 Visibility is a fundamental expectation in the design of any environment where caregivers must work as a team with groups of patients — in both inpatient units and ambulatory units such as infusion centers, prep and recovery areas and, particularly, emergency departments (EDs).
Visibility is a fundamental expectation in the design of any environment where caregivers must work as a team with groups of patients — in both inpatient units and ambulatory units such as infusion centers, prep and recovery areas and, particularly, emergency departments (EDs).
It has spawned countless explorations of physical configuration that can drive staffing and operational processes over the life of a facility. However, staffing patterns and logistical support concepts are certain to evolve throughout that life, potentially as often as clinical leadership changes in the C-suite.
This evolution usually is based on efforts to improve quality of care, maximize utilization of human resources or lower operational costs. However, more often than not, these changes have nothing to do with improving visibility once an environment is built.
An array of priorities
Research has shown the essence of visibility consists of an array of strong priorities that the physical environment must address. In the inpatient holding environment, awareness of patients — their condition, their presence, their actions and their needs — is fundamental. Architects go to great lengths to create the perfect patient room to address these goals. Other patient holding areas, such as infusion, procedure prep and recovery, or emergency care, seek similar visibility capacity.
The design components that impact visibility within a unit include the configuration of a patient room or space; the collective arrangement of rooms or spaces to create a functional area housing a team of co-workers, including the physical environment housing documentation and management of care as well as supply, waste and equipment; and staff support spaces. The size of the operational unit matters considerably in the equation for maximizing visibility.
In a 2006 study funded by the American Institute of Architects, research was conducted by the Center for Advanced Design Research & Evaluation (CADRE), a knowledge initiative of HKS Inc. that can be accessed at www.cadreresearch.org, to examine what contributes to flexibility in inpatient bed unit design. Visibility was identified as one key component. In the CADRE study, called "Inpatient unit design: Defining the design characteristics of a successful adaptable unit," the definition of visibility expanded beyond the classic idea of viewing a patient or all patients from one physical point. Researchers discovered that the perception of visibility by workers includes the ability for auditory monitoring of patient rooms or spaces.
Beyond direct observation of the patient at the bedside, visibility means many things of fairly equal importance to caregivers. Awareness of the patient's presence or circumstance by simple observation from the corridor is fundamental. This means good sight lines to the patient bed are necessary. The ability to evaluate the condition of the patient at a distance, as in from the corridor, also is important. This necessitates visibility of the patient's head and face to sense condition or need.
Awareness of the patient's activity is gained through both visual and auditory input. Observation of activity in a room is valued most because it may alert the caregiver to provide assistance to a patient with fall potential. Auditory "visibility," which means hearing activity in the patient room, is important to caregivers as well.
The ability to provide this kind of awareness to caregivers depends on their proximity to the patient room. Additionally, electronic voice communication has supported auditory visibility for years. Today, this awareness is enhanced through the use of beds or ultrasonic monitoring devices that generate a notice if a significant weight change or unusual movement is detected.
Finally, a repeated discovery in multiple research studies is the inclusion of sight lines to peer caregivers. This consideration relates to the security, safety and overall awareness of the caregiver team in conducting its daily work. The quality of peer line of sight also influences the perception of caregivers in the overall flexibility of a unit to handle changes.
What influences visibility?
The ability of caregivers to monitor patients uninterruptedly as they go about their regular tasks is a vital consideration in care delivery relative to safety, efficiency and flexibility of the care environment.
In a recent study involving 20 U.S. hospitals, a team of researchers from Stanford University Center for Health Policy and Harvard Business School focused on operational and physical design factors that affect patient safety in health care settings. "Facility failure" was determined to be the foremost factor affecting patient safety and one of the facility failures was identified as difficulty in observing patients. In a parallel study at six major U.S. hospitals, findings suggested that poor visibility of patients is a key factor that affects operational flexibility and efficiency, according to the CADRE study.
In general, there are six key areas of design that influence visibility:
1. Patient room configuration. Room configuration plays a crucial role in promoting or impeding visibility. From a clinical perspective, a key consideration is whether a patient's head is visible through the doorway or vision panel when a caregiver is in the corridor. Design decisions regarding the toilet location, bed orientation, storage compartment location and transparency of the corridor wall all factor into this functional need. Many recent patient room designs, often aimed at accommodating varying levels of patient acuity, have placed the toilet and shower room in an outboard location to maximize patient visibility for staff and vice versa.
However, in one recent study of a bed unit having a combination of inboard and outboard toilet and shower configurations for the same patient population and care-giving team, the staff considered the inboard rooms to have better visibility. Further examination revealed that these rooms were, in fact, the rooms physically closest to the nurses' station. Researchers concluded that the shortest walking distance, concurrent with better auditory visibility from the nurses' station, was of higher priority than actual sightline when ranking visibility, based on the CADRE study, "A multidimensional framework for assessing patient room configurations."
Also important is that health care organizations are not all on the same page regarding the relative importance of patient visibility and patient views of outdoors. Some systems have established patient room standards that angle the bed for optimal view outside and the nurse's ability to see the patient's head and face are diminished. Given the increasing acuity of patients, this design condition and the importance of certain kinds of visibility are worthy of debate.
2. Documentation station location. The locations of the work areas where a caregiver can document records clearly has an impact on actual visibility, but often creates barriers to what clients define or perceive as visibility.
While enforcing work at the bedside by placing computers and scanning within the room assures direct line of sight, visibility often has been compromised because of the loss of visual contact with peers and lack of awareness of corridor activity. When giving the caregiver choices between room or corridor location for documentation, the latter appears to deliver a greater sense of visibility.
On units where documentation sites are only provided just outside or within the room, without some form of gathering point in the core, visibility again is cited as being compromised. Visual contact with peers, coupled with the ability to periodically gather or huddle, is a psychological need that influences what caregivers consider good visibility.
3. Core transparency. Designers often deceive themselves into creating physical arrangements or groupings of patient rooms based firmly on the staffing ratio described in the model of care for a project. Theoretically, this would enhance overall visibility, but the reality is that unit managers routinely balance the acuity load of each nurse, and his or her assigned patients are rarely aligned side by side. They must regularly cross the core of the unit to manage patients on more than one side. Hence, good visibility must include the ability to see through the unit, from one side to another.
Even when supply, medication and linen holding areas are successfully decentralized into the patient room, there are selected support spaces that impose opaque room volumes on the core. Efforts to remove these from the core to the perimeter inevitably increase daily walking distances to levels that are unacceptable — compromising patient safety and direct care time, and stressing and fatiguing the caregiver. Efforts to provide transparency in these spaces by placing storage below counter height results in excessive bending and lifting by caregivers. Neither are good solutions to the need for cross-unit observation.
Beyond the inpatient bed unit, there is an even greater concern for cross-unit visibility in the ED. A study, "Environmental correlates of safety and efficiency in the emergency department," under way by CADRE has suggested that operational efficiency as well as patient and staff safety and security are associated with good visibility — first in the public waiting and intake areas in the front of the house, and then broad visibility between patient treatment areas and team work centers.
4. Unit configuration. Both unit size and shape are key visibility factors. Repeatedly through post-occupancy evaluations, a perceived lack of visibility has been discovered in bed unit configurations where the core has been eliminated in favor of corridors double-loaded with patient rooms (often end or corner conditions). These rooms are often the last to be assigned on units because their convenient surveillance is limited by not being on the "beaten path" of continuous circulation for nurses.
Strong pod or cluster arrangements of patient rooms can severely inhibit visibility if not carefully tested and analyzed. These configurations should be mocked-up full-scale, simulated and challenged with such tools as failure mode and effects analysis or other simulations to assure that the arrangement facilitates good visibility throughout the unit.
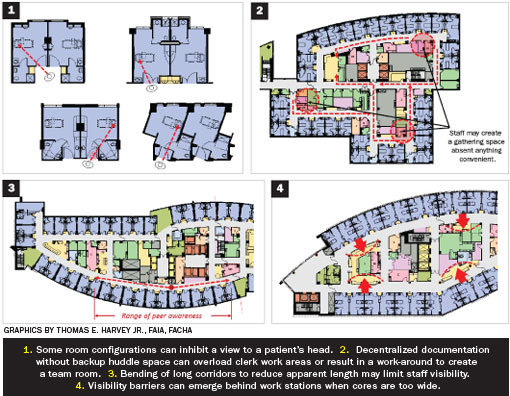
5. Corridor length. Large units with long corridors can impose visibility barriers. Real barriers occur when designers offset or curve corridors to reduce the perception of their length. On multiple units with curvilinear or other altered geometry to shorten the perception of the corridor, caregivers often note that visibility is problematic because they cannot see their peers. In the same study, perceived barriers were discovered when caregivers noted that cross-corridor smoke doors, a stairwell enclosure or similar break in the continuity of patient rooms occurs in the unit plan. While actual visibility may not be diminished, it creates a psychological barrier to some caregivers about their ability to observe territory created by their patients' locations.
6. Work station barriers. A final area of consideration is the emergence of continuous documentation stations around the interior, core side of patient corridors instead of directly outside one or two patient rooms.
This idea is of growing interest and addresses several visibility and other concerns, including better proximity of peers to each other while still being relatively close to patients as they document; greater visibility and expansiveness in the corridor as a result of its being perceived to be wider; potential reduction in noise levels outside the patient rooms; and an optional opportunity to decentralize supplies to fewer locations than in every patient room.
These configurations often are backed directly by unit support space in the core. This introduces visibility barriers because of the opacity of these rooms driven by building codes. Further, the configurations of the documentation stations face the caregiver outward, not positioned to look across the unit to both sides. This mistakenly presumes the caregiver will generally work on one side of the unit.
Perception and reality
Often, with a new design project, senior leadership of the institution will have a strong vision for change and can exert the management influence on the culture necessary to implement new ideas. These leaders rely on health care architects who have experience dealing with change observed over multiple generations of management within a facility. Hence, the seasoned health care architect is important to the design equation by intuitively addressing the perception elements that may ebb and flow as leadership shifts priorities.
Perceptions trump reality in human nature. One simple example is total decentralization of caregiver documentation stations such that all central work areas are eliminated.
Repeatedly on projects where this strong concept is the basis of design, the need for peer contact and visibility drives staff to create the essence of a central station within the core space. The impact deprives the planned operations of the unit of a space intended for other support.
CADRE research has shown that two other visibility considerations are important to design. From the patient's perspective, visibility of the corridor and of activity within it is associated with a sense of safety, security and satisfaction. Additionally, a staff's sense of security and safety is enhanced by visibility of family gathering areas in departments where unscheduled, episodic activities occur.
The core goal
Building a platform that positively influences the perception of good visibility in addition to delivering actual visibility must be the core goal in designing health care facility components where visibility is deemed critical.
Thomas E. Harvey Jr., FAIA, FACHA, is a partner and senior vice president of HKS Inc., and serves as president of the firm's CADRE initiative. He can be reached at tharvey@hksinc.com. Debajyoti Pati, FIIA, IDEC, LEED AP, is the Rockwell Endowment Professor at Texas Tech University and serves as the executive director of the CADRE initiative. He can be reached at dpati@hksinc.com.
| Sidebar - The importance of visibility |
|
Recent research studies by the Center for Advanced Design Research & Evaluation (www.cadreresearch.org) have discovered visibility to be a significant factor in patient safety, operational efficiency, patient and staff comfort and satisfaction. Two visibility attributes that affect functional flexibility or adaptability of hospital spaces described in the accompanying article include: 1. Peer lines of sight. Direct visibility of peers enhances the perception of operational flexibility and efficiency and provides a sense of security for caregivers. Obstructed sight lines increase stress by reducing the perceived and actual availability of help and opportunities for mentoring and socialization. The contemporary practice in health care design is to shift the principal work zones of the caregiver closer to the patient by providing documentation areas and supply storage closer to patient rooms. This is essential for minimizing travel distances and increasing direct care time available to patients. However, design of these work areas is critical to the nurses' sense of flexibility. Embedding these work areas too deeply out of the line of sight, down corridors or in areas comprising blind corners off the racetrack, suggests a lack of support team availability to caregivers. Interestingly, feedback from caregivers also concluded that gently curved corridors — designed to give an elegant exterior form and minimize the perception of corridor length on the interior — impedes peer visibility throughout the unit. Solutions:
2. Patient lines of sight. Higher acuity in medical-surgical units and an aging patient population necessitate better sensory links to patient rooms. This is a factor with considerable impact on operational flexibility. Nursing assignments frequently involve noncontiguous patient rooms where sensory links could be obstructed. Thus, the more open the unit, the more flexible the unit. Given increasing patient acuity and the fact that nurses often have patients in multiple locations on a floor, direct visibility of the patient through the doorway from the corridor and from the documentation station outside the room are minimal requirements. Other efforts to yield more openness throughout the unit can include views to patient rooms from the charting stations, medication stations and utility room doorways. Solutions:
|
| Sidebar - Researching issues of health care visibility |
|
For more than two decades, the design community has sought to establish a stronger foundation for design decisions based upon evidence of the value a design concept or element has to our clients. Architectural research interest has expanded beyond how architecture affects the people who use it, to a focus on performance – how it influences workflow and processes, safety and security, cost of operations and the well being of the occupants. A challenge that emerges as independent research teams endeavor to evaluate performance is an inconsistency in the definition of terminology used within health care and, consequently, a lack of uniformity of understanding of what this terminology really encompasses. One of the most important discoveries in learning how to set up a rigorous research framework and protocol is to confirm that the definition and view we designers hold about the topic we are studying correlates with the definition and view held by the users of the facilities we design. Do we speak the same language as our client? A prime example of this issue is the study of visibility. Visibility has been identified as a key contributor to patient safety, operational efficiency, psychological support of staff (awareness of peers), patient and family satisfaction, and user security. |
| Sidebar - The influence of unit size on visibility |
|
In an ideal world, a nurse could turn around 360 degrees in one location and see all his or her assigned patients. That was true in the Nightingale ward layout and is still prevalent in many countries around the world. In the United States, single-patient rooms have become the industry norm. Additionally, the single-patient room has grown dramatically in size to accommodate family and modern technology safety. It is no longer possible to provide immediate visibility of all assigned patients from one physical location, even in intensive care units of eight or more beds. Larger footprints of contemporary bed units compound these challenges. With these factors, a unit the size of Nightingale's is no longer realistic with respect to either visibility or walking distances. The industry's adjustment to this evolution of room size has been to adapt the definition of visibility. Alternative, objective interpretations of visibility, specifically in acute care settings now range from being able to see the patient's head from the room door, to being able to see any view of the patient from the room door, to being able to see the room doors of assigned patients from the nurses' principal work zones. The term "visibility" becomes more complex with the need of for an audibility dimension. The ability to hear alarms and calls for help from the patient rooms is a growing expectation due to higher acuity and frailty of patients admitted today. Add to that the feedback from nurses that good visibility includes having their peers in sight and the problem becomes quite challenging. Given today's patient room size, the creation of smaller working "units" of patients is worthy of discussion, even in light of some arguments that support staff may increase. To address safety, efficiency and satisfaction goals, moving toward a smaller unit size can more effectively address the visibility barriers that inevitable emerge in units comprised of 32 or more beds. Geographic distance between assigned patients can assuredly be reduced; back-up support areas typically in the core that block visibility can more likely be on the perimeter without excessive walking distances (assuming some supply areas are located in the patient room); and care teams can work in relative proximity and line of sight across the unit. Given the potential improvement in these ways, that issues associated with how to better staff these units without increasing work force is worthy of discussion. |
| Sidebar - Useful references on visibility in health care |
|
The following refences were used by the authors when writing this article. Carayon, P., A. Schoofs Hundt, B. -T. Karsh, A. P. Gurses, C. J. Alvarado, and M. Smith. (2006). "Work system design for patient safety: The Seips Model.'' Quality and Safety in Health Care. Center for Advanced Design Research & Evaluation, the knowledge initiative of HKS Inc., www.cadreresearch.org Harvey, T., Pati, D., Evans, J., & Vincent, D. "Environmental correlates of safety and efficiency in the Emergency Department." (2012). Final Project Report (under development) Center for Advanced Design Research and Evaluation (CADRE). Unpublished manuscript. Harvey, T., Pati, D., Evans, J., Waggener, L., & Cason, C. (2008). Inpatient unit design: Defining the design characteristics of a successful adaptable unit. AIA Report on University Research, Vol. 2, Washington, DC: American Institute of Architects. Pati, D., Harvey Jr, T. E., Reyers, E., Evans, J., Waggener, L., Serrano, M., & ...(check this ellipsis) Nagle, T. (2009). A multidimensional framework for assessing patient room configurations. Health Environments Research & Design Journal (HERD), 2(2), 88-111. Tucker, A., Singer. S., Hayes, J,. & Falwell, A, (forthcoming). Frontline staff perspectives on opportunities for improving the safety and efficiency of hospital work systems. Health Services Research. |





