Design innovation for stress reduction

Shell Point Retirement Community’s 200,000-square-foot Larsen Health Center includes a medical center, behavioral health suite, rehabilitation center, pharmacy, dental suite and a 180-bed skilled nursing facility with private rooms.
Image courtesy of Shell Point Retirement Community
Health care environments are universally recognized as high-pressure settings where stress can impact staff performance, well-being and retention. In senior living and acute care alike, leaders are exploring new ways to address burnout and emotional fatigue. These pressures affect not only the health of providers but also the safety and quality of care.
Shell Point Retirement Community in Fort Myers, Fla., partnered with The Center for Health Design to evaluate a neuroscience-informed, immersive relaxation kiosk designed to support well-being and reduce stress through calming imagery, guided breathing and binaural beats. Compact and self-contained, the prefabricated, modular Mind Pod was created by Florida-based Soul Happy to offer staff an easily accessible private space for restoration.
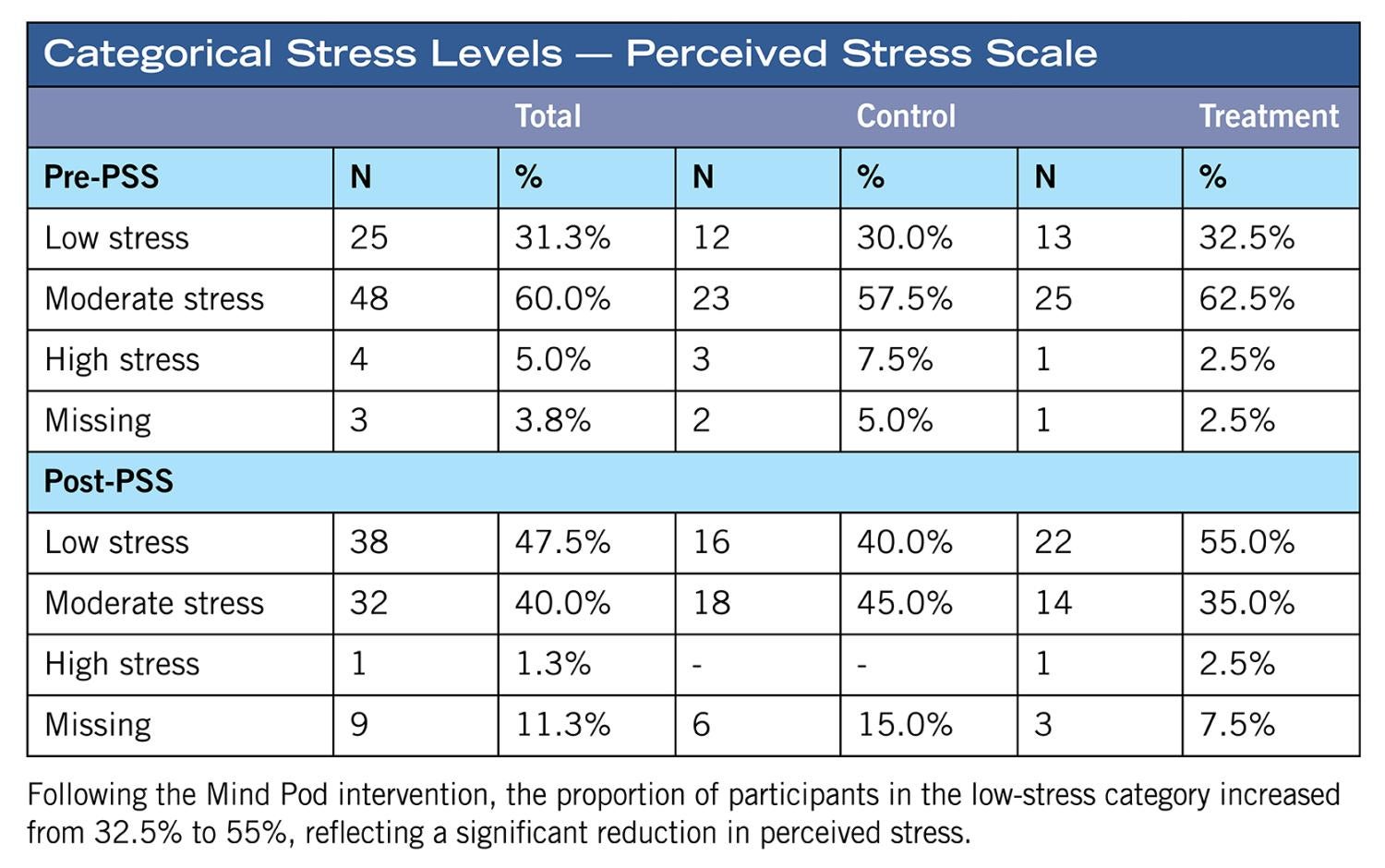
A proof-of-concept study with approximately 60 staff at Shell Point measured perceived stress and emotional exhaustion before and after use as part of a quality improvement project. Results showed statistically significant reductions in both measures, reinforcing the value of integrating restorative spaces and technology into care environments.
Addressing a critical crisis
Chronic stress among health care workers is a contributor to a wide range of negative physiological health conditions, including fatigue, headaches, digestive problems and sleep disturbances. The psychological impacts are equally serious, including anxiety, depression, lack of motivation and emotional exhaustion, all of which contribute to burnout.
More significantly, medical errors are the third leading cause of death in the United States, with a significant portion linked to staff stress, burnout and cognitive overload. When providers are overloaded, the risk to patients escalates.


A prefabricated Mind Pod kiosk utilizes neuroscience-informed, immersive relaxation techniques including calming imagery, guided breathing and binaural beats to reduce stress.
Images courtesy of Shell Point Retirement Community with interiors by Wegman Design Group
The organizational effects also are considerable. Reduced job performance, impaired clinical decision-making, high turnover and absenteeism are frequent outcomes. Providers are leaving the profession in record numbers due to psychological strain, creating recruitment and retention challenges. Replacing experienced staff is costly, and constant turnover disrupts continuity of care.
In senior living, staff often balance the physical demands of caregiving with the emotional intensity of supporting older adults in vulnerable situations. In acute care and behavioral health facilities, challenging environments add additional pressure. Across the continuum of health care, stress undermines performance and well-being, making it a critical crisis that organizations cannot ignore.
As leaders look for effective solutions, design-based interventions are gaining attention. Creating restorative spaces within the health care setting ensures immediate accessibility. Unlike programs that require time outside of work, on-site spaces allow staff to step away briefly, reset and return more focused and composed.
A self-contained prefabricated kiosk that can be delivered to any site represents one such opportunity. The Mind Pod is intentionally compact, evidence-informed and designed to offer respite in high-stress care environments.
Development and design
The kiosk approach was created to provide a brief, restorative escape from the demands of health care work. Inspiration for the unit’s compact design came from a lactation pod at Orlando (Fla.) International Airport. The enclosed structure suggested how an effective relaxation space might be embedded in institutional settings without major renovation.
Soul Happy co-founders Tracy Zboril and Cara Hewett, psychotherapists trained in clinical mental health and hypnotherapy, developed the concept as a direct response to the growing mental health crisis among health care professionals. Collaborating with human resources teams at local hospitals in Orlando, they began exploring scalable, evidence-informed interventions that could be integrated into high-pressure health care environments.
Drawing on their expertise in psychotherapy, hypnotherapy and the neuroscience of relaxation, they identified a need for private, accessible spaces where employees could engage in brief restorative practices during the workday. Their knowledge of brainwave modulation pointed to the value of incorporating altered states of consciousness — those linked with deep relaxation and stress regulation — into a self-guided format.

Of the seven choices offered, most participants viewed “Rest,” “Peace,” “Escape” and “Box Breathing.”
Image courtesy of Shell Point Retirement Community
The resulting prototype integrates therapeutic audio, guided meditation protocols, immersive audiovisual experiences and controlled sensory input to create a calming, neurologically supportive environment. Sessions are intentionally brief, typically lasting about five minutes, but are designed to help reduce anxiety, improve emotional regulation and provide a mental reset. A simple interface allows staff to select from multiple session themes, such as “Peace,” “Rest,” “Escape” and “Box Breathing.”
Several design elements form the foundation of the Mind Pod. Neuroscience-informed programming promotes relaxation and emotional regulation; multi-sensory integration engages sight, sound and breath; and a compact, self-contained footprint makes it adaptable to both high-traffic and private areas. Portability and scalability were central to the design: The unit can be installed in staff lounges, wellness rooms or other available spaces without requiring major renovation. By lowering logistical barriers, a prefabricated solution makes restorative design accessible to organizations that might otherwise struggle to provide such opportunities. Staff can engage with the space independently, without supervision or complex training, ensuring ease of use.
Shell Point’s information technology team worked with Red Dot Digital Media of Carlsbad, Calif., to customize the “in-pod” experience. Upon entering, users are asked to rate their current stress level and then choose from a series of videos ranging from deep breathing exercises and introspection techniques to faith-based content and calming imagery. Before leaving, they rate their stress again, providing immediate feedback on impact.
The media company also updated the hardware configuration, integrating a 32-inch touch-interactive digital display, and implemented the no-code content management system to simplify updates and reduce development costs. A reporting system supplies Shell Point staff with daily usage data, including which videos were selected and the before-and-after stress ratings, offering a practical way to track outcomes over time.
Implementation and evaluation
Shell Point Retirement Community embedded the project into its existing wellness culture and worked with The Center for Health Design to evaluate the system’s efficacy. Approximately 60 staff at Shell Point participated, completing pre- and post-use surveys on perceived stress and emotional exhaustion. The study was structured as a quality improvement project.
The Mind Pod was available on-demand in a designated quiet room. Staff were able to select from seven video relaxation themes. The most popular choices were “Rest” (23.3%) and “Peace” (22.5%), followed by “Escape” and “Box Breathing.” The least selected was “Renew,” which also was the only option that did not produce a statistically significant change in stress.
Half of participants visited the Mind Pod 16 or more times, showing consistent use. Desired frequency of use averaged about twice per week, and 76% of respondents said they would continue to use the Mind Pod if given the opportunity. Validated measurement tools included the Perceived Stress Scale and Maslach Burnout Inventory (MBI). Results demonstrated:
- Statistically significant reductions in perceived stress scores in the treatment group (p<0.001).
- Statistically significant improvements in the MBI subscales of emotional exhaustion (p=0.03) and personal accomplishment (p=0.02).
- Gains in stress reduction and emotional exhaustion also were observed in the control group, suggesting potential external factors such as organizational changes or concurrent stressors during the study period.
Demographic analysis showed varied influences. Role, sex, age and years of experience all played some part in outcomes, but the small sample size limited the ability to draw firm conclusions. Feedback also revealed practical considerations, such as requests for more video variety, volume control and adjustments to the door and seating for comfort.
Despite limitations, the results showed this well-being kiosk concept provided meaningful stress relief during the workday. Participants described it as “a calming getaway” and “a wonderful tool to decompress,” underscoring its value as a supportive resource for staff.
Outcomes and broader application
The study demonstrated statistically significant reductions in both stress and emotional exhaustion, with participants reporting that even brief sessions provided a calming reset during their workdays. While the pilot was conducted in senior living, the results indicate potential for use in many high-stress care environments.
Broader applicability is supported by several factors.
First, the quantifiable improvements in staff well-being metrics establish a foundation of evidence for adoption in other contexts. Health care leaders are under pressure to invest in solutions that show measurable impact, and the Mind Pod meets this criterion.
Second, consistent positive feedback reinforced the intervention’s perceived benefit. Staff valued the accessibility, emphasizing that the ability to step away briefly made a noticeable difference in their workday experience. The fact that most would continue to use it if available indicates strong user acceptance.

Embedding interventions into the physical environment shows promise to help improve staff well-being and support better patient care.
Image courtesy of Shell Point Retirement Community
Third, the adaptability of the technology supports its scalability. The compact and freestanding design makes it feasible to integrate into acute care hospitals, behavioral health units and rehabilitation centers. Unlike structural renovations, which can be costly and time-consuming, the Mind Pod can be implemented quickly with minimal disruption.
Fourth, while the Shell Point project did not directly measure organizational outcomes such as turnover or absenteeism, existing research suggests a strong link between reduced stress, improved retention and patient safety. By providing a reliable resource for decompression, conveniently accessible modular wellness spaces may contribute indirectly to these broader outcomes.
Finally, staff feedback about video options, sound levels and comfort highlights how small refinements can influence overall effectiveness. Continuous improvement based on user input can strengthen the intervention’s value across diverse environments.
These findings indicate that the Mind Pod represents a promising approach for addressing a critical health care challenge and demonstrates how intentional design can make a difference in daily operations.
Targeted tools
The Mind Pod represents one example of how health care environments can incorporate targeted, evidence-informed tools to address stress and burnout. By combining therapeutic design with brief, private access, it offers a scalable approach that complements broader wellness strategies.
The Shell Point project validated the potential in a senior living context, but the approach is generalizable. Staff used it regularly, reported positive experiences and demonstrated measurable reductions in stress and emotional exhaustion. While limitations in the study suggest the need for larger samples and broader testing, the underlying principles — stress reduction, accessibility and integration into daily operations — are directly transferable to acute care and other high-pressure care settings.
Related article // Programs for aging environments
The Resilient Aging Environments Network (RAEN) is one of The Center for Health Design’s network collaboratives. Established in 2024, the network was created for executive-level leaders involved in the planning, design and operations of settings that support health, safety, longevity and resiliency for an aging population. The network brings together diverse and forward-thinking members from care, design and solutions organizations who want to proactively contribute to advancing person-centered care.
With the support of The Center, RAEN provides dedicated programming and facilitated opportunities to members who drive conversations and topics of interest. Networking and communication, both in person and through an online forum, provide members with year-round access to learning, sharing, innovating, problem-solving and relationship-making experiences.
The evaluation of the Mind Pod well-being solution for addressing staff workplace stress discussed in the accompanying main article highlights the RAEN members’ interest in pursuing evidence-based solutions to advance the quality of care for residents and their families. The project also illustrates the increasing recognition that the care of staff is integral to the quality of care for residents. The opportunity to partner with The Center for an independent third-party evaluation of a project is just one example of RAEN members’ access to The Center’s research, education and community resources.
Sharing what has been learned — in regular “drumbeat” calls, deep dives and annual meetings — reinforces an aim of this dedicated group of professionals who are committed to shaping the future environments and the lives of older adults through thoughtful engagement and learning.
The recent September member meeting in Boston allowed members to tour multiple projects — The Pryde LGBTQ senior housing project, the Lasell Village lifelong learning community, the newly renovated Evans Park and the Chelsea Jewish Lifecare Community — learning more about the projects from residents, designers and care organizations.
A limited number of RAEN memberships are available for senior-level individuals in health care facilities and design and solution provider organizations. For more information, contact The Center for Health Design at info@healthdesign.org.
About this article
This is one of a series of articles published by Health Facilities Management in collaboration with The Center for Health Design. The authors are members of The Center’s Resilient Aging Environments Network. To learn more about it and The Center’s other networks, access healthdesign.org.
McKenzie Millis is executive director of The Springs and Connected Living at Shell Point Retirement Community in Fort Myers, Fla.; Ellen Taylor, Ph.D., AIA, MBA, EDAC, is vice president of research at The Center for Health Design; and Cara Hewett, MA, and Tracy Zboril, MSW, are co-founders of Soul Happy. They can be reached at mckenziemillis@shellpoint.org, etaylor@healthdesign.org, chewett@soulhappy.com and tzboril@soulhappy.com.