A facilities approach to preventing infection

Construction activities can lead to penetrations that can become pathways for infection.
Image by Getty Images
Over the past 10 years, the U.S. has made meaningful improvements in preventing health care-associated infections (HAIs), yet infections remain a major cause of death and disability. In addition to being incredibly dangerous to patients, HAIs also are costly because hospitals are generally not reimbursed by the Centers for Medicare & Medicaid Services for treating these infections.
To fully address this problem, hospitals have encouraged every department, including those once considered beyond the realm of patient care, to prioritize HAI prevention. As a result, infection prevention should be a significant part of a facilities department’s mission.
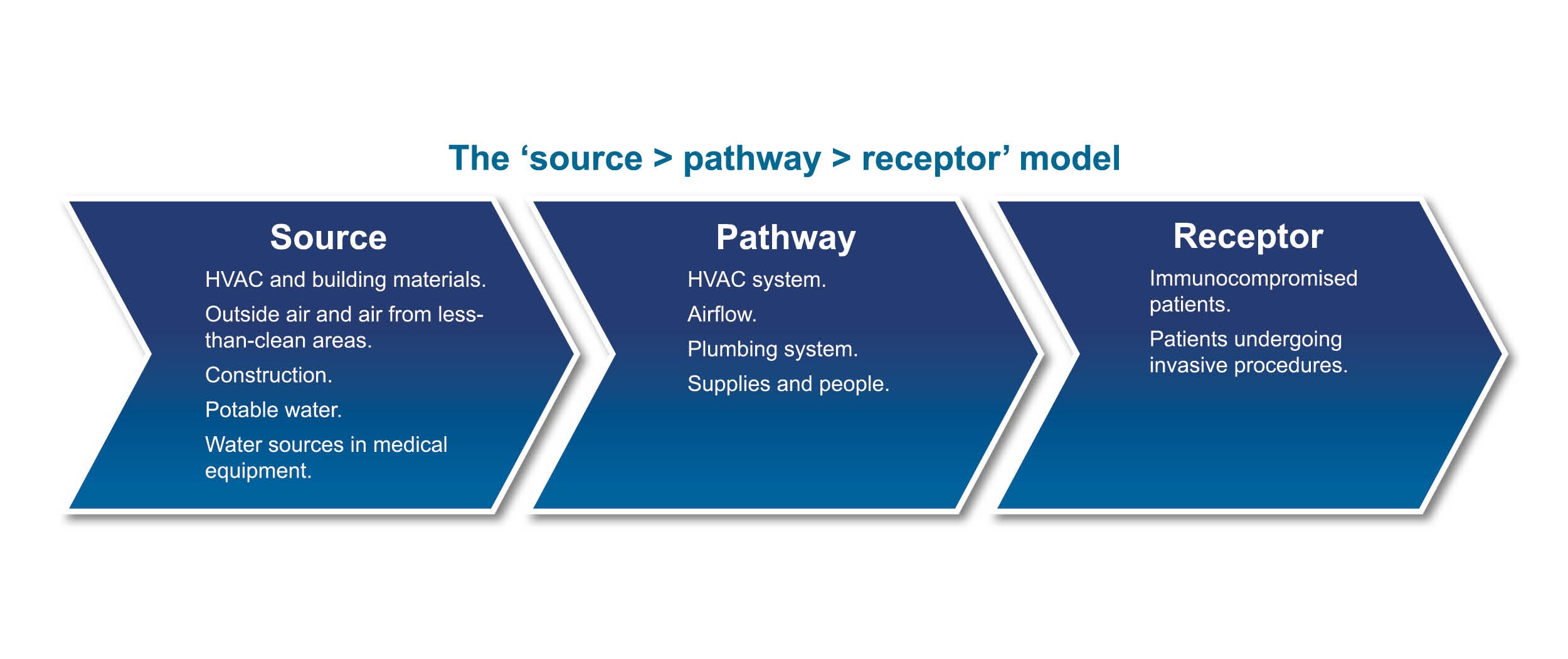
To strengthen the impact facilities managers and engineers can have on infection control, this department needs to build strong partnerships with the infection prevention professionals tackling this challenge from other areas. Facilities professionals also should ensure they understand the “source > pathway > receptor” approach to how infections are transmitted to break the chain of infections more effectively.
Most importantly, facilities departments need to reevaluate how they’re monitoring high-risk patient care areas — including intensive care units, operating rooms (ORs), radiology and other areas — to better mitigate risks present in and around these areas before a problem occurs.
A great way to accomplish this is to implement standing orders through an infection control risk assessment (ICRA) 2.0 process for those maintenance activities that warrant infection prevention risk assessment. These standing orders, once developed and approved, provide facilities staff with guidance on how to properly approach maintenance services within the patient environment. (For more information on ICRA 2.0, see the “ASHE Resource” box on page 39.)
Stronger partnerships
When facilities managers communicate with infection prevention and control (IP&C) professionals about how building systems work and infection preventionists share evidence-based perspectives to prevent infections, both professionals can better provide necessary support in stemming the transmission of HAIs. In fact, infection control and facilities professionals often find this to be one of the most important peer relationships they can have within the hospital.
In many instances, these departments already work together at times, connecting for environment of care (EC) rounds, water management meetings, and infection control and EC committee meetings. If facilities directors delegate some of these responsibilities, it is a good idea for them to represent their departments on these rounds and committees from time to time to gain insight into an infection control team’s concerns.
Understanding the infection control team’s concerns means speaking the same language. Infection control personnel tend to focus on laboratory data to gauge the presence of unusual infections or clusters, while facilities directors are focused on maintenance and operations. It’s critical to communicate more effectively around areas of overlap, such as opportunities for HAIs to develop around complex air and water delivery systems.
Signs of an effective relationship and strong communication include being able to work together to solve problems. These two departments can apply the source > pathway > receptor model to work together on preventing HAIs. Often IP&C professionals are skilled in source identification and facilities managers in pathway identification; though, in some infection clusters, these are very complex and specific expertise is needed. This is especially true when air pressurization and water systems are the pathway for opportunist microorganisms.
The source > pathway > receptor model is a simple yet effective approach for understanding how infections are transmitted. It relies on an understanding of the typical sources and pathways of infection transmission to better protect the receptor — in this case, patients, staff and visitors. Sources of microbiological infections include people, construction or renovation work; water-damaged building materials; water systems and medical equipment containing water; and equipment that can house infectious organisms such as fungi, bacteria and viruses.
The pathway is how the infectious agent gets to the host. Examples of pathways include people, equipment and supplies used in surgical procedures, water systems, ventilation systems and airflow.
Mitigating mold
Mold is found in all environments indoors and outdoors. In fact, it’s nearly impossible to create a space where there are absolutely no mold spores — especially in an environment where people are present. Even in hospitals, there is a low incidence of fungal infections that is considered typical, based on the inherent risk of clinical practice and certain procedures.
To prevent HAIs to the extent possible, it is critical to prevent the indoor amplification of mold to prevent dangerous fungal infections and clusters. To mitigate this risk, it’s important to first identify common sources of mold and then consider the pathways for carrying these infectious spores to vulnerable individuals. Typical sources include:
- Construction and renovation activities such as demolition and building processes that can disturb contaminated building materials or soil that harbors mold spores.
- Mold within buildings caused by water damage or high-humidity conditions.
- HVAC systems, which may host mold growth within the system or carry mold spores from outdoor air through or around the filtration system.
- Clothing of patients, visitors and staff as well as contractors.
- Equipment or supplies from contaminated areas.
To mitigate these risks, it’s important to take proper precautions before renovation or construction activities, in addition to regularly monitoring systems and rooms for evidence of water damage, water intrusion or high humidity levels. Facilities professionals should consider taking proactive air samples to assess mold risks in highest risk locations to identify any potential issues before they lead to infections. This monitoring also will allow them to gauge a baseline for indoor mold spores to compare any aberrant results against.
Environmental surveillance rounds should include assessments of evidence of water damage, interviews with staff in high-risk areas about local mold or water intrusion issues, and a review of HVAC preventive maintenance procedures.
Water issues
Waterborne pathogens are another dangerous source of infectious outbreaks. While Legionella has been a primary concern among health care facilities in recent years, it is not the only waterborne pathogen found in hospitals. Other pathogens include Mycobacterium and Pseudomonas, which can be found in air conditioning equipment, potable water systems, some medical equipment and other systems that may house stagnant water.
Fortunately, many of the strategies used to control Legionella growth can be used to reduce the risk of other waterborne pathogens as well. Many of these strategies are laid out by The Joint Commission’s (TJC’s) new water management standard EC.02.05.02, which focuses on preventing Legionella in health care building water systems through the implementation and ongoing operation of a water management program.
The updated standard requires a water management program, led by a clearly identified team or designated individual who holds responsibility for implementation and regular updates. The written water management program should include a diagram of all water supply sources, treatment systems and control measures, processing steps and end-use points.
The water risk management plan should address stagnant water and water monitoring protocols for ensuring stagnant water falls within acceptable ranges for control measures. It’s important to note that water monitoring does not have to and should not focus on the presence of Legionella bacteria. There is evidence that some facilities managers are focusing too narrowly on the presence of a problem rather than broad, potential risks. Monitoring can include other broad parameters that indicate that a plan is effective.
These water monitoring protocols also should include clear steps for corrective actions to be taken or procedures to be followed should the water fall outside of those acceptable ranges, or when a probable or confirmed waterborne pathogen case is identified.
TJC will be looking for evidence that hospitals are holding water management team meetings. Facilities professionals should prepare to have documented meeting minutes that demonstrate the effectiveness of the water management program and any monitoring or mitigation activities performed.
For additional guidance and information, readers can view the Compliance+Operations article on page 44 of this magazine.
Air pathways
Air distribution creates a pathway risk for infections because it can carry viral, bacterial or fungal particles through the air to potentially immunocompromised patients. Unfortunately, this continues to be a challenge for many organizations because it is one of the more common findings during surveys within the physical environment.
Depending on the purpose of the room and the condition of the patient, airflow must be directed either into or out of the room. For example, if a patient is immunocompromised, the airflow should be directed out of the room to prevent infection from spreading to the patient during their weakened state (positive pressurization). When the patient is the source of the infection and must be in an isolated space, airflow should be directed into the room to protect others and keep the infection from spreading (negative pressurization).
These pressurizations can be easily impacted by the offset between the supply and exhaust air as well as the tightness of a room. It’s this latter point that tends to be easily overlooked, in part because very simple changes can contribute to major problems. Room tightness can be impacted by factors as simple as missing door sweeps or as significant as wall penetrations.
A common example of this challenge tends to occur within central sterile departments. These departments typically consist of two back-to-back rooms separated by a washer or disinfector. The “clean” side must remain under positive pressure, while the dirty side must maintain negative pressure. However, these rooms can become leaky if the spaces between the washer are not sealed.
While gaps can pop up in construction, these airflow issues more typically arise over time as updates and their resulting penetrations are made to spaces. It’s important that any checklist for measuring compliance with pressurization parameters also address the tightness of a room. Many times, these challenges can be solved through a simple fix.
However, as facilities managers work to solve pressurization issues, small changes to a facility’s mechanical system can lead to other airflow problems. For example, in warmer weather, operating under negative pressure can lead to bringing in excessive outdoor air, heavy with humidity. If the mechanical system is unable to sufficiently dehumidify the air moving in, these damaging levels of relative humidity can lead to mold growth. On the other hand, low relative humidity can promote the transmission or suspension of viral particles in the air.
It’s important that after making any change to airflow, related factors be checked for change as well.
Construction dangers
Construction activities can lead to penetrations that can become pathways for infection. Construction also can be a source of dust and other contaminants such as Aspergillus that can result in HAIs if transmitted to patient areas.
The pre-construction risk assessment (PCRA) and the ICRA processes for managing construction activities are not new. However, deficiencies in the process still happen. Breakdowns often are related to the following areas:
- Communication and planning. It’s too easy to overlook minor factors such as door seals that can lead to major pressurization problems. Communicating with project partners to determine what to add to a project checklist can help. The core stakeholders to include in these construction meetings include a combination of facilities teams and infection control practitioners.
- Relative pressure. Failure to consider adjacencies during construction work can lead to problems with pressure outside the area being monitored. It’s important to think about — and measure — areas next to the construction space and the pathways that connect them.
- Monitoring to verify containment measures. Isolating construction work within health care facilities through a containment system is a standard practice. Verifying the effectiveness of a complete barrier is not. It’s critical that any containment system be inspected to ensure it’s a complete barrier and to ensure its pressurization.
- Complex and dynamic projects. Some projects simply create too many infectious risks or pathways for such risks to ensure effective containment using standard best practices. For example, one recent project involved removing the side of the building, making it impossible to maintain negative pressure in interior spaces.
- Not including end users. Involving the individuals who work within the facility is crucial for gaining insight into potential problems that need to be addressed and in driving education of end users to look out for problematic construction issues. Nursing staff is potentially the most important stakeholder to include because it tends to speak for the patient care unit.
Monitoring high-risk areas
Combinations of strategies can be applied to high-risk areas. In some cases, this can be as simple as increasing the frequency of environmental tours. Conducting these multidisciplinary rounds monthly might better mitigate issues in certain high-risk areas, such as ORs. This also can be accomplished daily at the line level, by the nursing team or clinicians.
In fact, training staff to speak up when they notice any sort of anomaly in the environment can prove incredibly valuable. Something as simple as a draft or water-stained ceiling tile in an area adjacent to these sensitive areas could signal a problem.
Technology solutions can be used to monitor these areas as well, and they range from the very simple to the very sophisticated. For example, monitoring space pressurization can be accomplished using a ball-in-tube pressure indicator or an electronic solution that can send an email or other alert in the event of a reading that moves beyond established parameters. The key is to have a system in place for checking and responding to these solutions regularly.
Through frequent, proactive monitoring of high-risk areas, facilities staff can develop more effective strategies for mitigating environmental risks. However, this is not a job that facilities teams should do entirely on their own. By working closely with infection prevention teams, environmental services staff, construction partners and end users, among others, hospital facilities staff can better monitor even the smallest changes that can have a powerful impact on infection transmission.
Through education on the source > pathway > receptor approach to infection, facilities teams can help end users better understand why building requirements are put in place. They also gain invaluable allies in the ongoing search for potential infection risks.
Treating an infectious pathway from patient to the nursing area
Negative pressurization has proven critical in isolating patients with COVID-19 and protecting staff from these viral particles. However, minor changes to a space can lead to potentially dangerous changes in pressurization, so regular monitoring is critical.
This was illustrated during one recent project, when a consulting firm was called in to determine if there were pathways by which the viral particles could travel from one patient room where a COVID-19 patient had been housed to nearby patient rooms or staffing areas.
The team began by monitoring the pressurization of the patient room in question, only to find it was at a slight positive pressure. A tracer gas study revealed that 30% to 60% of the infectious source material, when aerosol generator procedures were conducted, could be transmitted to a nearby nursing station, potentially putting staff at risk.
Once the pathway was identified and fixed, the space was tested again to ensure that the solution was effective.
Facilities team seeks pathway from moldy adjacency to ICU
After an intensive care unit (ICU) became the site of two fungal infections within 10 weeks, an investigation identified a possible source of mold on ceiling tiles in an adjacent resident on-call restroom. However, monitoring of the infected space showed that the ICU was correctly pressurized to prevent a pathway from which mold could move into the ICU.
A consultant was called in to determine by which other pathways the mold could be traveling into the ICU — or if there was another source to blame.
Upon interviewing the nursing staff, the team discovered that the door to the ICU room often stayed open. Because testing had been performed while the door was closed, the team monitored it once more with the door open.
The results showed that the slight change dramatically impacted the pressurization within the space, creating a pathway for the mold to travel from the resident on-call restroom to migrate into the ICU.
Fortunately, the repeated monitoring also presented a clear solution to this problem and steps to prevent it in the future.
Bryan Connors, MS, CIH, HEM, is managing principal consultant for health care at Environmental Health & Engineering Inc., Newton, Mass. He can be contacted via email at bconnors@eheinc.com.