Positive performance
 As the price of energy escalates and patient care requires more and more of it, health facilities professionals are searching for opportunities to reduce their expenditure. Typically representing the lion's share of this expenditure is a hospital's mechanical systems.
As the price of energy escalates and patient care requires more and more of it, health facilities professionals are searching for opportunities to reduce their expenditure. Typically representing the lion's share of this expenditure is a hospital's mechanical systems.
While it can carry a heavy price tag, the business case for upgrading a hospital's mechanical infrastructure is clear, providing both significant short- and long-term paybacks.
Following the five P's
The key to upgrading a hospital's mechanical system can be described in five words beginning with P: prior, planning, prevents, poor, performance.
Thus, assessment of prior infrastructure will dictate the type of mechanical system expansion possible. Changes in the local building code and new medical technology as well as the hospital's configuration and available land will play a role in this assessment.
Future hospital upgrades may require a more robust infrastructure that may or may not be in place. Detailed planning can provide the best life-cycle cost solution to ensure that the hospital's infrastructure keeps pace with the facility's mission.
Mechanical systems testing and validation can prevent any unwanted results through calibrated modeling used to predict future performance, real-time measurements and verification. Additionally, poor systems operation can be identified with corrective action, as the new efficiencies and the old deficiencies blend together.
Many times, poor operational performance is a gradual process that is the result of many factors. Optimal performance means reviewing new and old systems that were impacted by the upgrade to confirm improvement across the total facility.
But beyond these simple rules, a thorough mechanical systems upgrade takes place in two distinct phases, beginning with a systems assessment and plan, and concluding with validation and testing.
Assessment and plan
Gathering the project team to collect and review master plans and determine the goals of the new infrastructure usually is the first step in a hospital's mechanical systems assessment.
Interviewing operations and maintenance (O&M) personnel can reveal any existing infrastructure problems, including system deficiencies. Meeting with doctors and nurses who work in the space will provide insight into the comfort, workflow and noise issues experienced in the existing space on a daily basis as well.
This often-overlooked step is crucial to the assessment process because it eliminates the potential duplication of age-old problems repeating in the new facility and establishes both the O&M and professional staff as stakeholders in the upgrade, a distinction that will only enhance the performance of the new infrastructure.
Next, each of the hospital's existing systems should be reviewed, analyzed and scored to address reliability, energy efficiency, redundancy, code deficiencies and maintainability.
Is the mechanical system capable of meeting the current requirements of the space? Is it performing as expected or are occupants hot in the summer and cold in the winter? Is it capable of meeting the future infrastructure goals discovered in the interviews? Mechanical systems typically have a 30-year lifespan, so equipment condition is assessed as well.
Combining the interviews with field measurements, each system is given a grade. A report card is then distributed to hospital administrators to serve as a decision-making tool for prioritizing the mechanical upgrades.
With a better idea of which systems contain real deficiencies, an improvement plan then can be developed. This plan will determine the viability of each improvement, making sure the upgrades are actually possible given the uptime demands of each system.
In a working hospital, systems cannot be simply shut down and rebuilt. Instead, the improvement plan must detail the temporary systems or room changes that will be required to follow through with the upgrades.
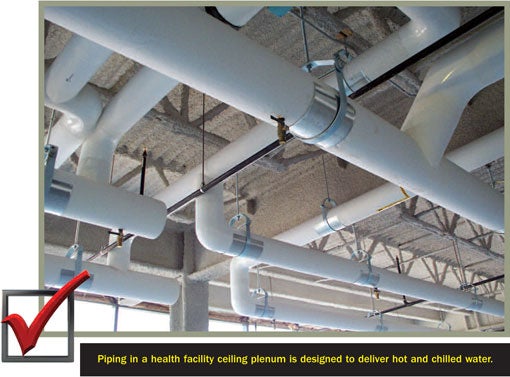
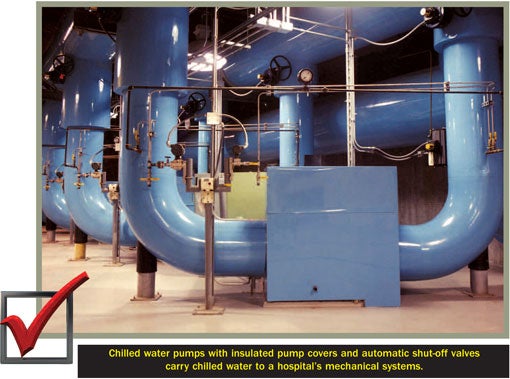
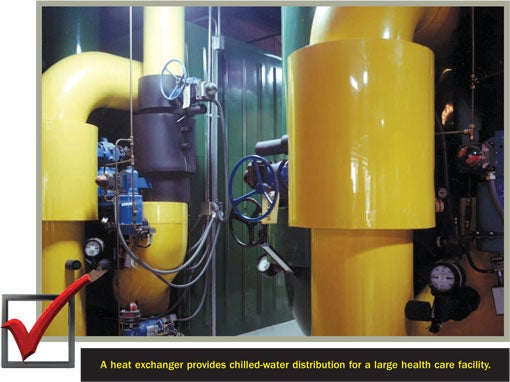
Customizable to each hospital, there are multiple solutions to this challenge. The most popular of these is a phased systems shutdown, which allows a hospital to remain fully functional throughout renovation and without any interruption of service. Factors that must be considered include duration, shutdown, disruption of operation, temporary systems operation, staging equipment locations and budget. Systems to be assessed include steam, hot water heating, cooling, ventilation, domestic hot and cold water, and control systems.
For example, an existing hospital's steam system can be 50 years old, patched for years to prolong its life. While boiler replacement is inevitable, it may not be the right immediate choice. Other questions need exploration. What pressure level will be maintained? What fuels will be used to support the equipment? What are the Environmental Protection Agency (EPA) emissions regulations that will change with the new equipment?
Systems flexibility and sustainability are key considerations in the upgrade plan during this stage as well. Which mechanical infrastructure upgrades will improve the hospital's cash flow or operating costs? Can the system be designed for today's load and future demands in a modular manner with minimal disruption? Is there a minimal cost to prepare the hospital for the next infrastructure upgrade down the road? Does the health care organization favor a lower first cost or are the owners more concerned about ongoing long-term costs?
Documenting the systems assessment and improvement plan phase is also crucial. Creating a living document with a clear paper trail of system upgrade scores and choices will provide a path for future upgrades and documentation for management, including necessary upgrades beyond the current budget that are scheduled for future years. Documenting efforts of the improvement process also will ensure that the new system capacities and sizes will aid in making better assumptions in the future.
An excellent method for capturing this data is the comprehensive building information modeling (BIM) process. Integrating documentation and measurements from all building team members throughout design, the BIM model will track systems improvements across the facility.
"Before" and "after" benchmarks also should be analyzed. What are the standards by which the new system improvements will be measured? Analyzing current hospital expenditure and projecting future expenditure goals through building and energy modeling will create a benchmark for both a one-year post-occupancy and a multiyear improvement plan.
Finally, commissioning and continuous commissioning should take place. Commissioning will make sure the desired system outcome has been achieved. For example, the commissioning agent will verify that the replaced air handlers maintain the right temperature, humidity, pressure, flow rates and velocities. Continuous commissioning not only validates that the mechanical systems are working on day one, but also helps maintain the improvement level as time goes by.
Validation and testing
Mechanical systems validation and testing is an important final step to eliminate any surprise discoveries during construction and any future infrastructure improvement projects.
In this phase, the team should study the project's scope and boundary. Are there any project limitations, including budget or spaces that have changed? Studying the project scope and boundaries to solidify comprehensive design decisions will ensure their intent is being met by the specified mechanical design.
Project forecasts and requirements should be compared. Under validation and testing, the basic design plan devised in the assessment-and-planning phase will be revisited. With additional information gathered, the original assessment may not be the right solution. Maybe the technology, cost-effectiveness of the plan or the owner's space requirements have changed. The project team should go back and revalidate the plan for improvement, if needed.
Additionally, critical path systems should be identified. What is critical that has to be done early rather than later? This may include testing or purchasing the equipment. An additional consultant also may be needed for this step. For example, if the cooling towers are slated for roof installation, will the roof actually hold them? During the assessment, it was assumed that the structure would hold the new cooling tower. Is that realistic? This is the time to explore the actual math. Also at this point, the system can be modified and the project design concept solidified.
New systems can be validated by integrating the new mechanical system with the existing one and commissioning the pair. Depending on how much time the project team wants to spend, commissioning can simply report that the equipment is working or it can report that it works well, both tuning and optimizing it.
The success of any infrastructure upgrade is largely dependent on the maintenance personnel's understanding of the hospital's new systems. After installation, the equipment manufacturer's representative must train the O&M staff on its operations. Videotaping these sessions will ensure continuity after the current O&M staff is long gone.
The O&M staff usually is involved in collecting performance data as well. Does the post-occupancy performance data support the projections? Typically taken one year after move-in, performance data will ensure that the systems are functioning as designed. This may involve occupant and staff interviews, reviewing utility data and equipment logs as well as trending data from the building automation system (BAS).
Back to the five P's
Integrated throughout system assessment, planning, validation and testing, the five P's provide hospitals with a detailed plan for mechanical system improvement.
Assessment of prior infrastructure will dictate what new systems are needed and which existing ones will remain when planning the hospital upgrade at the lowest life-cycle cost. Mechanical systems testing prevents any unwanted results or poor systems operation, leading to optimum performance one year later and a process to maintain that performance throughout the life of the system.
With careful assessment and infrastructure planning, hospitals can reduce their energy expenditure and significantly impact their bottom line both today and tomorrow.
James Vallort, LEED AP, CBCP, CSDP, CEM, leads the Health, Institutional and Sciences Group at Environmental Systems Design (ESD), Chicago. He can be reached at jvallort@esdesign.com. Robert D. Benzuly, P.E., is vice president at ESD. He can be reached at rbenzuly@esdesign.com.
| Sidebar - Adding capacity to imaging suite |
| Chicago's Northwestern Memorial Hospital (NMH) was looking to upgrade its outpatient imaging department located on three floors in a neighboring commercial office building. After meeting with hospital administrators to understand both their immediate and long-term needs, a building assessment that included a review of the existing mechanical systems was performed in March 2007. The study revealed that the mechanical infrastructure lacked the capacity to serve the immediate requirements for the new ultrasound, X-ray, magnetic resonance imaging and computed tomography scan areas. Multiple infrastructure upgrade options were presented to NMH to help the existing mechanical systems meet the cooling, pressure requirements and stringent air quality needed for imaging areas, as well as to meet planned future growth. The new mechanical systems design, completed in spring 2008, included five new modular, water-cooled chillers and cooling towers providing cooling water for year-round use to meet current loads, future load growth and to provide N+1 redundancy. Working with the hospital owner to prepurchase the equipment that matched their cooling profile and energy requirements allowed this equipment to be optimized as a system. Additionally, the building's existing building automation system (BAS) was expanded to monitor and control the new high-performance equipment. New air handling units with BAS control were provided for the imaging suite. Training was provided to all three shifts of building operators and videotaped for future use as a refresher course and for staff training. The infrastructure improvements completed in early 2010 allowed the imaging department to function at its full capability with reliability and redundancy. |




