next five years, including design interventions to reduce falls (62 percent), design considerations to facilitate patient mobility (62 percent) and multiple locations for hand sanitizing and hand washing (59 percent).
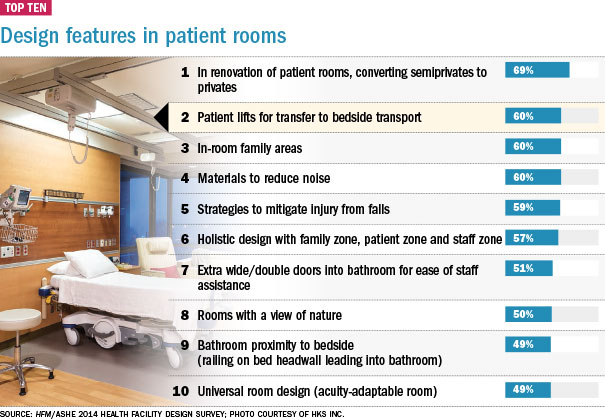
Making rooms accessible and safe is a major trend, says Sprague. “One of the biggest challenges I see is that you have a situation where you need motivation and mobility to move from the patient bed to the toilet area,” he says. “Handrail placement and ways to reduce falls are really strong considerations in the design of the patient room.”
Hamilton says he would like to see more emphasis on infection prevention, especially in light of major worldwide outbreaks like Ebola. “I would have bet that there would have been more emphasis on infection prevention,” Hamilton says. “The physical environment plays a role, but I would have liked to have seen more about antimicrobial materials like copper.”
Slightly more than half (53 percent) of respondents said antimicrobial surfaces would have an emphasis in hospital and facility design over the next five years.
Fifty-five percent of respondents said that creating or expanding observational units in the emergency department or for psychiatric patients (49 percent) would be a priority over the next five years.
William Hercules, AIA, FACHA, ACHE, LEED AP, president of WJH in Orlando, Fla., expresses surprise that it wasn’t higher. “Emergency departments are in a transformational stage,” Hercules says. “I believe the number of observation beds is going to increase because the amount of care and its associated expense is higher if patients ultimately are admitted as inpatients.”
Some are moving forward with additional psychiatric beds, like Nationwide Children’s Hospital, which is opening a 16-bed behavioral health unit for patients younger than 18 within the next year. “We look at this as a responsibility to the community,” Reifeis says.
Rise of technology
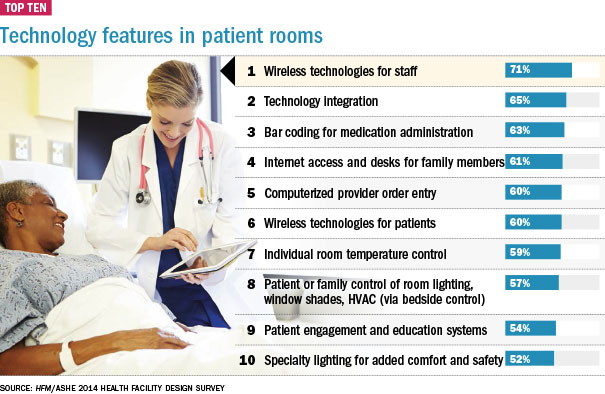
Technological advances and investments in IT were high on the list of factors driving change in facility design, with 72 percent and 65 percent of respondents, respectively, having said these are major influences. Over the next five years, respondents said the following IT features would be incorporated:
• Design space and infrastructure to accommodate point-of-care technology (handheld devices);
• Expanded mobile and cable networks for telehealth services;
• Larger operating rooms to allow for increased technologies;
• Created or expanded space for physicians and nurses to deliver telehealth services;
• Created or expanded space and infrastructure to accommodate robotic equipment.
Technology is driving the health care industry and that is increasingly reflected in design, says Quirk. “But I’ve never seen technology integrated into the architecture of the facility,” he adds.
“How does a facility change to reflect technology? Does the room change if you are walking into it with an iPad? Do the buildings that we now have in service respond to the technology sea change happening?” Quirk asks. “A lot of buildings can’t adapt to this new environment. But you will see a blending of technology and architecture. It’s a huge opportunity.”
Likewise, Reifeis says he was surprised that more respondents did not see robotics as a major factor in the next five years. “I think robotics will come on strong in the near future,” he says. “I believe we will see robotics used to deliver food carts and move trash. It is an opportunity to improve efficiencies and reduce costs.”
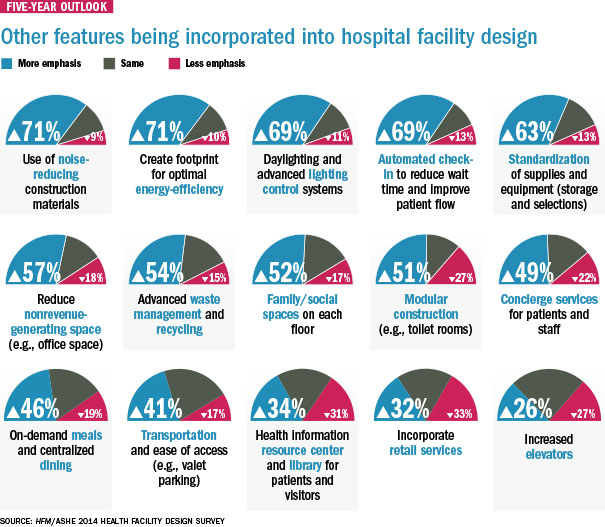
Another emerging trend may be modular construction, with 51 percent of survey respondents saying they plan to put more emphasis on modular construction over the next five years.
“Modular construction has a bright future,” Sprague says. “A lot of large hospitals are looking at prefab toilet rooms because they can save money on construction costs.”
Patient comfort
Not surprisingly, noise reduction in hospitals is top of mind in hospital facility design. Some 71 percent of respondents said that over the next five years noise-reducing construction materials would be incorporated into design features. And 60 percent of respondents said they are incorporating noise-reducing materials into patient room design.
Noise reduction is an area of focus because of the increased emphasis on patient satisfaction and Facility Guidelines Institute (FGI) Guidelines for Design and Construction of Hospitals and Outpatient Facilities issued earlier this year that has a new section on acoustics, including the use of noise-absorbing materials and reducing the amount of hard surfaces in facilities, which can create unnecessary noise, Sprague says.
The FGI is a volunteer-run organization and its guidelines, published every four years, are used by 40 states as a hospital licensure requirement. “It’s amazing how noisy hospitals have become,” Sprague says.
To that point, 71 percent of survey respondents said that regulatory requirements are a major influence in driving change to health care facility design. Another FGI guideline involves medication safety zones to reduce medication errors. This can include guidelines on lighting, security and access, Sprague says. Nearly half of survey respondents (48 percent) said they would put more emphasis on medication safety zones over the next five years.
Top features in room design include wireless technology for staff (71 percent), conversion of semiprivate to private rooms (69 percent), technology integration (65 percent) and bar coding for medication administration (63 percent).
Other items that could influence patient satisfaction include individual temperature control (59 percent) and patient control of room lighting and shades (57 percent). “That’s a lot,” Hamilton says of the results. “The research shows these are helpful in terms of patient satisfaction.”
An important aspect of facility design these days is energy efficiency because it can reduce overhead costs, some experts said. For instance, 68 percent said better energy usage and efficiencies were a major influence in driving changes in facility design. However, just 37 percent of respondents said that selecting environmentally friendly materials was a major influence in design.
“Energy is the biggest opportunity to make an effect on the financial well-being of a hospital,” says Quirk. “It gives you better control over swings in commodities like gas, water and electricity. Hospitals and health care organizations need to push the industry and, on the client side, clients need to be willing to take professional recommendations and step up and take a little bit of a risk.”
Improving the process
Process improvement is an underlying theme in health facility design today — from improving patient flow to reducing unnecessary steps and tasks for staff. All improve the patient and caregiver experience and can improve quality, Sprague says.
“Everybody is interested in process improvement,” he explains. “You don’t want to design a building with an old, inefficient process.”
is a freelance health care writer based in California. is a senior editor of data and research for Health Facilities Management’s sister publication, Hospitals & Health Networks.
Respondents report interest in outpatient facility designs
Hospitals and health systems are paying careful attention to outpatient facility designs these days to improve care coordination and meet the multifaceted needs of patients while extending their brands, according to the 2014 Health Facility Design Survey.
A major trend emerging over the next five years is expanded health system-branded general medicine and family care centers in the community, with 63 percent of respondents having said this change is on the drawing board.
“A consistent brand across the continuum is a major trend,” says William Hercules, AIA, FACHA, ACHE, LEED AP, president of WJH in Orlando, Fla. “If hospital systems are now going to be responsible for the overall health of communities, they have to be responsible for the continuum of care for an illness or an event. So outpatient settings are only going to be called outpatient settings within the health system. To the community, hospitals are trying to make it look seamless.”
So-called “intermediate care” facilities — community-based facilities for patients well enough to leave the hospital, but too sick to go home — are one such area that hospitals and health systems are exploring, with 45 percent of survey respondents having said this is on the drawing board for the next five years.
Children’s Hospital Nationwide in Columbus, Ohio, for instance, is investigating intermediate care, says Scott Reifeis, director of design and construction. “The adult market has a lot of these types of facilities, but it is just emerging in pediatric care.”
Nearly half of respondents (49 percent) said that rehabilitation centers are on the drawing board for the next five years as well.
Any unfulfilled needs expressed by patients are driving outpatient trends because of an increased focus on consumerism and patient satisfaction, experts say.
“The patient really is now the consumer,” says Andrew Quirk, senior vice president and national director for Skanska USA’s Healthcare Center of Excellence. “Everyone is starting to shop for the delivery of health care. Everyone better deliver the quality and price. Now you have to brand yourself.”
More than half of survey respondents (54 percent) said that expanded immediate care facilities like urgent care are on the drawing board for the next five years. Urgent care is another area of focus for the consumer — allowing them to see a physician quickly at a convenient location near home or work.
Additionally, expanded health system-branded clinics in retail spaces like strip malls, corner stores or big box retailers is another emerging trend, with 43 percent of respondents having said this is on the drawing board for the next five years. And 36 percent said retail health centers are on the drawing board as well.
“As big chain retailers like Best Buy are closing up, health care providers are renovating these spaces as outpatient specialty clinics,” Quirk says. “It’s really a smart branding opportunity for health care.”
Patient flow in the outpatient setting is another area of focus to maximize efficiencies for staff and to move patients in and out as quickly as possible. With that in mind, emerging trends over the next five years appear to be expanded technology to support registration pre-visits (52 percent); boutique space for integrative medicine so patients can see multiple providers during a single visit (24 percent); concierge integrated health (34 percent); and flexible, multipurpose post-acute buildings that can accommodate a broad spectrum of patients (37 percent).
“Whether the care is interventional or diagnostic, it is important that the design flow reflect the points of care,” says Joseph G. Sprague, FAIA, FACHA, FHFI, principal and senior vice president at HKS Inc. in Dallas.
Yet to catch on appears to be self-rooming — where patients guide themselves to exam rooms without assistance — with just 14 percent of respondents having said this is on the drawing board over the next five years. Telemedicine booths in primary and specialty care are not yet a major trend, with 29 percent of respondents having reported that this is on the drawing board.