Study says patients infected with Clostridium difficile are twice as likely to be readmitted
 |
| PHOTO BY JANICE HANEY CARR/CENTERS FOR DISEASE CONTROL AND PREVENTION |
All facilities across the health care spectrum need to maintain strict compliance with hand hygiene, use of protective wear and especially antibiotic stewardship requirements to reduce the number of Clostridium difficile-infected patients who are readmitted to the hospital.
Patients infected with C. difficile either upon admission to the hospital or during their stay are twice as likely to be readmitted within 30 days as those not infected with the bacterium, according to a study published in the April issue of the American Journal of Infection Control.
“We should be looking at our health care system as a whole, not just as one hospital, because the world is becoming smaller and smaller,” says Teena Chopra, M.D., an expert with the Detroit Medical Center’s (DMC's) division of infectious diseases and leader of the study.
“Patients are moving from one facility to another more frequently and transitions of care are very weak regarding sharing patient information,” she says.
Patients in acute care hospitals are transferring from nursing homes, skilled nursing facilities and long-term acute care facilities with possibly less stringent policies for hand hygiene, environmental services and use of antibiotics, Chopra says.
Researchers from DMC, a seven-hospital health care system, studied the epidemiology of C. difficile infection (CDI) readmissions by analyzing 51,353 all-cause hospital discharges in 2012.
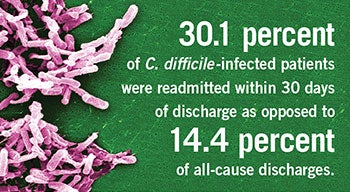
Of that number, 615 patients, or 1 percent, were discharged with a CDI diagnosis, including 318 who were infected with C. difficile upon admission and 297 who were diagnosed during their hospital stays. The study reported that 30.1 percent of C. difficile-infected patients were readmitted within 30 days as opposed to 14.4 percent of all-cause discharges.
The study also revealed that the length of stay upon readmission was higher among C. difficile-infected patients compared with non-CDI readmissions. Patients readmitted with community-onset CDI spent 4.4 more days in the hospital and those with hospital-onset CDI spent 6.4 more days in the hospital compared with non-CDI readmissions.
Chopra says controlling C. difficile bacteria presents difficult challenges because it produces highly resilient airborne spores that clinical staff may carry on their clothing even when they are not touching a patient, she explains. That’s why it’s important for staff to wear protective gloves and gowns and to practice vigorous hand hygiene using soap and water, she adds.
Because patients older than 65 who take antibiotics are most at risk for developing CDI, Chopra advocates the use of strong antibiotic stewardship programs in acute care hospitals as well as nursing homes and long-term acute care facilities, especially as the population ages.
More than half of all hospitalized patients will receive an antibiotic during their hospital stays, but studies have shown that 30 to 50 percent of antibiotics prescribed are unnecessary or incorrect, according to the Centers for Disease Control and Prevention.


