It's the process
 The complexity of the health care environment requires an inclusive and collaborative approach to the design process. Designers must propose solutions that meet the needs of a facility operationally and financially as well as provide an environment that is conducive to healing. In this challenging era, the access, affordability and delivery of health care requires innovation of designers and caregivers to work together toward improving outcomes and defining new standards.
The complexity of the health care environment requires an inclusive and collaborative approach to the design process. Designers must propose solutions that meet the needs of a facility operationally and financially as well as provide an environment that is conducive to healing. In this challenging era, the access, affordability and delivery of health care requires innovation of designers and caregivers to work together toward improving outcomes and defining new standards.
In recent years, several health care organizations have dedicated themselves to rethinking every process by embracing the philosophies of Lean. And the effort already has begun to pay off in visible savings. Rather than build another new hospital based upon old models, these organizations have streamlined their operations to eliminate waste.
This has translated into the design and construction of health care facilities where project teams are looking at new ways of working, bringing forward a more efficient, collaborative process where the schedule is shortened and buildings are more efficient and effective.
Given the risk-averse nature of the health care industry, there can be many challenges to rethinking the old ways of delivering care. Health care can be siloed, sometimes resulting in redundancies, inefficiencies and unnecessary touch points for a patient. Similarly, the design process is fraught with inefficiencies.
Fortunately, there are different design methods that help facilitate the incorporation of Lean principles in health care operations. Moreover, specific design strategies can enhance Lean processes within the design firms themselves. Finally, standardization also can help achieve Lean goals.
Simulations and prototypes
Health care facilities are challenged to continually deliver care with fewer resources. There has been a high level of focus on the impact of the physical environment on caregivers' ability to deliver care safely and efficiently. Poorly designed physical environments can reduce the effectiveness of staff to provide care and potentially impact the safety of patients and caregivers.
To achieve a more efficient model of care, the entire team is asked to think beyond their current methods of working. Understanding health care processes before actually developing the space can facilitate resolution to the operational issues. In the spirit of Lean design, all processes should be driven by the patient's experience.
With this in mind, the goal is to create a model where all aspects of care — caregiver workflow, distribution of supplies and medications and clinical documentation — are pushed to the point of service. Hands-on exercises, including simulation modeling and prototyping, are effective tools that enable caregivers to explore possibilities more freely.
Simulation modeling. Simulation modeling can quickly assess the impact of change on a given aspect of flow. For one Chicago-area hospital, simulation modeling was a highly effective tool to test an outcome assumption of reducing its operating room case load.
An analysis of the current process in place included evaluating each of the steps in the process, applicable trends, impact of the process on staff and the technologies to be leveraged. The steps that were not considered value-added or that could be combined or automated were changed.
Following the definition of a new process, it was possible to determine how the new facility would be designed. The importance of this exercise was apparent when analyzing the costs associated with delays in case starts. By reducing these costs and the associated process steps by 50 percent, a savings of four nursing full-time equivalent employees was seen.
Methods such as this enhance communication, one of the key objectives of Lean design. All participants feel more invested in the process and are better equipped to provide commentary in an environment that supports all points of view. Additionally, the focus is placed on patients and their needs, identifying the places where redundancies and unnecessary tasks are performed.
Prototyping. To improve nursing efficiency and allow for increased nurse time at the bedside, a greater emphasis has been placed on the design of floor layouts and nurses' stations. Due to the myriad operational models and workplace cultures, there is no singular solution emerging. Prototyping is an effective means to validate assumptions to inform the design of future patient units.
This method can help meet needs quickly and effectively through the use of techniques that test theories related to positive outcomes. Prototyping methods encompass workflow, technology and processes.
Once process standards are established, the physical room prototypes can be constructed in a simple manner so that the workflow can be tested in real conditions. This allows for a variety of assumptions to be validated in a low-risk environment.
Rooms may evolve into a final, finished state where a number of design solutions can be evaluated, such as construction details, standardization of components, finish materials and color palette. This can allow both the design team and the contractor to confirm their assumptions prior to building multiple rooms.
The opportunity to collaborate and to discuss the best solutions can address issues often raised during the construction process, such as constructability, cost and final execution.
Flexible and modular design
One of the key principles of Lean is to create as much flexibility, scalability and adaptability as possible.
Flexibility. Because much of the planning in health care is for an unknown future, incorporating adaptability makes sense. Changes in work processes, equipment and technology can require costly changes to the physical environment. A flexible environment enables adaptation of design, space and the future state of practice over time.
One approach can be to design a patient unit that allows for flexibility for any medical specialty or acuity. Rooms can be sized and configured to be universal rooms, allowing for future flexibility to convert acute beds to a higher intensity of care with minimal renovation. The unit can be organized to support the optimal workflow no matter what the medical specialty and thus be standardized.
Modularity. For outpatient facilities, modular clinic designs can be used that allow for flexibility based upon workflow and scheduling. Shared reception and waiting spaces accommodate visitors comfortably while modules for exam rooms and their associated spaces support a standardized model of care and can flex according to a particular clinic's schedule for a given day.
Taking this another step further, the facility can be designed and built to enable future practices and allow continuous improvement with minimal cost or disruption. When considering the physical impact that modification to the care model can drive, work spaces must be designed to meet these needs, ranging from private spaces to support critical thinking to open, collaborative environments to promote care coordination over various disciplines.
Modular components and systems can enable modifications to be made easily with minimal disruption.
Development of standards
Standardization within health care organizations and design practices also may contribute to Lean processes.
Health care system standards. Many larger, multihospital systems are creating standards with the intention of using them comprehensively. Their goals are to streamline certain processes that are repeated for each and every project, including decision-making for the products specified and purchased.
Functionality of key rooms is considered. The goal for such efforts is to develop a best-practice standard. This creates a room organization and operational model that can be applied to future projects, whether renovation or new construction. This approach streamlines the planning process, eliminating redundant efforts and enabling the health care organization to maintain a consistent level of quality, provide a comparable patient experience and operate in a similar manner across the system.
Frequently, the development of standards is tied into a brand initiative. This can result in the design of specific components that patients may encounter throughout their journeys.
Design practice standards. The design process can benefit from some standardization as well. Work efforts can be structured so that processes and tasks that contribute value are prioritized and those that do not are eliminated.
Certain information gathered throughout a project also can be translated to future projects as standards, thereby reducing the amount of time needed for research related to specific, common elements.
Throughout the course of a project, designers find many redundant efforts. However, that information is rarely used to inform future work. Health care organizations are demanding that professionals
bring the expertise forward regarding innovation.
Most projects would benefit from referencing detailed information about the rooms included in a project at the outset. The focus then can shift to the specific needs of the organization, maximizing the time spent on innovation and streamlining the entire process.
Similarly, the analysis typically conducted on life cycle and performance of materials for use on one project should be considered more comprehensively for application on all projects.
One way to achieve this is to develop a comprehensive matrix of products that typically are specified in project work. Performance characteristics for each product can be listed, along with information related to first cost and life cycle cost. Data gathered from various mock-up installations also can be useful when products are considered.
These tools enable designers to identify quickly which products are suitable for a specific circumstance, streamlining this part of the design process.
Value and benefit
The incorporation of Lean principles can help a health care facility achieve optimal performance by improving strategic, operational and financial outcomes.
Patients are put at the forefront of the experience, leading to greater satisfaction. Additionally, patient handoffs and patient moves are minimized, leading to a smoother, more streamlined overall care delivery process.
Likewise, if done in a methodical and well-conceived manner, incorporating Lean principles into the design process itself can greatly enhance any health care project by improving the quality and efficiency of the outcome.
Jocelyn M. Stroupe, AAHID, IIDA, ASID, EDAC, is principal at Cannon Design, Chicago, and president of the American Academy of Healthcare Interior Designers. She can be reached at jstroupe@cannondesign.com.
| Sidebar - Northwest Community Hospital project puts mock-ups to the test |
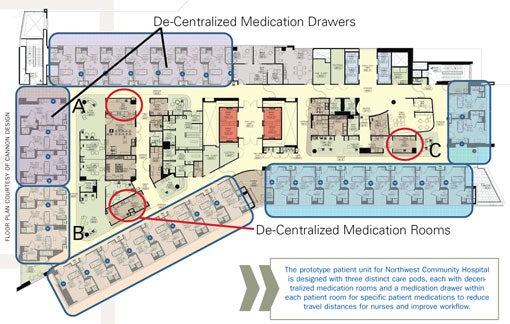
| Northwest Community Hospital's decision to build a new inpatient care unit at its Arlington Heights, Ill., campus was focused on three strategic goals: to move from the current semiprivate model for patient rooms to all private rooms in response to consumer demand; to position the hospital with the ability to adapt easily to a variety of acuity levels with minimum disruption to patient care; and to bring the building online as quickly as possible due to the competitive market in the area. A warehouse mock-up space called the "Vision Center" was conceived as a means to facilitate a fully integrated design process. Multidisciplinary teams were brought together that included clinicians, facilities, the design team and the construction manager. The results were standardization of rooms and patient units, simplification of construction details, streamlined decisions on products and a shortened construction schedule. The Vision Center was used to develop a prototype model. The goals set forth by the team stated that the patient population would be converted to a private room model with no increase in staff cost. Standardization of patient unit design would allow for ease of adaptation and conversion in the future. The patient rooms are designed to accommodate a larger caregiver work zone and have the ability to modify the entry door to a large, sliding breakaway glass door along the corridor for increased visibility and access. Adoption of a universal-size planning module was employed to allow for prefabrication and testing of repetitive units off-site. Patient safety was enhanced by the adoption of innovation and standardization of clinical protocols, particularly distribution of medications to the bedside. Each patient unit was organized into three distinct care pods, each with its own central supply storage, medication storage and team station. In addition, each patient room was equipped with individual supplies required for the patient on a day-to-day basis, including linens, supplies and medications. The caregiver is able to chart electronically in the room or in the team station. The operational changes made a significant impact on the time nurses spent walking from a single, centralized point of distribution. The team station has been designed with flexibility and collaboration in mind. Through the use of modular furniture, zones for work have been created to support workflow that are open and accessible or closed and private. The ability for the care team, comprising many disciplines, to collaborate and communicate has been accommodated with modular, demountable walls, allowing for future change to occur with minimal disruption. The design process and strategies used at Northwest Community Hospital effectively reduced inefficiencies in the building, budget and the schedule. Through Vision Center tours with staff and community members, the design team was able to confirm some assumptions and learned where it missed the mark on others. Surveys from the tours enabled a continuous feedback process. Through simulation of patient transport in the prototype, for instance, the design team discovered that wider, single-leaf entry doors to patient rooms were preferable to the double entry doors originally considered. The elimination of the double-door access to patient rooms yielded a net savings of $400,000. Moving to a private-room model increased the unit's size by 50 percent and achieved the goal of remaining staff-neutral. It also resulted in higher patient utilization rates, from 64 to 86 percent in the first six months. Due to the market fabrication of prototype room components, the project team was able to advance the project schedule, enabling the building to be completed three-and-a-half months ahead of schedule. |




