Patient focus
 As the debate on health care reform continues, its impact on hospital facility design remains unclear.
As the debate on health care reform continues, its impact on hospital facility design remains unclear.
Some predict smaller hospitals with multiple satellite buildings and freestanding outpatient care facilities. Others foresee a different future, in which acute care hospitals continue to grow larger and become more complex.
But, whatever the vision, it is certain that there will be a continuing need for complex medical care that will be provided in hospitals and, like today, inpatient unit size and layout will continue to be an important driver.
Among the significant recent trends in inpatient unit design are support for the single-patient room, decentralized nurses' stations and supply distribution, awareness of the importance of healing environments and patient safety, family-centered care and evidence-based design.
Because it is impossible to know exactly where health care is heading, it may be more practical to focus on understanding and refining current design initiatives for the near future.
The patient room
The patient room is the cornerstone of the inpatient care unit. It seems safe to conclude that the single-patient room, with separate patient, staff and family zones, will continue to be the norm.
However, one important issue requiring careful consideration is how the family zone is affected by other elements of patient room design. For instance, the staff zone is growing in complexity and additional equipment needs are pushing the patient bed into the family zone.
To allow more flexibility for equipment and bed placement in the future, headwalls must remain clean and flexible, with as few fixed elements as possible. Thus, as the patient room becomes more equipment- and supply-intensive, increased vigilance may be required to protect the patient and family zones, ensuring that they remain comfortable and retain healing amenities for the patient and family members.
Other considerations include the following:
 |
| The caregiver zone in this patient room includes a bedside work area with a mobile computer, sink and a nurse server cabinet that provides a pass-through to the corridor. |
Room standardization. Nowhere is the debate about implementing patient safety interventions more apparent than in the design of the inpatient care unit. Two types of patient rooms—cuity adaptable and standardized or same-handed—are currently being utilized to address patient safety issues.
Acuity-adaptable rooms, equipped to deliver care in one room to patients with varying levels of acuity, have been introduced as a way to improve care processes and patient safety. This model of care suggests that some types of patients, such as cardiovascular patients, can be admitted to the patient room directly from the intensive care unit (ICU) and stay in the same room until they are discharged, reducing transfers to other rooms or even other units.
What is frequently overlooked is the effect of the acuity-adaptable room on the larger inpatient unit. Future inpatient unit designs must take the whole unit into account. How will acuity-adaptable rooms affect the staff-to-beds ratio? The proportion of acuity adaptable rooms impacts the layout of the whole unit and the entire system needs to work together.
The second patient room concept thought to affect patient safety is the standardized or same-handed room. It is important to differentiate standardized placement of equipment from direction of approach (same-handedness). A patient room can be standardized but may not necessarily be same-handed.
The concept of using standardization as a means to reduce medical errors and increase patient safety originated in research and practice in other industries. This approach assumes that there are two types of errors present in complex systems, including health care: latent conditions (e.g., facility characteristics, equipment or processes that contribute to errors) and active failures (e.g., errors made by health care providers).
From this perspective, repetitive actions performed in standardized patient rooms are thought to reduce cognitive burden on staff and, consequently, reduce errors (from both latent conditions and active failures) especially in life-threatening or emergency situations.
The underlying premise is that staff intuitively know where equipment and supplies are located in every room. As a result, they are more able to focus on care and less likely to make errors. Unfortunately, research evidence to support this assumption is currently scarce. Likewise, the same-handed patient room concept is hindered by a lack of information on how nurses actually move while delivering care.
 |
| Left: Advances in technology have enabled nurses to move away from traditional centralized paper-charting station to smaller, decentralized workstations and charting substations distributed around the unit and closer to the point of care. Right: Each patient room in this 128-bed inpatient unit has a ceiling-mounted lift system that extends from the bed to the toilet to help move and turn patients and alleviate the risk of injury to patients and staff. |
Patient fall prevention. Nearly one-third of patients who fall suffer moderate-to-severe injuries that reduce mobility and independence, increase length of hospital stay and, subsequently, increase the risk of premature death. Inpatient falls frequently occur during unassisted transfers to and from bed and during toileting.
Changes in patient room layout, in which the distance from the bed to the bathroom is minimized and handrails are provided along the wall for patient support, have been suggested as possible ways to reduce falls. While these recommendations seem reasonable, no systematic research has been conducted to determine if these changes reduce falls.
A better understanding of the interaction between person factors (e.g., age, medications and cognitive state) and environmental factors (e.g., handrails, toilet room placement and flooring) will be necessary to reduce patient falls in the future.
The nurses' station
In the past, inpatient units were designed with one centralized nurses' station, necessitating numerous trips between patient rooms, the unit core and the nurses' station to chart, locate and gather supplies, and consult with other staff members.
Advances in information technology have enabled nurses to move away from traditional centralized paper-charting stations to smaller decentralized workstations and charting substations distributed around the unit, closer to the point of care.
Decentralized charting can improve patient visibility and increase family-staff contact while reducing time spent walking; on the downside, it interferes with staff consultations, staff mentoring and social behavior.
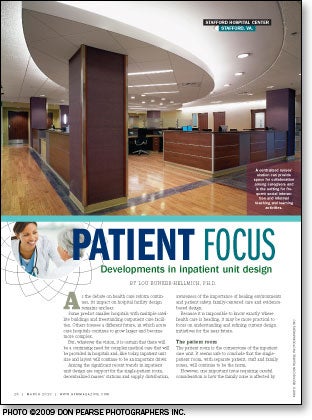
Health care is a multidisciplinary practice in which nurses, doctors, pharmacists and other support staff need a place to interact. A centralized nurses' station can provide space for collaboration among caregivers and is the setting for frequent social interaction and formal and informal teaching and learning activities.
Research suggests some of these important social functions may be negatively affected in decentralized nurses' station designs.
In a pilot observational study of three centralized and three decentralized nursing units conducted by Ellerbe Becket and furnishings company Knoll Inc. (www.knoll.com), East Greenville, Pa., significantly less time was spent consulting with other medical staff on each of the decentralized units when compared with the centralized units. In addition, observed social interactions were significantly higher in the centralized units than in decentralized units.
These results suggest that there are important social behavior components of nurses' station design that should be considered in the future. While the design of the nurses' station is no longer chart-driven due to the prevalence of technology, the nursing unit still needs a center of gravity where caregivers can find each other.
Other considerations include the following:
Access to supplies. Efforts to locate supplies and medications closer to patients also have led to a good deal of controversy. For instance, one hospital recently called in a number of consultants to determine the best system for their new facility. Each of the consultants recommended different, conflicting systems in line with their particular perspective, such as nursing or materials management.
The project's planners subsequently helped the client sort through the consultants' reports and create one plan that made sense for the hospital as a whole. Ultimately, they decided on three 10- to 12-bed clusters, each with a nurses' station, clean supply and medication rooms, and a pneumatic tube (i.e., three sets of everything on a 36-bed floor).
To address the supply distribution conflict, the client identified the top 50 most frequently used items and stocked those in decentralized supply areas. The rest of the supplies were stored in a central location.
The decentralization of supplies and medications has led to renewed interest in the use of nurse servers. Originally developed in the 1960s, nurse servers are supply closets built into the corridor wall of patient rooms, accessed from inside the room and stocked in the corridor. Questions about what to store in the in-room supply areas, who will have access, how they will be secured and how they are restocked will need to be addressed in future inpatient designs.
Noise reduction. Nurses' stations are often noisy, crowded, busy spaces. Sound sources include alarms, pagers, telephones and other technical equipment as well as frequent conversations. Noise on an inpatient unit interferes with communication between staff, increases stress among patients and staff, and disrupts patient sleep. According to patient satisfaction surveys by Press Ganey, South Bend, Ind., noise and poor acoustics are the most frequent complaints among both patients and staff.
It would make sense to assume that smaller, decentralized nurses' stations would be quieter than busy centralized nurses' stations. However, sound levels measured in all nurses' stations in the Ellerbe Becket and Knoll study exceeded recommended levels set by the World Health Organization and the Occupational Safety and Health Administration and did not differ significantly between centralized and decentralized nurses' station designs.
More research needed
As health care reform continues to evolve, it will be necessary to move forward in the near future with new inpatient design initiatives. Understanding the importance of looking at the pieces of the inpatient unit puzzle together, as a whole, integrated system, rather than as individual parts in isolation, will help guide and improve future designs.
Evidence-based design research has the potential to improve inpatient units of the future as well as other areas of facility design. Moreover, a comprehensive body of research results will be built over time, providing answers that can support or refute many intuitive assumptions.
The industry needs persistent, thorough, well-conceived design research to grow the field and meet the challenges of an uncertain health care future.
Lou Bunker-Hellmich, Ph.D., is health care research specialist at Ellerbe Becket, which became part of AECOM in late 2009. She can be reached via e-mail at Lou.BunkerHellmich@aecom.com. She was assisted with this article by Ellerbe Becket's Cindy Saathoff, senior interior designer; David Derr, AIA, principal; Roland Binker, AIA, senior medical planner; and Terri Zborowsky, R.N., Ph.D., director of health care education and research.




