On the front lines of climate change

Large and small solar energy projects can be financed through investment tax credits.
Image by Getty Images
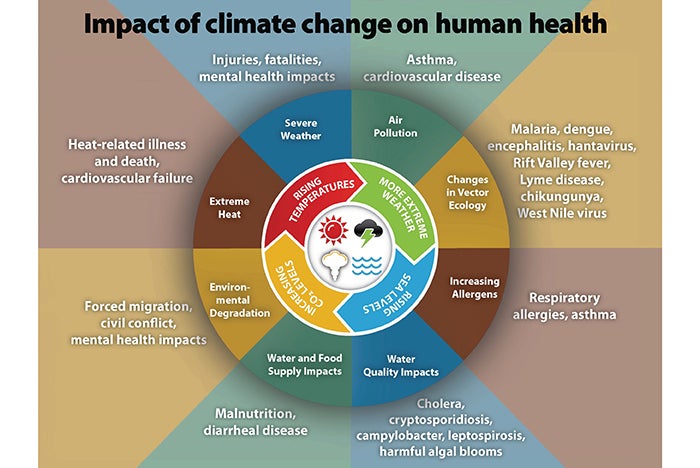
Climate change is continuously evolving, impacting weather and the environment. This affects the quality of air, water and food that is consumed.
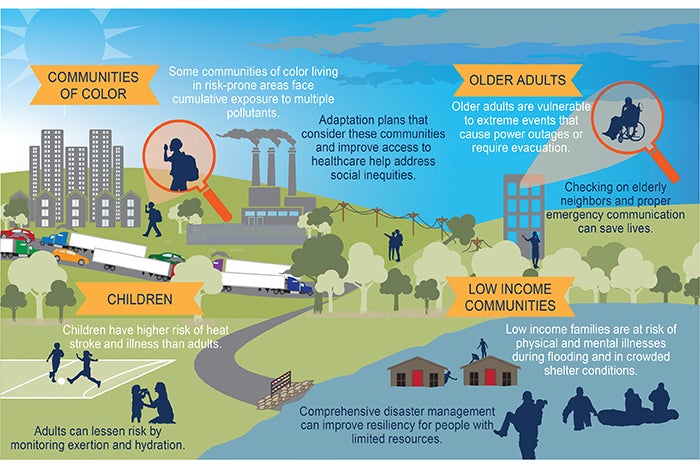
The most vulnerable members of society include children and the elderly, people with disabilities or chronic health conditions, individuals with limited access to health care and those who work a significant amount of time outside. For instance, climate change has contributed to increases in asthma rates among children, deaths due to extreme temperatures and the frequency of flooding, which impacts both property and health.
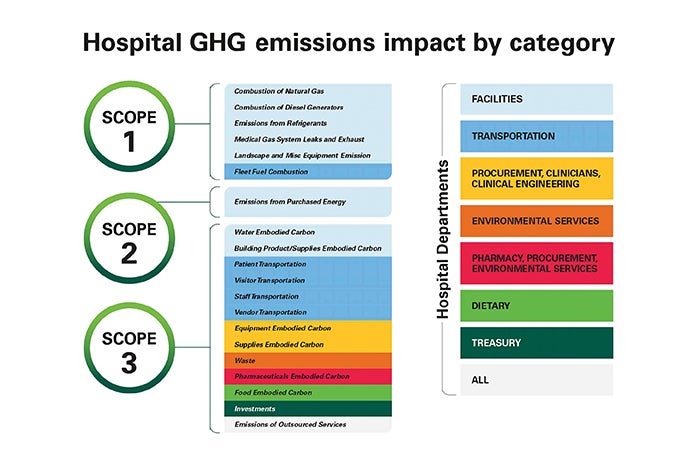
Health care is on the front lines of climate change, bearing the costs of increased illnesses and disease and the medical care associated with more frequent extreme weather events. Ironically, the health care sector also is responsible for 8.5% of U.S. greenhouse gas (GHG) emissions, with the U.S. health sector accounting for 25% of global health sector emissions.
As a professional field that is tasked with treating health conditions resulting from increased emissions and a contributor to these same emissions, health care has a profound role in climate change.
Intensifying demands
Demands to be more responsible stewards of the environment are intensifying every year. Initiatives are no longer being simply evaluated based on direct costs but more on the overall impact on society by reducing health care costs and improving the environment. Both the financial and social benefits of these initiatives far outweigh the direct costs of the initiatives themselves.
Due to their unique activities, their regulatory environment and 24/7 operations, hospitals consume a significant amount of energy, using 2.5 times more energy per square foot than office buildings. What’s more, health care organizations spend more than $6.5 billion on energy each year.
Renewable energy will provide improved price predictability as fossil fuel prices continue to increase. Legislation such as the Inflation Reduction Act (IRA) provides incentives to reduce the financial barriers to sustainability efforts, while legislation in multiple jurisdictions is intended to impose financial penalties for not reducing emissions and energy consumption. Utility companies are progressively investing in renewable energy. This, in conjunction with energy storage, will help hospitals remain operational during extreme weather events or periods of peak demand.
Some key points to consider include:
- Over the past decade, wind energy prices have dropped 70% and solar photovoltaics have dropped 89%. This trend is expected to continue as fossil fuel prices increase.
- Health care professionals and the public will continue to pursue career opportunities and seek medical care from companies that value sustainability.
- Sixty-four percent of the U.S. health care sector’s carbon emissions come from its supply chain, which is the production, delivery, use and disposal of the goods and services consumed. Hospitals must be able to deliver services even when faced with extreme weather events. Investing in resiliency, emergency preparedness and energy independence is imperative.
- Reduced building emissions are being targeted by legislation. More than 33 states have introduced, passed or enacted legislation to require buildings to develop action plans and produce results or face financial penalties. Only two states have currently enacted legislation, but this number will dramatically increase every year.
Pressures to decarbonize
According to the World Health Organization, the U.S. health care sector is estimated to contribute around 8.5% of the country’s total GHG emissions. This includes emissions from energy consumption, transportation associated with health care services and the production and disposal of medical products.
Health care’s contribution to GHG emissions can vary. The percentage of GHG emissions attributed to health care operations can depend on the region, size and type of health care facilities and the energy sources used. Additionally, larger hospitals, research institutions and medical centers tend to have a more substantial carbon footprint than smaller clinics and primary care facilities.
Efforts are being made within the health care sector to reduce its carbon footprint by improving energy efficiency, transitioning to renewable energy sources, adopting sustainable transportation practices, exploring the use of anesthetic gases and implementing environmentally responsible waste management. As these initiatives continue to expand and gain traction, the GHG emissions attributed to health care operations will decrease.
Due to U.S. health care’s contribution to GHGs, pressures are rising for health care to address the issue. Health care institutions are being compelled to adopt strategies that incorporate decarbonization, operational efficiency and other methods of reducing their organizations’ carbon footprint. Many health care institutions across the U.S. have made substantial progress while others are taking small steps to improve their sustainability and resilience.
Reasons for the move
The catalyst behind this sustainability movement comes from various factors, including the global ecological crisis and the standards and regulations that are being set by industry leaders and governmental entities. Some of the reasons health care is moving toward decarbonization and sustainability include:
- The Health and Human Services Pledge. The White House and the Department of Health and Human Services (HHS) launched the Health Sector Climate Pledge on Earth Day 2022, underscoring the federal government’s commitment to carbon reduction. By setting this standard, the HHS pledge directs hospital leadership to expand on the support to the communities they serve. It reinforces the idea that health care’s responsibility goes beyond patient care and encompasses a commitment to environmental stewardship. As of November 2023, 116 organizations representing 872 hospitals have signed the pledge.
- The Joint Commission’s Sustainable Healthcare Certification. The Joint Commission recently introduced its new Sustainable Healthcare Certification as an opportunity beginning in January 2024. This voluntary certification provides health care organizations with the ability to expand or continue their sustainability efforts while gaining recognition for their achievements.
The Joint Commission has increasingly turned its spotlight onto sustainability practices within health care facilities. This emphasis on sustainability reveals the connection between health care quality and environmental stewardship. It reiterates that health care institutions play a crucial role in the global challenge of environmental sustainability.
- The National Academy of Medicine. In response to the impacts of the changing climate, the National Academy of Medicine launched the Action Collaborative on Decarbonizing the U.S. Health Sector. The collaborative is a public-private partnership of health care sustainability leaders committed to addressing health care’s environmental impact and helping the field become more sustainable.
Despite these compelling reasons for health care decarbonization, this transformation presents unique challenges, especially for nonprofit health care organizations. Often constrained by tight budgets and the need to prioritize patient care, institutions may find the initial financial investments in sustainability initiatives daunting. Nevertheless, it is crucial to recognize that these investments are not merely ethical; they are financial imperatives. Over time, they can yield substantial cost savings and environmental benefits, which can bolster the long-term financial health of these organizations.
Legislative trends
Currently, 33 states have climate action plans, and 24 states have GHG emissions targets. State legislatures consider climate change to be a serious issue and are taking actions to reduce global warming. While most of these target utilities and state-owned properties, there is a demonstrated trend of emissions reduction legislation in various states and local jurisdictions. Two such examples are New York City and the state of Washington.
While the New York City law has exceptions for buildings that are 24-hour operations critical to human health and safety, it also gives owners of nonprofit hospitals and health care facilities an option for a percent reduction rather than a cap. While the option of a percent reduction may sound good for many hospitals, those that have been on the energy management journey for many years and have already seen reductions up to 35% need to take note of the caps, as this may be the better route to take. Also, many office buildings will fall outside of these exemptions and must comply.
Washington state passed The Clean Buildings Act in 2019, establishing a first-of-its-kind standard that will improve the energy performance of thousands of large commercial buildings in the state. Commercial buildings that are 50,000 square feet and larger must comply in phases, with the largest beginning in 2026 and most coming into the program by 2028.
The standard itself is based on an “energy utility index” — a simple measure of energy use per square foot. To account for widely varying energy uses between different commercial buildings and the influence of colder weather in the eastern half of the state, the standard is adjusted by building category and geography.
Washington also intends to reduce 70% of its net annual energy consumption in new residential and nonresidential buildings by 2031, compared with the 2006 Washington State Energy Code. It currently requires energy-efficient heat pumps for space and water heating in all new residential buildings, which is a move away from natural gas and propane.
On the federal level, there are several initiatives to encourage decarbonization and sustainability. They include:
- The IRA. Tax credits and deductions have been a longstanding resource for organizations involved in energy projects. However, for tax-exempt entities such as hospitals, accessing certain energy tax benefits was historically challenging. The IRA made changes to Section 48 and Section 179D to make it easier for nonprofits to benefit from these types of incentives.
- The Investment Tax Credit (ITC). Previously, nonprofits such as hospitals found it cumbersome to reap the full benefits of the ITC. However, the IRA provides lump-sum cash reimbursement to nonprofits equal to at least 30% of a project’s total cost. Moreover, the IRA has expanded the eligible projects, increased the amount and extended the timeline of the ITC.
The 30% ITC is available for solar projects that begin construction before 2033 and geothermal projects that begin construction before 2035, as well as standalone energy storage, qualified biogas, microgrid systems and qualified grid interconnection.
Smaller solar projects below 1 megawatt are automatically eligible for the 30% ITC, and larger projects are subject to more stringent requirements, including a requirement that contractors completing the project pay prevailing wages and have an apprenticeship program. The new ITC also provides bonuses for projects, which can increase the ITC by up to 70% of total project costs. These bonuses encompass rewards for domestic content, projects in designated energy communities and projects in designated low-income communities.
- The 179D energy-efficient property deduction. The 179D deduction (Internal Revenue Service Code Section 179D) provides tax benefits to renovate or build energy-efficient buildings. The changes to 179D decrease the efficiency requirement and provide provisions for nonprofits to benefit from the deduction.
Today, if a nonprofit hospital cannot directly use the deduction, the deduction can be transferred to the architects, engineers and contractors. Once transferred, they can be sold to other interested parties, including banks or other corporations. This will allow hospitals to negotiate to lower the final cost on eligible projects.
Furthermore, the qualification threshold for the deduction has been lowered from 50% energy cost savings to 25%, making it more attainable for hospitals. Additionally, hospitals now have the option of claiming a deduction on a specific building every three years, which is especially advantageous for hospital campuses with multiple building renovations and expansions. The value of the deductions is determined on a sliding scale based on square footage of the building and the energy savings achieved. The deduction value for projects meeting prevailing wage and apprenticeship standards is between $2.50 and $5 per square foot.
Leveraging tools like state and local incentives, as well as the IRA, ITC and 179D programs, can empower hospitals to engage in a wider range of energy projects, reduce their carbon footprint and lower overall project costs.
Health care’s journey
As the pressure intensifies for health care institutions to reduce their carbon footprint, the journey toward a sustainable future continues.
Through collaboration, innovation and a steadfast commitment to their core mission of healing, health care organizations can become beacons of responsible environmental stewardship.
Jessi Bienert, CEM, is vice president of sustainable solutions at Bernhard LLC, Metairie, La.; Kat Fink is director of utilities and energy management at Temple University/Temple University Health System, Philadelphia; Michael Roberts, PE, CHFM, SrHE, SASHE, is director of enterprise energy services at Atrium Health, Charlotte, N.C.; Scott Winfrey, PE, HFDP, LEED AP, is associate principal at Specialized Engineering Solutions, Omaha, Neb.; and G. Andy Woommavovah, CHFM, is system director of facility management, energy, infrastructure, and planning, design and construction at Trinity Health in Livonia, Mich.