The 'triple-demic' is on its way

Hospitals are examining their infection prevention procedures as they grapple with rising respiratory infections.
Image courtesy of Chicago Faucets
Doctors are warning that a surge in cases of respiratory syncytial virus (RSV) is coinciding with an increase in COVID-19 transmission and an earlier-than-normal flu season. With three respiratory viruses surging simultaneously (RSV, COVID-19 and the flu,) experts are dubbing this period the “triple-demic.”
The increase in RSV cases is partly due to the relaxation of COVID-19 precautions, such as masking and social distancing, which helped to reduce rates of both RSV and flu during the pandemic. And as the holidays approach, social interactions and travel increase, augmenting the potential for spread.
Flu cases are higher than typical for this time of year, per data from the Centers for Disease Control and Prevention (CDC). At the same time, RSV cases are soaring and COVID-19 cases are increasing as hospitals see higher positive rates. These rates are expected to worsen based on reports from Australia and Europe.
If each virus surges and peaks around the same time, this “triple-demic” could be a huge problem and would tax hospitals and health care facilities even more. Older adults, immunocompromised people and pregnant women are most at risk for COVID-19 and the flu, and young children are highly susceptible to influenza and R.S.V. Many infected children are becoming severely ill because they have little immunity, either because immunity in the general population has waned or because they were not exposed to these viruses previous to the pandemic.
“It’s always concerning when you have three respiratory viruses — RSV, influenza, and COVID — rising at the same time,” White House COVID-19 Response Coordinator Ashish Jha, M.D., MPH, said in an interview with CBS News.1 “If all three of them rise at the same time, again if people are not vaccinated, then we can start seeing a lot more hospitalizations.”
Increases in COVID-19, RSV and the flu infections have led to the current 'triple-demic.'
Image courtesy of Chicago Faucets
Hospital resources are operating at peak, but this extra demand may weaken care access as infections potentially become more prevalent.
Concerns for practitioners and infection prevention professionals include the increase in health care-associated infections (HAIs). In this scenario, the transfer of pathogens occurs either by direct contact with health care staff or from a contaminated environment or medical device.
Bloodstream infections remain prevalent, with the primary cause being central line-associated bloodstream infections. These contaminations originate from skin flora and are also referred to as the microorganisms that reside naturally on the skin. According to the U.S. Centers for Disease Control and Prevention (CDC), HAIs affect 1 in 31 hospital patients on any given day and can cause significant morbidity and mortality.
Below are other common causes of HAIs.
Surface infections. Public restrooms, laboratories and patient rooms all harbor germs. Even small surfaces such as water faucet handles harbor bacteria. While the length of time coronavirus is viable on a hard surface is still being researched, there is solid evidence for other germs like influenza and staphylococcus. According to an article published by the Mayo Clinic, viruses like colds and flu can last for several hours on a hard surface. And according to the (CDC), staph infections like MRSA can live on a surface for weeks.
Intensive care and infections. Nurses and doctors have cited time as the reason hand hygiene is falling off. Though gloves may be worn, that is not a substantial reason to skip hand hygiene, before and after wearing a glove as noted in the CDC brochure for patients and health care workers. A study conducted within intensive care units (ICUs) and published by the National Institutes of Health, showed, universal standard precautions with protocols that require health care providers to wash their hands with soap and water or alcohol-based disinfectants before and after visiting every patient proved successful in reducing the number of contact-based HAIs.

Hospitals are operating at a high level to keep up with patient demand surges.
Image courtesy of Chicago Faucets
A pediatric study published in Children showed that neonatal intensive care units (NICUs) with low rates of acquired infections have employed immediate and individual feedback to health care workers on their hand-hygiene performance and collective feedback to the NICU on acquired infection rates. In contrast, NICUs with high rates of acquired infections only communicated when there was a problem with the acquired infection rate and did not address improper individual hand-washing performance. Overall, throughout a health care facility, to reduce infections it is necessary to maintain a continuous training and reporting system for all health care workers.
Water-based health care-associated infections. The water provided in health care facilities can become infectious to patients due to the higher prevalence of pathogens found in these settings, leading to a variety of HAIs. Plumbing systems in hospitals require close monitoring and strict controls to reduce the rates of exposure and infection. For example, Legionnaire’s disease can quickly lead to an outbreak if not detected early.
Hospitals require aggressive clinical surveillance systems to identify contaminated water systems. If those monitoring the hospital’s plumbing systems discover any pathogens in their facility, it is vital to address the issue immediately. Hand hygiene in health care settings is a proactive control measure to prevent the spreading of water-based HAIs.
Key culprits in harboring infectious pathogens
Many factors put hospitals and long-term care centers at risk for harboring infectious pathogens in their plumbing systems, including:
- Large, complex plumbing systems that quickly migrate infectious pathogens throughout the facility.
- Increased temperatures within the plumbing systems that can contribute to colony growth;Warm, moist environments are ideal for the growth of bacteria.
- Low-flow systems with a propensity to stagnate and incubate pathogens.
- Startup and shutdown procedures that create vibration and release biofilms into the hospital’s water supply.
In addition to these factors, contamination can also spread from basins, sinks, showers, faucets and other devices such as humidifiers or hemodialysis equipment to patients. Even the splash-back of a running faucet can lead to an outbreak of HAIs in ICUs, and remediation may require the complete replacement of all the plumbing equipment.
Protect patients from Legionella
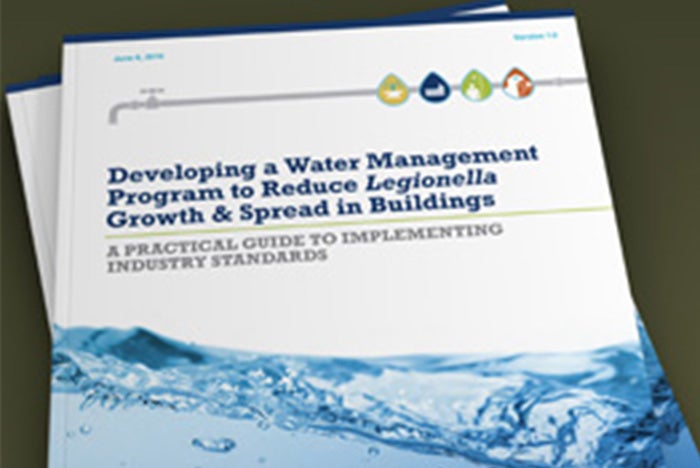
The CDC guidebook on managing Legionella provides valuable information on how to develop an effective water management program.
Image courtesy of Chicago Faucets
To protect vulnerable patient populations, the CDC published a guideline for preventing Legionella from growing in hospital water systems. Available since 2017, the guideline provides a comprehensive set of standards called “Developing a Water Management Program to Reduce Legionella Growth & Spread in Buildings.” The specifics of the guidelines include monitoring and prevention requirements for hazardous conditions in hospitals, nursing homes or assisted-living facilities. Based on the ASHRAE Standard 188-2018, Legionellosis: Risk Management for Building Water Systems, these guidelines are an easy-to-understand interpretation of how to develop an effective water management program for buildings
Internal and external building factors can lead to increased growth of Legionella. These include variations in the quality of the municipal water supply, changes in water pressure throughout the facility, temperature fluctuations during distribution and differences in the water’s pH levels over time, creating ideal colonization conditions. A water management program should consider all these factors to keep water sources safe for patients and staff.
Five steps to develop a successful water management plan
The current control measures deployed in most hospitals use filtration, chemical dosing and temperature technologies to reduce the number of pathogens and prevent exposure. Some of these techniques are more effective than others, and hospital administrators and facility owners need to find the right combination of treatment tactics to ensure that their water supply remains safe to use. Here are five basic steps to build a comprehensive water system safety plan:
- Establish a water management team for the facility.
- Describe the water system completely using text specifications and process flow diagrams.
- Identify monitoring points for water quality, and establish the necessary control measures.
- Review the efficacy of the plan, and update it annually based on documented results.
- Include contingency measures and response plans for any Legionella or other types of outbreaks.
Employing these five steps lays the foundation for water management program success.
Limit exposure with strategic upgrades
Replacing outdated plumbing with new technologies also helps to maintain or increase patient safety. It’s crucial that facilities managers educate themselves on and opt for newer health care products for water management. Here are key considerations:
- Select faucets specifically designed for patient care applications that offer quicker response times, reduce the need to wait for sensor-activated faucets, allow for setting time with a scrub mode and limit the tested microbial contamination.
- Select a shower system that comes with a thermostatic pressure balancing valve that removes water automatically when shut off.
- Select a shower system with an integrated drain that flushes water out of the pipes and shower hose after each use.
- Select showers or faucets that provide protection against scalding and prevent the crossflow of dangerous bacteria within the plumbing system.
- Select plumbing equipment that has been tested and validated by a nationally recognized testing laboratory.
- Select faucets and shower systems with programmable modes for hygiene flush, scrub, metering and cleaning.
While the “triple-demic” may be upon us this winter, there are proactive steps facilities managers can take to prevent HAIs. As Alan Lakein, the American guru on planning and time management, once said, “Planning is bringing the future into the present so that you can do something about it now.”
By Greg Hunt, commercial product manager for Chicago Faucets’ commercial product lines. He is a member of the American Society for Health Care Engineering and has his ASSE Legionella Water Safety and Management Specialist certification. Greg’s experience includes over 20 years in product management in a variety of industries.




