Automated disinfection systems
It has long been recommended that environmental surfaces in patient rooms be cleaned and disinfected on a regular basis, when surfaces are visibly soiled, and after patient discharge. Disinfection usually is performed using a hospital disinfectant registered with the Environmental Protection Agency (EPA).
“However, recent studies have shown that this type of cleaning can be inadequate,” contends Douglas Goldman, senior product manager, Steris Corp., Mentor, Ohio. “In addition, hospitals deal with unique surfaces that may present difficult cleaning challenges, as well as surfaces that should not be cleaned with some typical disinfectants.”
Automated disinfection systems have evolved to meet the specialized needs of hospitals. A variety of technologies — using ultraviolet (UV) light or hydrogen peroxide (HP) vapor — are available to complement traditional methods of cleaning. The goal is to disinfect patient rooms in a fast-paced environment and reduce the possibility of health care-associated infections (HAIs).
UV disinfection
Steris manufactures the Pathogon UV Disinfection System, which is designed to kill pathogens on environmental surfaces. After completion of a manual cleaning process, the system delivers a calculated dose of germicidal UV-C energy, which alters the DNA of aggressive pathogens to kill them. The process produces no ozone or secondary contaminants and rooms can be reoccupied immediately after treatment.
Safety features include sensors that, when detecting motion and heat, turn off the UV lights and stop the cycle. A wireless controller allows the operator to exit the room before initiating the countdown to start the disinfection cycle. A protective lamp cover doubles as a door barrier to be placed at the entrance and exit of the room.
The Clorox Healthcare Optimum-UV System produces UV-C energy via ultraviolet lamps that emit a wavelength of approximately 254 nm, the ideal wavelength to kill microorganisms by inactivating their DNA. The system achieves 99.992 percent reduction of Clostridium difficile spores in five minutes at 8 feet, and greater than 99.999 percent reduction of methicillin-resistant Staphylococcus aureus (MRSA) in two minutes at 8 feet.
Xenex Disinfection Services, San Antonio, manufactures devices that use pulsed xenon instead of mercury to create UV light. Pulsed xenon is powerful, so the units are capable of disinfecting rooms in minutes, according to Daniel English, senior advisor, environmental services (ES). Additionally, no warm-up or cool-down time is required between cycles, so the devices can treat many patient rooms each day.
Also, the devices are connected to an online database that enables ES managers to track which rooms have been treated and by whom, so they are able to verify that the rooms being targeted are the ones being treated. Xenex’s broad-spectrum UV light is capable of damaging microorganisms four different ways to ensure that the pathogens are destroyed.
“Eliminating pathogens from patient rooms is the quickest and easiest way to lower the risk of additional infections,” says Mark Stibich, Ph.D., chief scientific officer. “Our customers report in peer-reviewed, published studies that after using Xenex germ-zapping robots to disinfect surfaces, they experienced significant reductions in hospital-acquired infections.”
Automated disinfection systems that measure UV-C dose and adjust timing cycles to adapt to room variables have the majority of the current market share, according to Chuck Dunn, president and CEO of Tru-D SmartUVC LLC, Memphis, Tenn. However, the latest trend in hospital demand regarding UV disinfection devices is about more than delivering consistent outcomes alone; it’s about having the data to prove it.
“Hospitals are insisting on solid reporting data that integrate into software found in environmental services and bed-tracking software packages,” Dunn says. “Tru-D SmartUVC with built-in sensor technology not only is able to ensure consistent outcomes through measurable dose delivery, it also employs the device’s cloud-based, usage tracking capability to provide hospitals with the data they need for this integration.”
Among the latest advances in automated room disinfection is the use of multiple emitters during the same disinfection cycle, according to Gunner Lyslo, CEO, Surfacide, Naperville, Ill. “The issue of shadowing is well-known, and recent published data indicate that objects and surfaces in direct line of sight are more effectively disinfected by UV-disinfection than those in shadowed areas.” The Surfacide Helios system uses multiple emitters designed to overcome the shadowing problems hospitals face when using a single emitter.
The introduction of new automated disinfection systems has led to new business relationships between third-party companies and UV-C manufacturers. Last year, Clorox Healthcare, Pleasanton, Calif., entered into a partnership with UltraViolet Devices Inc. (UVDI), Valencia, Calif., to introduce the Clorox Healthcare Optimum-UV System. The partnership marked the first time both companies were able to offer health care customers a comprehensive, bundled approach that combines proven, EPA-registered surface disinfectants with UV-C technology to help facilities reduce the threat of infection among patients, staff and visitors.
“In this instance, a partnership was a great way to quickly pair our efforts to help protect patients and reduce illnesses caused by HAIs. It remains to be seen if this type of relationship will become an industry trend as the needs of the health care landscape continue to evolve,” says Rosie D. Lyles, M.D., MHA, MSc, head of clinical affairs for Clorox Healthcare.
“With the rising need for improved solutions in environmental surface disinfection, we are excited to partner with Clorox Healthcare and expand our reach in providing advanced UV solutions to the health care industry,” adds Peter Veloz, CEO and chairman of UVDI.
For close to a decade, Tru-D SmartUVC has been developing and maintaining relationships with cleaning and environmental services companies contracted by hospitals across the country, as well as with infection prevention experts and decision-makers within those facilities, according to Dunn. “With the recent increase in attention toward automated UV-C disinfection technology among group purchasing organizations, Tru-D has been selected as the sole source for this category among some of the nation’s largest integrated delivery networks.”
Elsewhere, Crothall Healthcare, Wayne, Pa., an environmental services company, has partnered with Surfacide to improve its operations, according to Lyslo.
HP vapor systems
Disinfectant fogging systems also are available to disinfect hospital rooms and prevent the spread of HAIs. Sanosil International, New Castle, Del., has developed the Halo Disinfection System, which eliminates 99.9999 percent of C. difficile spores in hospital rooms. It is the first EPA-validated aerosolized HP fogging system to disinfect entire rooms, says Maryalice Panarello, vice president of business development.
The system also kills others pathogens commonly found in hospitals by using a patented solution of HP and ionic silver applied in a dry mist by a portable fogger. During hands-free use, the odorless mist reaches in and around every surface in an enclosed area. There is no need for rinsing or wiping.
By using the Halo Disinfection System, Pennsylvania Hospital in Philadelphia reduced its C. difficile rate by 66 percent, from 4.9 to 1.65 new cases per 10,000 patient days, during the first year of implementation, Panarello says. As a result, the hospital was awarded Penn Health’s Quality and Patient Safety Award.
Bioquell Inc., Horsham, Pa., manufacturer of the Q-10 Suite Hydrogen Peroxide Vapor emitting system, has developed chemical indicators (CIs), which are placed inside the area being decontaminated and display the expected effectiveness of a Bioquell cycle.
Cards are impregnated with a dye that changes color in the presence of HP vapor. “Incoming patients should not be at risk of acquiring an infection because of a previous infected patient. These indicators help to prevent that from happening by letting hospital staff know that the proper amount of HP vapor has filled the room,” says Ed Striefsky, director of operations.
In other instances, where environmental services personnel need confirmation that a pathogen has been eliminated from the entire area, Bioquell uses biological indicators (BIs). They are designed for the HP vapor decontamination process and reportedly assure that 99.9999 percent of the bioburden is killed during every decontamination cycle.
“One example of the use of BIs is the recent spread of Ebola,” Striefsky adds. “Hospitals around the world have asked Bioquell to decontaminate areas occupied by Ebola-infected patients. During these situations, it is critical to use BIs to validate a kill of more than 99.9999 percent of pathogens. Unlike CIs, BIs must be incubated for a number of days before we can complete a full assessment.”
Making a selection
Hospital facilities managers need to consider many factors when purchasing and implementing an automated disinfection system. One factor is how they can make the purchase cost-effective.
“The easier a product is to use, the more likely it is that staff will use it correctly,” says Lyles. “Environmental services professionals should ask vendors about ease of use along with factors such as maintenance and training support to determine the best automated solution for their facility.”
What should always matter first and foremost are relevant studies and facts regarding the efficacy of the system, says Striefsky. “Without this data, environmental services managers could be wasting their time and money,” he adds.
“Never hesitate to bring in a subject matter expert, such as an infection control expert, for his or her opinion,” he continues. “When it comes to the latest features with automated disinfection systems, safety should be the primary focus. The system should be safe for the end user and for the incoming occupant. While some systems will focus on speed, be sure to ask if faster means more effective.”
Neal Lorenzi is a freelance health care writer based in Mundelein, Ill.
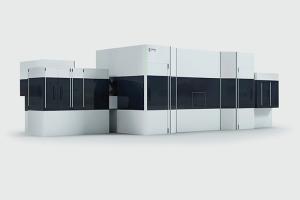
 | Extra exposureA standard Helios Triple-Emitter UV-C system room configuration is designed to overcome shadowing problems. |
 | Taking the pulseThis unit utilizes pulsed xenon UV light to destroy microorganisms that cause infections. |
 | Room is readyThe Halo Disinfection System is an EPA-validated aerosolized hydrogen peroxide fogging device that disinfects entire rooms. |
 | Data-drivenThis device uses combined automated measured dosing capabilities and real-time usage tracking to ensure optimum disinfection outcomes. |
 | Surface sanitationThe Q-10 Suite Hydrogen Peroxide Vapor system decontaminates any exposed surfaces in an enclosed room, floor to ceiling and wall to wall. |
 | Extra protectionThe Optimum-UV System combines effective manual surface treatment supplemented by UV-C technology to inactivate dangerous and persistent pathogens for optimum prevention. |
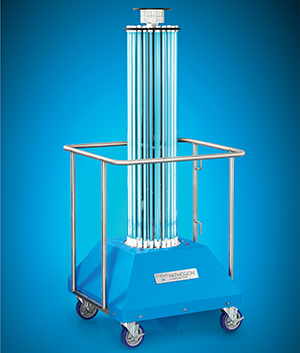 | Lethal doseThe Pathogon UV Disinfection System delivers a dose of germicidal UVC energy that alters the DNA of aggressive pathogens, killing them. |