As Health Facilities Management's readers rethink strategies and operations to help their organizations move more care off campus and into the community, they may be unaware that this transition is no recent phenomenon.
Ian Morrison, a Menlo Park, Calif.-based author, consultant and futurist, notes that the migration of the health care built environment has been under way for two or three decades.
"The single biggest factor has been medical technology," says Morrison, who is a regular contributor to Hospitals & Health Networks' H&HN Daily e-newsletter and a member of Health Forum's Speakers Express bureau. "Particularly the combination of less-invasive surgical procedures on the one hand and better drugs on the other, so you can treat patients in the outpatient setting who would have previously required significant lengths of stay."
Hand in hand with these advances have been financial incentives.
"Because of the significant concentration in the inpatient environment of diagnosis-related group-based funding where few hospitals can actually make money on Medicare, there's been more aggressive encouragement of the outpatient environment," Morrison says. "Certainly on the commercial payer's side, prices have been the key margin generator for most hospitals, so it's not volume as much as price on the outpatient side that has been really the core of financial sustainability for many institutions."
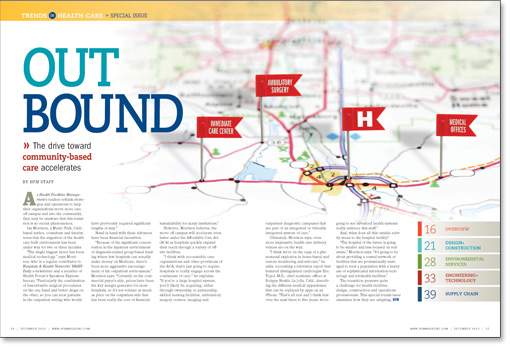
However, Morrison believes, the move off campus will accelerate even faster under the Affordable Care Act (ACA) as hospitals quickly expand their reach through a variety of off-site facilities.
"I think with accountable care organizations and other provisions of the ACA, that's just going to require hospitals to really engage across the continuum of care," he explains. "If you're a large hospital system, you'll likely be acquiring, either through ownership or partnership, skilled nursing facilities, ambulatory surgery centers, imaging and outpatient diagnostic campuses that are part of an integrated or virtually integrated system of care."
Ultimately, Morrison says, even more impressive health care delivery venues are on the way.
"I think we're on the cusp of a phenomenal explosion in home-based and remote monitoring and self-care," he adds, recounting a television report that featured distinguished cardiologist Eric Topol, M.D., chief academic officer at Scripps Health, La Jolla, Calif., describing the different medical apparatuses that can be replaced by apps on an iPhone. "That's all real and I think that over the next three to five years, we're going to see advanced health systems really embrace this stuff."
And, what does all this outside activity mean to the hospital facility?
"The hospital of the future is going to be smaller and less focused on real estate," Morrison says. "It's going to be about providing a central network of facilities that are professionally managed to treat a population with a heavy use of sophisticated information technology and telehealth facilities."
The transition presents quite a challenge for health facilities design, construction and operations professionals. This special trends issue examines how they are adapting.





