
View "Master planning for the future" Gallery
The Affordable Care Act (ACA), a focus on population health management and the Medicare funding shortfall have created uncertainty for health care providers in deciding how to respond. Concurrently, the design profession has focused on improving the patient experience through the environment of care, improving efficiency and functionality through Lean planning, and reducing the cost of operations through more efficient buildings.
Traditionally, health care organizations have completed master plans in response to facility constraints and invested in new buildings to respond to growth or obsolescence. This planning has been largely facility-based and investments were made if the organization had the money. In more recent years, the analysis of return on investment has become more prevalent but still largely built on historic experience driving future expectations.
Also in this article |
| Master plan helps organization to improve and expand |
|
|
In the post-ACA environment, capital investment is a larger question far beyond simply expanding or replacing outdated or undersized facilities, improving the environment of care or even supporting evidence-based design. An organization’s board of directors, C-level executives and vice president of facilities and real estate must first align their strategy with their desired role within a health care community.
While most health care organizations have tried to be all things to all people, the future requires them to determine their role in the continuum of care. Positioning an organization to manage the health of a population, while continuing to work in a fee-for-service environment, requires thoughtful self-actualization before making 30-year investments.
New realities
In an attempt to create a sustainable health care delivery model and close the gap between cost and quality, Medicare has begun to reimburse hospitals based on value rather than volume. A value-based system requires that performance be improved by controlling costs and enhancing quality, safety and patient satisfaction.
The federal government is challenging health care organizations by putting their Medicare reimbursement at risk in multiple domains: clinical (the core measures); service (HCAHPS surveys); outcomes (mortality); and efficiency measures (cost per Medicare beneficiary). Depending on performance, health care organizations may receive what they would normally expect from Medicare; or they may get more or less.
You may also like |
| Conducting a facility portfolio analysis |
| Deciding to renovate or replace |
| 2014 Health Facility Design Survey |
|
|
Value-based purchasing, where cost, quality and service are each integral parts of the equation, is now widely seen as a replacement for the traditional fee-for-service model. For senior hospital and health system executives, the challenge is going from the way things have always been to the way things will be without tumbling into a fiscal chasm because of the way things are now.
Other elements besides reform also can be game-changers. Macroeconomics — the overall performance, behavior and structure of the whole economy — demands better planning. The aging of the population, new care models and tighter reimbursements are increasing the need proportionally for both critical care and ambulatory care.
Moreover, access to capital has, in many cases, not returned to its pre-2008 level. Expenses continue to increase as does uncompensated care. Technology continues to impact institutions at an intense pace. And there is significant competition for capital within an organization by other needs such as program development, medical staff recruitment, network development and information technology.
Ultimately, the bottom line is:
• The practice of tying facility decisions to the old models of reimbursement is outdated;
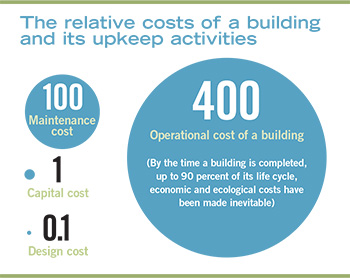
• The impact of operating costs far exceeds that of capital costs over the life of a building;
• Plans must be based on what and where services will be provided, not on an assumed historical straight-line growth of existing services.
So why would a health care organization continue to do facility master planning the same way it’s been done for decades?
Master planning approaches
In the traditional approach to master planning, a set of longstanding assumptions has been prevalent. For instance, it was assumed that most hospitals would provide all clinical services and that all of those services would continue to grow, albeit with some shift of volume to outpatient settings. It also was assumed that capital would be available to invest in buildings and that the best solution is always the best building.
Historic trends were used to determine future space needs while capital capacity dictated the size of the built solution. Operational performance was not prioritized. The people on the institution’s side in charge of delivering a master plan were typically facilities staff with only a modicum of oversight being provided by senior strategic leadership.
However, master planning in this new era should be based on the best strategic intent for the institution while keeping in mind a realistic capital envelope. The American Hospital Association Committee on Research’s 2014 publication, “Your hospital’s path to the second curve: Integration and transformation,” suggests the following strategic questions to help move an institution from volume-based to value-based care:
• What are the primary community health needs?
• What are the long-term financial and clinical goals for the organization?
• Would the organization be included in a narrow/preferred network by a health insurer, based on cost and quality outcomes?
• Is there a healthy physician-hospital organization (a business model that aligns physicians in private practice with hospitals and hospital-employed physicians)?
• How much financial risk is the organization willing or able to take?
• What sustainable factors differentiate the organization from current and future competitors?
• Are the organization’s data systems robust enough to provide actionable information for clinical decision-making?
• Does the organization have sufficient capital to test and implement new payment and care delivery models?
• Does the organization have strong capabilities to deliver team-based, integrated care?
• Is the organization proficient in program implementation and quality improvement?
Addressing these questions should occur before undertaking a facility master plan to give planning the correct direction.
Leadership buy-in
Clear guiding principles should be established at the outset of the project and bought into by the highest levels of leadership — the board and the C-suite. Throughout the entire planning process, there will be many instances of competition for resources; guiding principles help the team make decisions on resource allocation and prioritization.
A health care organization must know and understand its market. Being all things to all people is rarely accomplished in the present market; the organization should focus on defining community needs and the organization’s role in serving those needs.
Organizations should consider whether the market can be better served by shifting the delivery of services closer to the patients and at lower costs (e.g., outpatient facilities and physician offices), while at the same time balancing the necessity to have a critical mass for the utilization of such high-tech, expensive services as interventional radiology and radiation oncology.
They also should build for business and community need as opposed to facility potential. There may be a desire to overbuild for the immediate uses; but there should be a defendable reason, such as anticipated growth in a service line or to avoid a permanently missed opportunity due to a physical inability to build out a particular site at a later date.
The full range of the organization’s users should be considered. Traditionally, the focus has been on patients, employees and medical staff, but the focus also should be on patient families, who are much more involved in care than in the past. The larger community and how plans might serve the overall health of the marketplace and neighborhood also should be considered. Organizations should weigh opportunities in employment, education, retail, healthful lifestyles and access to healthful food choices, among others.
An institution’s relationship with physicians is a key driver in developing a master plan. Physicians will be accommodated in the planning process and master plan outcome in a different way, depending on whether the hospital is one in which physicians have admitting privileges or all of the physicians are employed or it is a physician-led institution.
When it is necessary to phase a plan, it should be based on a “most responsible moment” principle, rather than capital availability. In other words, it should be timed for when the facility is optimally needed, keeping in mind that physical constraints also may be drivers of phasing.
While the facilities manager may be key to organizing the master planning process and logistics, it is extremely important that the highest levels of the institution’s leadership are deeply engaged. This ensures that the plan is truly strategic and it addresses the multidimensional aspects of an organization’s mission, beyond simply a facility solution. The team should be diverse and multidisciplined, so that multiple points of view are raised, challenges are posed that create a stronger plan and all aspects of investigation are addressed.
Because capital planning decisions are among the most impactful a leadership team can make, there must be accountability. While each institution has its own process and protocols for decision-making regarding capital expenditures, it is sometimes surprising how many major moves are made with a large helping of gut feeling and a dearth of rational process.
Unfortunately, the outcomes of poor decision-making on major capital investments have to be lived with for a long time. It is important that an institution establish a set of metrics by which capital projects can be evaluated. In addition to answering the basic questions (e.g., cost of money and understanding the total project cost), the metrics should be designed to tie in with the move toward the provision of value-based health care.
Assuming a strategic plan has been established, other considerations include having a viable business plan for the project, measurable benefits that can be anticipated and operational improvements that can be incorporated.
Opportunities for operational improvements should be investigated in advance of facility planning because they will also impact the rest of the organization and must be manageable throughout the entire enterprise.
Physical considerations
Establishing an overall organizing framework with a time frame of future decades will set up an institution for flexibility to accommodate what cannot be predicted. What could be the next two, three or four moves after this one? Will it be possible to continue to add space to the hospital? Will it be possible to remove space that needs to be retired? Does the organization’s real estate strategy support future additions or subtractions? What physical plant considerations will help or hinder these moves?
Operational efficiency and flexibility must support any new organizing and operational models. Facilities don’t necessarily have to be organized by traditional departments. Multidisciplinary care methods and mapping patients’ movements through their care processes have led to developments such as the interventional platform and the acuity-adaptable room. An efficient master plan will show evidence of carefully thought-out flows with great thought toward hierarchy and separation of traffic. Soft spaces like offices can be located as easily movable occupants of strategically placed future expansion space.
Context is important. Every institution has something on the other side of the property line. Residential neighborhoods are particularly sensitive. Organizations should be considerate in addressing how the hospital’s master plan will affect neighbors.
While there is a tendency to think of facility master planning as resulting in buildings, open space is just as important. Open space can be reserved for future growth, but it’s also an important element of the overall plan. Research has shown that patients who have a view of nature will heal faster and require less pain medication than those who do not. Physical access for patients to outdoor space is being more frequently planned of late and hospital staff also use it for respite during breaks, finding it calming and refreshing.
There are some key drivers of form that are inextricably linked to an operational model, including the patient room. The organization’s model for nursing care also should be considered. Will nursing be centralized, decentralized or a hybrid of the two? Should the room shape and size allow for acuity adaptability (e.g., clearances within the room that will accommodate acute care patients now and intensive care unit patients in the future, if needed)? The patient room configuration will drive the column bay size for the patient floor. Site constraints for patient tower size and length should be reviewed at the same time.
A healing environment is essential for a positive patient experience. Desirable elements include access to daylight and views; maximum privacy and control for patients; allowance for family participation and accommodation; and even outdoor amenities. Consumer expectations are driving much of the demand for better-quality accommodations; but it’s also a bottom line issue when HCAHPS scores are considered. At the same time, planners must be aware of the risk of inappropriate supersizing of spaces like lobbies and waiting rooms.
Additionally, changes to technology must be anticipated and accommodated. While it is difficult to project what currently doesn’t exist but will be common in the future, it is possible to make buildings technology-enabled, whether for building systems or information technology, by building in flexibility for change and growth, especially in the “bones” of a new building (e.g., using optimal floor-to-floor heights and column bay sizes). It is also key to be cognizant that new types of treatment modalities emerge on a frequent basis and it is important to avoid overcustomization in planning. A physical plant should not constrain the mission of an institution.
Significant consideration also should be given to safety and security in the master plan. Site, infrastructure and building plans must consider the institution’s particular risks with respect to natural disasters, terrorism, surge capacity, redundancies and resilience.
Finally, approaches to sustainability should not wait to be identified until after the master plan is complete; the large moves should be integral to the plan. Organizations should target a low carbon footprint while looking at both renewable energy options and passive approaches.
A living document
A good master plan is a living document that guides daily decisions. It may sound ironic, but the less money an organization has, the more important it is to spend money on master planning. Organizations must plan deliberately with an appropriate balance of both free imagination and rational caution. The financial implications of building to a flawed plan are enormous.
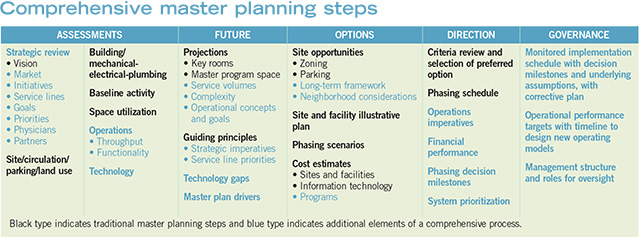
A comprehensive master plan is driven by senior leadership. However, it also is broadly participative, integrating all necessary disciplines into the process. Operational benchmarking informs capacity, financial modeling informs decisions, and business strategy drives projections and priorities.
Joan L. Suchomel, AIA, ACHA, EDAC, principal at Eckenhoff Saunders Architects in Chicago, is a founding member of the American College of Healthcare Architects and 2016 president of the American Institute of Architects Academy of Architecture for Health. She can be reached at jsuchomel@esadesign.com.





