Preparing hospitals for RTLS implementation

Clinicians can see patient information, status and location on a centralized electronic white board based on data generated by the RTLS system.
For all of the health care field's adoption of sophisticated new technology, health care has lagged behind when it comes to adopting real-time locating systems (RTLS). In fact, beyond such basic uses as aiding asset management, the broad range of benefits these systems can provide has been largely ignored.
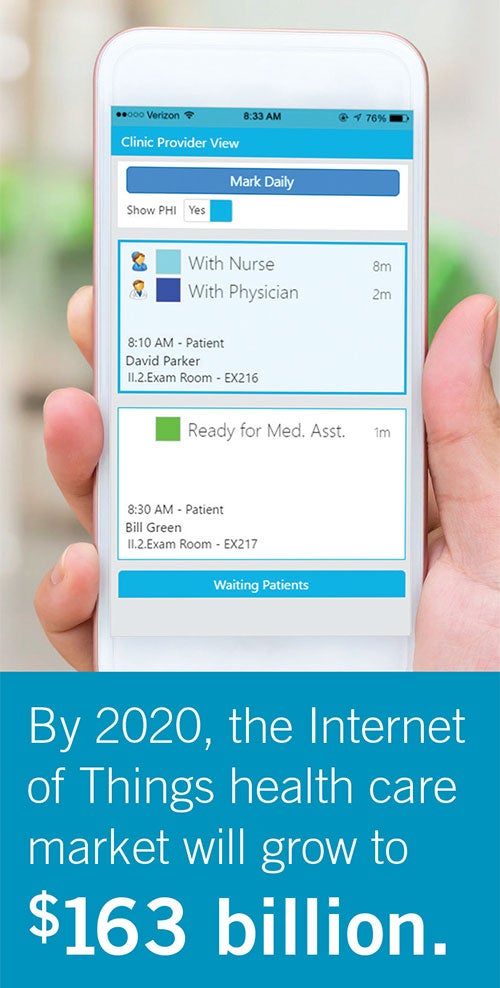
However, the Internet of Things (IoT), devices embedded with software or sensors connected to the internet, can help to drive the RTLS revolution in health care. By 2020, the IoT health care market will grow to $163 billion, according to research firm MarketsandMarkets Inc., Seattle, while the global location-based services health care market will grow more than 30 percent, according to estimates by Toronto-based Technavio. RTLS sensors, system integrations and analytics all play a part to take advantage of IoT devices and enable an approach customized to each facility’s vision and budget.
Health care facilities that are seeking to improve operational efficiencies and performance should consider these quickly developing technologies.
Powerful outcomes
A 2016 Forbes article about IoT trends points out that “we tend to focus on the glorified outcomes, but the mundane ones are equally if not more powerful.” For health care facilities, powerful outcomes might include increased staff efficiency, improved room utilization, process improvement and overall patient safety and satisfaction. With RTLS, a single technology can help providers to address all of those outcomes.
You may also like |
| Gaining a real-time view with RTLS |
| RTLS keeps workflow on track at two busy clinics |
| How an RTLS solution can help ES efficiency |
|
|
Deploying RTLS within the health care environment provides many benefits to patients, health care workers and health care operations. Consider patient safety, for example. With RTLS, facilities can initiate hand-hygiene compliance programs that match the tags on alcohol or soap dispensers with tags on staff, tracking utilization to ensure that employees follow proper hygiene guidelines.
Similarly, RTLS enables better tracking of staff member and patient interaction. In the case of exposure to a patient with an infectious disease, the appropriate parties — staff and other patients with whom the staff had subsequent contact — can be notified. RTLS also promotes patient safety by improving endoscope management: tagged scopes are tracked along each phase of the usage, cleaning and storage cycle.
Equipment tracking with the use of RTLS also saves time for facility staff. Being able to know the exact location of a tagged piece of equipment provides staff clear direction for retrieval — and ultimately allows them to spend more time with patients.
RTLS also can help health care facilities to improve department workflow in the emergency and surgery departments, where staff, patients and equipment are constantly moving from one area to the next.
Outpatient facilities are designing smaller waiting rooms and more exam rooms within the same building square footage by utilizing RTLS for patient rooming. As patients arrive at the facility, they receive an RTLS tag. Then, medical staff receive notification when these patients move to the exam room.
This improved rooming method reduces the overall number of steps that staff take each day to escort patients from room to room. Physicians can even have a mobile app that gives them easy access to their patient schedule for the day.
Patient experience
With the continued increase in consumer-driven health care, patients have more options — and often a greater financial stake — when choosing their health care providers. In response, health care facilities are increasing their focus on improving the patient experience, which translates directly into patient satisfaction, higher HCAHPS scores and, ultimately, more facility funding. Here, too, RTLS can be part of a successful strategy for achieving these goals.
For example, health care facilities that interface their nurse call systems with RTLS tags worn by staff can track both the response time after a call is placed and how much time nursing staff spend with a patient. Facilities are then able to analyze the data via RTLS software and establish goals for nursing teams. They also can transmit alerts to staff automatically when patients have been left alone for specified periods of time. These capabilities facilitate a higher level of patient-centered care.
RTLS also provides increased and improved staff communication to both patients and their families. Staff can reduce the amount of time they devote to such tasks as transferring patients from waiting rooms to exam rooms and searching for equipment — and spend more time providing care. Family members, meanwhile, are able to get real-time updates about their loved ones throughout a medical or surgical procedure.
Health care facilities are utilizing RTLS data to identify a variety of performance improvement opportunities in scheduling. With the technology, for example, they can rightsize staffing levels, correctly slot appointment times, and review and address scheduling bottlenecks. This information allows clinics to achieve faster throughput, without compromising the time spent with patients, and potentially to make more appointments available to patients each day.
RTLS planning
Planning for an RTLS implementation involves much more than the selection of RTLS hardware and software, although those are two important elements. For facilities to optimize the value of RTLS, it is imperative to bring key stakeholders into the planning process at an early stage to determine the facility’s vision and to document objectives for the project.
Begin by defining the challenges to address with RTLS. Is patient cycle time an issue? What about room utilization? Is optimizing patient flow this year’s key initiative? Once they have identified the goals, facilities professionals should identify appropriate metrics to track and measure improvements after system implementation.
First, they should take baseline measurements before implementation; then, monitor progress continually. It’s also important to identify bottlenecks or other issues that occur as unintended consequences of the new operational process.
Although operational planning and baseline measurements are part of the design and implementation process, staff expectations and buy-in frequently are overlooked even though they are critical to the overall system design and its success.
Consultants can spend hours defining the master plan and vision, work hand in hand with the health care system’s information technology department and provide all required infrastructure requirements needed to support the RTLS go-live. But it is unlikely to succeed if the staff who are affected by the system daily have not been included in the meetings or are left in the dark about the overall expectations for the system.
For example, an RTLS project calling for hospital staff to be issued tags so their movements can be tracked to reduce overall wait times in the emergency department and allow for higher throughput may seem like an intrusion to hospital staff if goals and expectations are not presented to staff up front so they understand the reason for the project.
Moreover, they must be presented to staff in plain language. Otherwise, terms such as workflow, operational analysis and Lean process may come across as yet another expectation for an overburdened staff to fulfill.
The staying power of an RTLS installation depends on its scalability. Different facilities require different applications and not all will have the same baseline measurements. Scalable, flexible solutions will help hospitals to grow and prepare master plans that can produce results.
Implementation of an RTLS can be expensive. A standard asset management application with RTLS hardware and software for a 100-bed hospital can cost more than $500,000. Taking a phased approach to implementation can help, but only if the system initially purchased accommodates future expansions, upgrades and capabilities.
Varying infrastructure also can help with RTLS scalability. Technologies such as Wi-Fi, ultrasound, radio-frequency identification (RFID) and Bluetooth low energy (BLE) each requires its own infrastructure planning.
For instance, Wi-Fi tags can run off the hospital wireless access point infrastructure for tracking facilitywide and across the enterprise. Ultrasound and RFID tags require separate Category 6 cable infrastructure to support hardware needed for room-level accuracy. BLE can be either wireless or wired and supports wayfinding, proximity-based, event-driven notifications and proximity-based remote authentication to workstations. Quality of service should be addressed to ensure that data are being transferred across the network appropriately and in real time without delay.
Integration of RTLS with other medical technologies transforms a standard equipment tracking system into a robust health care information system. The nurse call system, wireless phones, patient engagement software, electronic health record (EHR), digital signage, electronic wayfinding and patient wandering/security are examples of systems that can integrate with RTLS to provide a platform for optimal utilization.
For example, a patient who checks in at registration receives a badge that will be with him throughout his procedure and recovery. With integration to the nurse call system and EHR, the nurse can see the patient's information, status and location on a centralized electronic whiteboard based on the initial staff assignment. Once the patient’s procedure is complete, the nurse can assign educational videos to him; if he has certain medication risks or allergies, information from the EHR can then further customize that educational content automatically.
The assignment of the video to the patient (as well as a record that the patient watched the video) is documented in the EHR, closing the loop on the patient education initiative that helps to support reimbursement. Because the patient’s bed also has been assigned an asset tag, it is tracked through each department, provides data about clinical procedure throughput and helps to identify where bottlenecks are occurring.

Automatically collected RTLS data provide information on asset utilization and other operational metrics.
This information can be collected in a format that allows the department director to evaluate it in real time, so adjustments can be managed proactively. This is the definition of medical equipment and technology interoperability.
The next step in the planning stage involves taking the data generated by the RTLS and its integrations and making it useful operationally. Wearables, other IoT devices, mobile phones and RTLS all generate continuous streams of data. How can the health care field take advantage of the big data being created? The challenge is to filter out superfluous data and utilize only what is necessary for the application parameters that have been set.
Analytics is becoming increasingly important in health care. Analytics software can aggregate the data and provide real-time notification of improvements or continued areas of concern. This process, known as predictive analytics, is Level 7 in Salt Lake City-based Health Catalyst’s eight stages of the Healthcare Analytics Adoption Model.
Having the means and methods to gather specific data securely, incorporate it into the proper software tool and distribute it efficiently can have a dramatic effect on the overall system design and health care planning process. If analytics is part of a facility’s overall vision, it should be evaluated early in concert with RTLS, the EHR and device integrations to address data center planning and network infrastructure.
Some RTLS software vendors build analytics into their software platforms, while others utilize third-party platforms to manage and distribute the data. Many health care facilities have begun to adopt analytics as part of their operational planning and are seeing an immediate impact.
Finally, any health care technology system that requires detailed planning and design must also have a process in place to manage change, including the RTLS. Having a change management process can correlate directly to success or failure as technologies mature or new standards are adopted after the initial system design is complete.
To that end, facilities should rely on a core group leadership council, operating on a schedule of periodic reviews. Revisiting the process, studying outcomes and acting on information are critical to the effectiveness of interoperability.
Continued push
Market factors will drive continued growth in RTLS as the imperative to control costs necessitates improved efficiency and as the quality of the patient experience is linked to reimbursement.
These factors, combined with consumer expectations, staff shortages, a continued push for reduced wait times and further development of IoT will make RTLS an important part of every health care delivery platform in the near future.
Failing to plan for RTLS based on clear objectives, appropriate metrics and staff input, coupled with a strategy for scalability and flexibility, is simply planning to fail.
Josh Kelly and Nikki Tuft are senior technology consultants at Mazzetti+GBA, a global provider of health care mechanical-electrical-plumbing engineering design and technology/information technology consulting. They can be reached at jkelly@mazzetti.com and ntuft@mazzetti.com.





