Minimum impact

Health care waste is a complicated and costly compliance challenge to health care organizations.
It can include everything from chemical hazardous waste, construction and demolition debris, infectious red bag waste, pathological waste, pharmaceutical waste, laboratory reagent waste, radioactive waste, recyclables, solid waste and wastewater.
Transportation and disposal of waste creates greenhouse gases, incineration leads to air pollutants that irritate the lungs and the heart, sewer disposal leads to contamination of drinking water sources and land filling can create methane, pollute groundwater and destroy habitats for humans and wildlife.
Health care waste streams also are regulated by a variety of entities, including the Department of Transportation, Environmental Protection Agency (EPA), local health departments, the Joint Commission, the Nuclear Regulatory Commission, state environmental agencies, state and local solid waste commissions and publicly owned wastewater treatment plants. These entities often impose a number of restrictions on the management and disposal of waste, including segregation, labeling, packaging, record-keeping, transportation, treatment and disposal.
Waste from provider organizations that is not properly managed can create pollution that is detrimental to community health and contrary to a health care organization's mission.
Impacts of waste
Recycling a cardboard box may involve as many as six touches or handoffs by different staff before it ultimately is sent for recycling. The staff involved in managing a waste cardboard box vary from materials management to pharmacy staff and surgery personnel, eventually to environmental services, and leads to costs considerably more than 3 cents per pound charged by a facility's waste management vendor.
Fig. 1 shows the economic impacts waste can have on a health care facility. In addition to extensive internal handling, transportation expenses — including fuel surcharges or stop charges — often are added onto waste management fees. Compliance costs include the time spent developing segregation and management programs, staff education, container expenses and logistics, record-keeping, environmental audits and improvements.
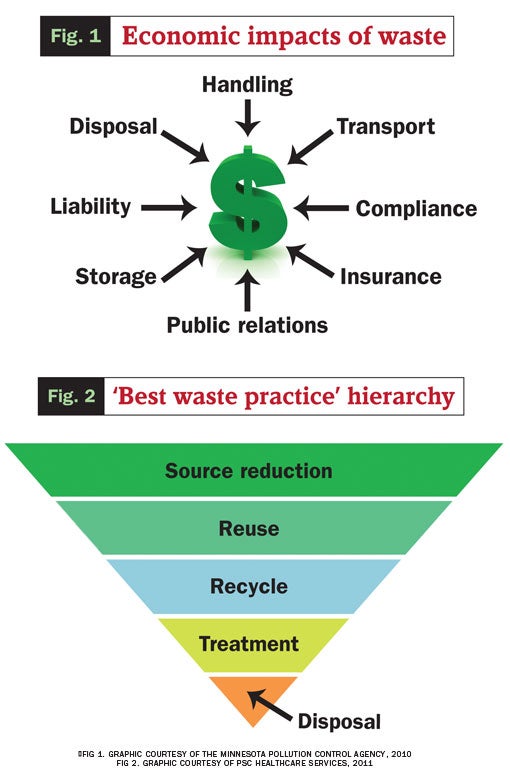
Hazardous materials spill cleanup also can be a significant expenditure and facilities that use and dispose of hazardous materials have higher insurance costs than others. Moreover, any health care provider that has experienced improperly disposed waste — such as infectious waste at a landfill — can understand the penalty associated with bad press. In addition to the liabilities associated with hazardous material spills and exposure of staff, patients and visitors, a business could be required to clean up a contaminated disposal site.
Finally, space is often at a premium in health care organizations, and using space for storage of waste rather than for the production of revenue, extracts a toll on the bottom line.
All of these impacts add to an organization's operational costs and often they are not fully realized. Acknowledging these costs can provide the incentive needed to engage in "best waste practice."
Best waste practice
Best waste practice calls for source reduction, reuse and recycling as the primary strategies for accomplishing the goals of reducing costs and minimizing environmental and public health impacts (see Fig. 2 above). Treatment and disposal are the least preferred, as they are waste management options that result in the aforementioned impacts.
Source reduction is key to curtailing waste and associated overhead. It contradicts the mindset that waste has to be a part of business. Source reduction also includes reducing the toxicity of waste. It involves looking at every item that creates waste and considering what can be done to eliminate it.
Employing reusable totes and containers as substitutes for cardboard boxes is an easy source-reduction activity. These items can be used repeatedly before they have to be repaired, remanufactured or recycled.
Inventory management that employs actual utilization data to determine appropriate stock levels also is a good tool for source reduction, especially for more costly wastes such as expired pharmaceuticals and lab reagents.
Source reduction is not the same as recycling. Recycling involves the creation of a waste (e.g., a cardboard box, which is used as feedstock in the manufacture of another product, such as another cardboard box). However, additional resources such as paper fiber, water and energy are needed to make the new box and additional waste is generated. Many wastes that are recycled, such as plastic water bottles, are not recycled into the same item but are down-cycled into less critical uses such as detergent bottles.
Minimizing the toxicity of waste is also a source-reduction strategy. Source reduction has been used to minimize the toxicity of many chemicals used in the past, such as trichloroethylene or polychlorinated biphenyls. These chemicals ultimately were recognized as being toxic and persistent. Source-reduction strategies have succeeded in reducing and eliminating their use. In environmental services operations, using a less-toxic disinfectant, such as substituting hydrogen peroxide, can improve safety for workers and minimize compliance and hazardous waste disposal costs.
Source reduction is easy. Denying waste entry can be made part of the procurement process. It can be included as part of the request-for-proposals process or as part of an environmentally preferable purchasing (EPP) program.
EPP often is used to select items with less environmental impact both in their manufacture and disposal. Purchasing office paper with greater than 30 percent postconsumer recycled content is often part of an EPP program.
Vendors can be asked how their product reduces waste, reduces toxicity or whether the product can be reused, reprocessed or remanufactured. Examples include eliminating the use of redundant or unnecessary products; using microfiber mops that require less chemical and water; and using equipment made with components that can be changed out as opposed to disposing the entire item. EPP products, strategies and tools are available from the EPA at www.epa.gov/epp, Practice Greenhealth at https://practicegreenhealth.org/topics/environmentally-preferable-purchasing/epp-case-studies-health-care or from various local environmental programs.
If source reduction is not an option, considering whether an item can be reused or remanufactured for reuse is the next step in reducing waste. Examples of reuse strategies that lead to reduced waste are refillable bottles used for cleaners rather than aerosols, equipment that can be reprocessed for reuse, and such solvents as alcohols, formalin and xylene that can be distilled.
Recycling is the third step in a source-reduction strategy. Because recycling uses a waste and remanufactures it into another item, it is not the most preferred option to reduce waste. Some wastes, like aluminum, cardboard, newspaper, office paper and steel, can be recycled back into cans, boxes, newsprint and office paper. Purchasing products that are recycled back into original items is the best source-reduction approach.
The last steps in a best waste practice program are treatment of the waste to minimize hazards, such as autoclaving infectious waste and incineration of hazardous waste, followed by final disposition in a monitored landfill.
Using all these steps is critical to a good waste management program. However, focusing on source reduction will provide the most economic, environmental and health benefits.
Tracking progress
Good waste management involves identifying, quantifying and tracking all waste streams in the health care facility.
Source reduction utilizes the data to pinpoint wastes to be reduced. Paper and cardboard, followed by plastics, are often a health care facility's largest waste streams. Pharmaceutical waste management is the most complicated.
Most health care facilities probably are engaged already in source reduction in some areas, such as utilizing reusable dishware in the cafeteria, distillation of xylene in the laboratory, or installing compact fluorescent light bulbs that conserve energy and reduce waste. Source reduction in almost any department will improve the environmental services team's productivity as reduced time spent handling waste will leave more time for other tasks, such as infection prevention.
It is important to track the information and data generated from these practices. Values to track include the name, composition and quantity of items, weight, procurement and disposal costs, and notes on how the results were achieved. Using the data generated from waste practice activities will show cost savings, can be used for productivity and labor measurements, and is a good environmental improvement initiative for the Joint Commission or other quality program.
Environmental benefits can be quantified using the EPA's waste reduction model (WARM) calculator, available at www.epa.gov/warm/versions-waste-reduction-model-warm#WARM Tool V14. The WARM calculator measures greenhouse gas reduction based on waste management practices such as source reduction and recycling. For example, source reducing 1 ton of office paper rather than incinerating it will eliminate 8 tons of greenhouse gas equivalents. The reduction in pollutants not only is due to the reduced paper, but also to the pollutants slashed by not manufacturing, transporting and disposing of the paper.
The WARM calculator shows that environmental outcomes of source reduction can be multiplicative. Best waste practice outcomes are also multiplicative. They can improve compliance, improve community health and improve the organization's bottom line.
Catherine Zimmer is an industry leader for PSC Healthcare Services, Houston. She can be reached at catherine.zimmer@pscnow.com.
Sidebar - Making cleaning operations environmentally friendly


