Building a design framework for better results
Every project presents an opportunity to tackle complex challenges. A range of problem-solving approaches is available to support designers, researchers, facilities professionals and implementation teams in achieving their goals.
Often, teams draw on multiple approaches — such as an evidence-based design (EBD) process, which uses credible research to guide design decisions, and Lean methodology, which focuses on maximizing value while minimizing waste.
Choosing the best approach isn’t an either/or question — the answer is using a combination of both.
Integrating EBD with Lean throughout the planning, design and construction phases can unlock a broad and distinctive spectrum of improvements — in health, safety, quality, user experience and business outcomes.
Foundation and framework
These complementary approaches form the foundation and framework for project success, benefiting all stakeholders involved.
What is EBD? EBD is the process of basing decisions about the physical environment on credible research to achieve the best possible outcomes. EBD focuses on business challenges and improving outcomes and aims to create environments that have a positive impact on patient health, safety and well-being as well as staff satisfaction and efficiency.
Research-informed design leverages evidence from various sources, including design research, industry benchmarks and best practices, to inform design choices and solutions. EBD considers the needs of different users, including patients, families, staff and visitors, to create spaces that are user-friendly and supportive.
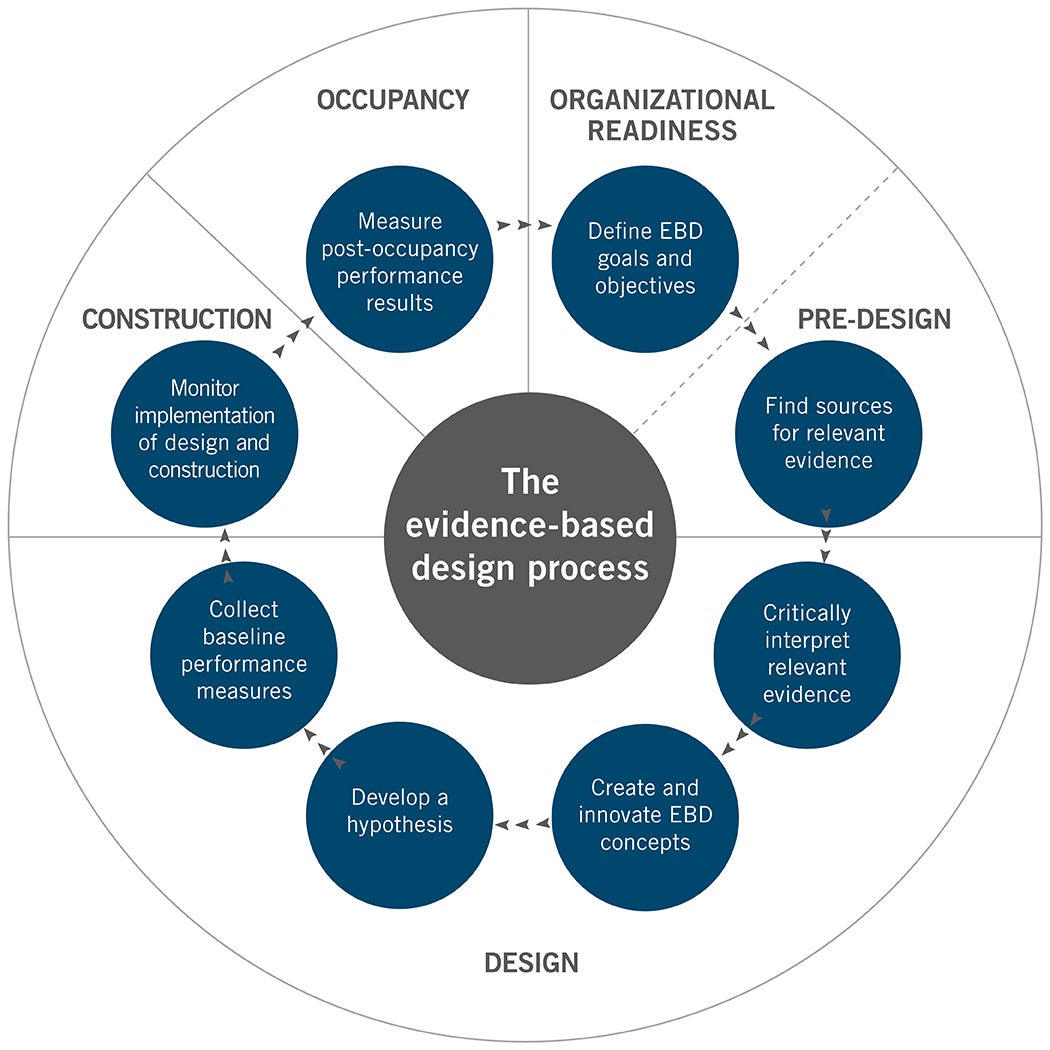
There are eight steps in an EBD process that are integrated into the typical phases of a design process (see the graphic above at left). Although the steps appear linear, some steps may be repeated during different phases of the project.
What is Lean? Lean methodology has evolved from improving manufacturing and business processes into improving delivery of care and design and construction processes.
Applying Lean starts with defining and maximizing Lean methods. Tools and templates are used to identify areas of improvement and test the future state before creating the new standard for work. The foundation for Lean is respect for people and continuous improvement, focusing on effectiveness and efficiency — doing the right things with the right resources in the right way (see the graphic above at right).
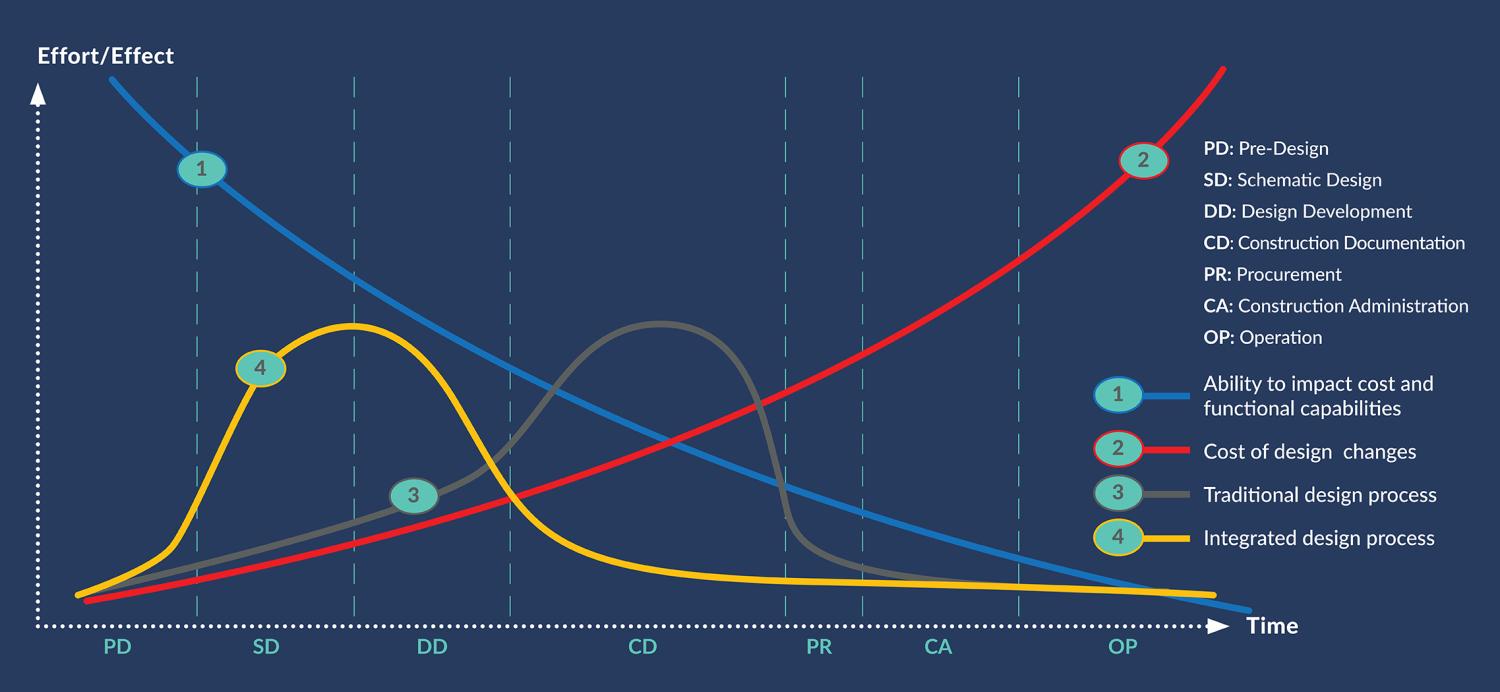
Why EBD and Lean? Applying an EBD process and Lean methodology is powerful when combined to create evidence-informed, effective and efficient physical environments. The business case for an integrated approach considers the optimal time for decisions to have the greatest impact on the project while minimizing costly redesign or missing opportunities for innovation (see the graphic at right). This mindset shift considers value beyond first costs, the needs and expectations of stakeholders, improved outcomes and the life-cycle return on investment.
To address today’s challenges with informed designs, EBD and Lean need to go hand in hand. By integrating these value-based approaches during the planning, design, construction and occupancy of a project, teams can maximize project outcomes while improving performance.
In a 2017 study co-sponsored by The Lean Construction Institute and The Association of General Contractors, called “Lean Construction Institute Designer Satisfaction Survey”, there was significant correlation between very high Lean-intensity projects and likelihood for better project outcomes and excellence in design. Lean intensity refers to the extent a project used the Lean methods studied, particularly those that are recognized as most effective.
Planning and predesign
How will the team know when it is right to combine EBD and Lean? The following conditions provide the best opportunity:
- The health care system is ready to look at its processes and how they can inform design.
- The health care system is ready to spend time upfront gathering data to inform design.
- The team is ready to invest the time to link design to measurable outcomes.
- The team is ready to evaluate and prove the design achieves the measures of success.
All projects should begin with the creation of an interdisciplinary team (IDT). In many projects, the full team is brought on board as the project progresses, creating silos and potential rework. Onboarding all disciplines at inception creates opportunities for increased collaboration and innovation by leveraging the input and perspectives of a diverse team.
In addition to the typical design partners, the IDT may include the contractor, researchers, trade partners, vendors and representatives from the community, patients and families.
Adding implementation partners at the beginning of the project provides them with the opportunity to understand the intention of design choices and the design detail. This can result in the implementation team becoming the vision keepers, ensuring that critical design strategies are not value-engineered, losing intent or being removed in construction.
Once the IDT is formed, time should be taken to align. Creating the vision, guiding principles and goals for the project together ensures everyone has the same North Star for the project. These become the guideposts for the team as they make decisions and are the first things shared when onboarding new team members.
Issues and challenges
Understanding the current state is an imperative first step for any project. If the baseline isn’t captured, it’s impossible to know the improvements to make and evaluate whether the future design made a measurable difference.
Current-state capture can be accomplished through observation, surveys or interviews. The successes and pain points uncovered inform the development of the future state. There are a variety of Lean methods and tools that can be used to understand and evaluate key issues and challenges, including:
- Gemba walks. This is going to the place the work is done, observing and questioning to uncover the successes and pain points.
- Scenario-based simulations. This facilitates the engagement of multiple stakeholders in the design process, ensuring systematic interactions and feedback between the user and the environment.
- A3 problem solving. A tool used to collaborate on a problem, research topic or big idea that promotes transparency and collective analysis as the team works toward a recommended solution.
- Paper dolls and seven flows. This allows teams to test the plan against the seven flows of health care, rapidly changing the configuration of a typical clinic module in response to ideal workflows and experience.
While this work is being accomplished, the IDT can start looking for existing evidence. This information can come from benchmarking, site visits and/or conducting a literature search. Research questions should be written to focus the search. There are many sources to look for existing research, including search engines, online journals or databases.
Once the literature review is completed, the team begins to review the information to determine if it is reliable, valid, relevant and applicable to the project. It is hard to know where to start or what would be considered credible.
One of the best places to begin is The Center for Health Design’s Knowledge Repository, a free, user-friendly database that continues to grow with the latest peer-reviewed publications about health care design research.
Design, construction, evaluation
Data gathered from the Lean studies is combined with the research gathered from the literature review. The translation of this collective information becomes the foundation of knowledge used to develop a future design and solutions to address the identified issues.
Once a future-state design is developed, it should be tested before construction. Evaluating adjacencies and planning flow is accomplished with a “paper dolls” exercise and then transitioning to use 3D mock-ups with progressing levels of fidelity.
This testing provides stakeholders with the opportunity to experience the space and discuss changes to operations. Evaluating ideas to ensure optimal performance is paramount.
At Piedmont Atlanta Hospital’s Marcus Tower, the goal was to complete a first-run study to not only confirm operations but also test the constructability and reduce costly changes impacting rework and the construction schedule. There were 76 refinements uncovered in this high-fidelity mock-up (see image below), resulting in zero changes in construction.

Lean study data combined with design research informs testing of future designs, like this 3D mock-up at Piedmont Atlanta Hospital’s Marcus Tower, reducing costly changes.
design and Image courtesy of HKS Inc.
When the project moves to construction, annotated diagrams are completed that illustrate and link design strategies to outcomes. These diagrams are used to communicate design intent to the construction and implementation teams. Together with the contractor, members of the project team should monitor the project to ensure that design strategies are built as designed.
Finally, it’s important to close the loop and evaluate project outcomes at least six months after occupancy by completing either a rigorous post-occupancy evaluation or design research. Measuring and evaluating post-occupancy results and sharing the findings and lessons learned at conferences, in research reports and by publishing the results in peer-reviewed journals ensures transfer of knowledge to the field and that lessons learned are used to inform future projects.
Project example
In one representative project designed by HGA, CentraCare was seeking to combine its hospital and clinic into CentraCare – Redwood Hospital in Redwood Falls, Minn., a critical access hospital on one campus to create efficiencies that address rural health care staffing shortages.
A study was completed before the project began to evaluate existing conditions. The result encouraged innovation in a new care platform and assessed the merits of using a universal platform (UP).
The IDT kickoff meeting started with education on Lean methods and tools and how they would use an EBD process throughout the life of the project. Also at the kickoff meeting, the project team defined critical to quality (CTQ) goals and objectives. These CTQs were used throughout the project to measure and help inform decisions. The team participated in gemba walks, staff interviews and value stream mapping.
The research team reported that there was little precedent or research about designing rural hospitals that combined shared and standardized patient rooms. Several articles discussed the concept of sharing rooms between departments, but few articles were research-based. This drove an integrated approach to combine and translate the knowledge gained from the review of literature and the knowledge gained from using Lean to innovate, ideate and test new design concepts to inform this new care delivery model.
During design, the solution of an UP and combining departments resulted in the following hypotheses:
- Increased access to more (universal) rooms would help as different departments’ volumes changed during the day.
- Shared departments would improve access to additional team members for staff assist or emergencies.
- Combined departments would reduce space, leading to a positive budget impact.
After completing the design, stakeholders discussed their involvement and next steps to evaluate outcomes, which included pre- and post-occupancy evaluations, pre- and post-procedure staff surveys, and data collection for length of stay and utilization of rooms over time.
Overall, findings from a staff survey indicated few differences between the existing spaces and the new space, likely due to moving from siloed departments into shared spaces. However, in the open-ended responses, staff loved having a medication room and the larger patient rooms. Results from shadowing data demonstrated that nurses are more efficient in the UP design, with less time spent traveling and transferring patients.
Original estimates for patient room need based on emergency department volumes were seven beds, and 12 for the surgical services pre- and post-procedure areas. The UP concept and the ability to use the same beds early in the day for surgical services and later in the day for emergency services allowed the number to collapse to 12 new rooms around a single unit or platform.
The overall square footage planned for the original design of these two departments (excluding waiting areas) was 16,690 square feet — with no shared patient rooms. The final design that included the UP (excluding waiting areas) was 7,300 square feet. As a result, the project realized construction cost savings of slightly more than $3.8 million.
This example illustrates how an integrated EBD and Lean approach led to innovation, leveraging research findings and client data, and solutions that improved efficiency and effectiveness with resulting cost savings.
Foundation and framework
To achieve desired project outcomes, team members and health care systems must align on priorities and the best problem-solving approach. The answer is using a combination of both EBD and Lean.
EBD’s use of credible research to highlight solutions with proven results complements Lean’s focus on eliminating waste, maximizing value and continuous improvement.
Together, these complementary approaches will form the foundation and framework for project success, benefiting all stakeholders involved.
While it can seem overwhelming to project teams that are unaccustomed to this type of integration, changes can be paced to achieve incremental progress. By starting small, these teams can build confidence and competence en route to even greater gains and integration on the next project.
Related article // Resources to learn about EBD and Lean certification
More than 3,000 professionals — health care providers, designers, architects, construction engineers and product manufacturers — have achieved certification in evidence-based design (EBD) through The Center for Health Design’s internationally recognized Evidence-Based Design Accreditation and Certification (EDAC) program.
Obtaining the credential demonstrates an understanding of the EBD process and how to apply it in the planning, design and construction of settings that contribute to health, safety, well-being and satisfaction. Certification also includes a commitment to measuring and sharing results with the field.
To obtain the EDAC credential, individuals must pass a 110 multiple-choice question exam. A variety of exam prep materials and assistance are available through The Center.
Health care projects or products that demonstrate exemplary use of an EBD process can apply each year for a Touchstone Award. Presented annually during The Center’s awards ceremony at the International Summit & Exhibition on Health Facility Planning, Design & Construction™, Platinum, Gold and Silver Touchstones reflect the level of completion attained in the EBD process.
The Lean Construction Institute’s (LCI’s) certification programs support owners and teams looking for people with verified Lean design and construction experience. Through completing the LCI Certified Professional – Design (LCI-CPD) and LCI Certified Professional – Construction (LCI-CPC) certification, individuals can show their nationally verified Lean experience and track record applying Lean principles.
- Learn more about EDAC certification and the Touchstone Award.
- Learn more about Lean certification.
About this article
This is one of a series of articles published by Health Facilities Management in collaboration with The Center for Health Design. The authors are contributors to The Center’s evidence-based design practice and EDAC certification program.
Andrea Sponsel, RID, IIDA, EDAC, LSSBB, LEED AP, is process improvement strategies leader and vice president at HKS; Terri Zborowsky, Ph.D., R.N., EDAC, CPXP, is design researcher at HGA; and Donna Deckard, BSN, MPA, EDAC, is director of strategic projects at The Center for Health Design. They can be reached at asponsel@hksinc.com, tzborowsky@hga.com and ddeckard@healthdesign.org.