Seven factors to monitor in power system operations

Power system components such as switchgear and switchboards require regular attention.
Image by Getty Images
A few decades ago, the health facilities professional’s main activity with regard to facility power systems was running the unloaded generator weekly or monthly, and then shutting it down to take some readings. Sometimes, facilities professionals also turned circuit breakers off to relocate or fix the equipment they powered.
Now, they must consider designing for reliability, rules for acceptable equipment locations, installation acceptance testing and commissioning to get new equipment installed.
They also write utility management plans, emergency operations plans, policies and procedures. Then, they conduct detailed inspections and testing, mandatory maintenance and equipment shutdowns, watch power system load profiles and watch the loading grow.
Facilities professionals need detailed training. They also must conduct risk assessments, vulnerability analyses and assess vulnerability mitigation. Additionally, facilities professionals should do detailed contingency planning for equipment failures, considering more severe weather conditions, increasing probability of cyber threats, a less robust electrical power grid and other factors.
Key areas
What are some of the key issues regarding health care electrical system operations? The following overview touches on issues from planning emergency power systems through developing contingency plans in case of failure and many issues in between:
Planning for demand loads. An article in the November/December 2019 issue of Health Facilities Management magazine titled, “Powering up to meet today's health care technology demands,” discussed in detail the likelihood of increasing emergency power demand loading, as well as increasing normal power demand loading, in health care facilities.
As more modern electrical equipment is installed, the likelihood increases of having an electrical power management system to monitor and report feeder and branch circuit loading, peak demands and other equipment parameters, such as event analysis.
These systems should now be able to provide both the normal power and emergency power load profiles as well as emergency power loading during load tests and real-time emergency power loading.
Available documentation. Availability of record drawings, manufacturer’s recommendations, actual equipment loading, protective coordination studies, electrical system one-line diagrams and arc flash studies should be verified. Some important documentation includes:
- An emergency power system maintenance program.
- Chapter 6 of the National Fire Protection Association’s NFPA 99, Health Care Facilities Code, has some inspection, testing and maintenance requirements for the essential electrical system (EES).
- Chapter 8 of NFPA 110, Standard for Emergency and Standby Power Systems, has inspection, testing and maintenance requirements for the emergency power supply system (EPSS), which is a part of the EES if the alternate power source is one or more generator sets.
- Normal power system maintenance programs (as with all other utilities, an inventory is required).
Additionally, organizations subject to the Centers for Medicare & Medicaid Services (CMS) conditions of participation are required to have copies of manufacturer recommendations for inspection, testing and maintenance.
An option to manufacturer recommendations is an alternative equipment maintenance (AEM) program if the organization has in place a CMS Tag A-0724-
compliant AEM program. The organization is required to meet its commitments and must be able to prove it when requested during surveys.
Testing requirements. The testing requirements have not changed much for several years. However, the testing records must be very clear and should always be checked and vetted before being filed. A test failure needs to be recorded, the cause of the test failure then must be corrected, the equipment then must be retested and the retest “pass” then needs to be entered into the records as well.
Depending upon the equipment or subsystem being tested, there may be additional requirements to assess and mitigate related risks to life safety, infection prevention and control requirements, or other patient safety risks.
NFPA 110 has for more than 20 years under sections 8.4.2, 8.4.2.1 and 8.4.6 required EPSS testing to be monthly; however, NFPA 99 has for the same period (including section 6.4.4.1.1.4 (A) “Test Criteria” in the 2012 edition and 6.7.4.1.1.5 (A) “Test Criteria” in the 2018 edition) required that same testing to comply with a 20- to 40-day interval requirement.
Not all organizations realize that satisfying all authorities having jurisdiction may require simultaneously complying with both interval requirements.
Training needs. As equipment becomes more complex and the compliance rules become more rigid, training is more important. Facilities professionals must be trained on more complex manually operated equipment, new technologies, and the equipment used for repairs and adjustments.
Personnel must know how to operate specialized equipment such as main-tie-main switchboards, generator paralleling switchgear, and automatic transfer switches with either a manual bypass-isolation feature or an automatic bypass-isolation feature.
Personnel also must know how to operate the intelligent control and communication features built into modern electrical service entrance equipment, switchboards, generators, paralleling switchgear, automatic transfer switches (ATSs) and uninterruptible power supplies (UPSs).
Recognizing the rapid evolution of electrical power monitoring systems into much more robust and complex electrical power management systems (EPMS), facilities professionals should be sure that operational knowledge doesn’t rest with just one individual. In some organizations, an entire EPMS became unused when the only employee who knew how to operate it left the organization.
Many power equipment inspections are mandated now by CMS rules. They are important because of the increasing reliance on these power systems for patient safety and patient care. When inspecting, facilities professionals should know what they are looking for and why; what is important; and what is reported, when and why.
The mandatory testing requires detailed records that are likely to be scrutinized by surveyors a few years from now. Facilities professionals should know how to assess the test results, whether the forms meet today’s requirements, and when the last time a form was vetted against surveyor expectations.
Maintenance programs. There are several sources for guidance in establishing or improving electrical maintenance programs, including the manufacturer’s recommendations; the equipment operating and maintenance manual; NFPA 70B-2019, Recommended Practice for Electrical Equipment Maintenance; and ANSI/NETA MTS-2019 Standard for Maintenance Testing Specifications for Electrical Power Equipment & Systems.
The Occupational Safety and Health Administration also requires an electrical safety program. The electrical safety program requires accurate electrical power system studies to determine overcurrent protective device coordination, arc flash hazard incident energy and numerous other related parameters such as approach boundaries and required personal protective equipment. NFPA 70E-2018, Standard for Electrical Safety in the Workplace, is the recommended standard for establishing and managing an electrical safety program.
In most cases, safe electrical equipment maintenance requires an equipment shutdown. Equipment modernization also requires shutdowns. An American Society for Health Care Engineering (ASHE) monograph titled “Managing Hospital Electrical Shutdowns” provides guidance for planning and conducting shutdowns of normal power system equipment as well as portions of the EES.

Infrared thermography is useful in assessing equipment condition.
Image by Getty Images
Organizations with an AEM program can consider predictive maintenance (PdM) of the normal power equipment and those portions of the EES whose maintenance is not governed by law and regulation. The PdM may take the place of manufacturer-recommended preventive maintenance, also typically known as calendar-based maintenance.
Historically, the most common PdM approach for health care electrical power equipment has been regular infrared thermography of the equipment. The thermographic results were then used to determine where corrective action was indicated.
Infrared thermography is important because it allows the facility management professional to identify deteriorating components before they cause a catastrophic equipment failure, thus leading to an unscheduled outage and major repair or replacement costs.
An electrical power management system with internal equipment monitoring devices can acquire numerous condition-based parameters and provide PdM output to the organization’s facility management professionals.
Failure and its impacts. Many health care organizations are dealing with the fragility of older power system equipment due to age substantially beyond the equipment’s useful life, lack of maintenance (often called “deferred maintenance”), inoperable components or adverse locations. In some cases, retrocommissioning (i.e., improving existing equipment) or retrofitting (i.e., replacing existing equipment with new equipment) has been a viable solution.
The 2017 edition of NFPA 70®, National Electrical Code® (NEC®), has new guidance in Section 110 regarding reconditioned, refurbished or remanufactured electrical equipment. The 2020 NEC edition has new equipment marking requirements in Section 110 for reconditioned equipment.
Fragile power equipment has a greater probability of negatively impacting operations. Fragile equipment is more likely to fail, and, as a result, the organization needs to have immediate resources for repairs.
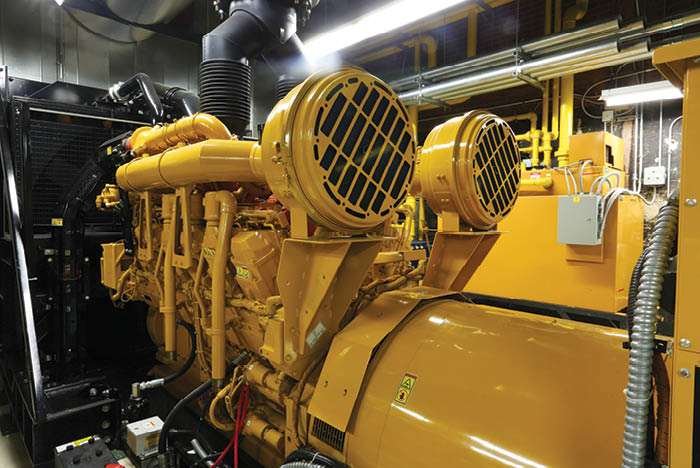
Regulations mandate generator inspections, testing and maintenance.
Image by Getty Images
The 2017 NEC generator docking station requirement for new construction and modifications has begun to apply to existing facilities in some situations. NFPA 70-2017 Article 700.3(F), Temporary Source of Power for Maintenance or Repair of the Alternate Source of Power, requires exterior quick connect capability for single generator installations powering NEC Article 700 loads. Some organizations may decide to add a remote generator docking station to provide the ability to easily connect a generator in the event that the existing generator fails. In that case, this new requirement would apply.
When calculating generator run time, it is recommended that the fuel tank ullage (i.e., available space for fuel oil) be considered rather than the fuel tank capacity rating. It is also recommended that the refill order point plus refill time to deliver during the postulated emergency should also be considered.
Facilities professionals also should know the impact of electrical equipment failures on other systems and equipment. It is preferable to know the correct responses to the following types of situations before the situation exists rather than after it commences:
- What does the impact of a life safety (LS) ATS or LS panel or LS riser failure mean? Is it necessary to do interim life safety measures/alternative life safety measures? And, if so, in what areas?
- What is the impact of an equipment branch (EB) ATS, or EB motor control center or EB distribution panel failure? Is an infection control risk assessment required because of the high likelihood of losing critical area ventilation equipment, or even important but noncritical care area ventilation equipment and in what areas? What new technology loads have been recently added to this equipment, and what impact will the loss of power to that equipment cause? Is security or other equipment powered by this source?
- What is the impact of a critical branch (CB) ATS or CB panel or CB riser failure? How will that loss impact direct patient care, and in what areas? Is immediate corrective action necessary to continue safe patient care while repairs are performed, verified and completed? Similarly, what new technology loads have been recently added to this equipment, and what impact will the loss of power cause to that new equipment? And what will others need to do meanwhile? How will they find out?
- In the event of a feeder or branch circuit failure, what will the team do?
Contingency planning. Electrical utility power grids and incoming utility services from utility substations to health care facilities may be more fragile now than in the past. This can result in a higher probability of utility power failure to a health care facility even if that has not previously occurred. The historical mindset of “It’s never happened here before — why should I worry now?” can become problematic.
A 2014 study by ASHE and Eaton, Cleveland, found that the frequency of electrical utility outages affecting hospitals has been increasing. The Federal Emergency Management Agency (FEMA) has indicated that facilities are more vulnerable to power outages than previously.
A Department of Energy technology review indicated a trend toward more frequent and intense weather-related electrical power grid disruptions with major disruptions every few years, along with the potential for cyber and physical attacks on the electrical power grid.
Additional resources are the Department of Health and Human Services’ Sustainable and Climate Resilient Health Care Facilities Initiative (SCRHCFI) and SCRHCFI Best Practices Guide Toolkit for Vulnerability Assessments, which can be accessed at https://bit.ly/2W214bt.
Other articles have discussed the growing threat of cyberattacks on critical infrastructure SCADA systems, including electrical power grids.
Some approaches to reduce power failure vulnerabilities could include hardening critical equipment locations to prevent damage, improving emergency planning and procedures to limit the consequences of power failures, contingency planning for restoration of service including identifying available spare equipment, upgrading controls, improving redundancy and improving communications.
Important elements
Health care power systems are important infrastructure elements upon which much of a hospital’s activities rely.
The areas discussed in this article provide considerations on which health facilities professionals may focus as they get their arms around these increasingly complex systems.
David L. Stymiest, PE, CHFM, CHSP, FASHE, is a senior consultant at Smith Seckman Reid, Nashville, Tenn., specializing in engineering and regulatory compliance. He can be reached at DStymiest@SSR-inc.com.