Shine on
 Today's health facilities professionals must factor in unprecedented oversight of every decision they make—not the least of which is deciding when and how much capital to invest in new or expanded facilities.
Today's health facilities professionals must factor in unprecedented oversight of every decision they make—not the least of which is deciding when and how much capital to invest in new or expanded facilities.
The average hospital or health care facility spends roughly twice the amount of a typical commercial office building to power its lighting. What's more, lighting accounts for 40 percent of the electricity consumed in such facilities.
While those figures are substantial, a hospital owner or facilities manager still may hesitate to reduce lighting out of concern that patient care and safety will be affected.
The good news is that advances in lighting control technologies are allowing hospitals and health care facilities to maintain a high level of care without increasing costs.
Properly applied, lighting control measures have a typical payback of two years, helping health care facilities reduce lighting-related energy costs by 35 to 50 percent. Moreover, health facilities professionals who implement lighting control systems to reduce operating costs often create the perception that their facilities are clean, modern, sustainable and conducive to convalescence.
But the key in achieving such benefits for facility ownership and management is understanding and clearly conveying during the design process how specific spaces within a new hospital or health care facility will be used.
That will dictate the appropriate lighting control technologies a consulting engineer specifies, and how they will be integrated into the building management system. These technologies include everything from a schedule-based lighting control system with overrides for administrative areas, to daylight-harvesting sensors in lobbies, to localized controls that allow patients to adjust the lighting, shades and temperature of their rooms.
Types of control
For decades, branch lighting circuits that powered lighting in hallways, parking garages and common areas in the typical hospital or health care facility were controlled by contactors or relays located adjacent to the lighting panelboard in an electrical room. But, as times have changed, so have lighting control technologies, and nowhere is this more apparent than with the intelligent lighting control panelboard.
An intelligent lighting control panelboard combines branch circuit protection and control into a one-panel solution. Thus, instead of having two panels—a lighting panelboard for circuit protection and a relay or contactor panel for control—engineers can now utilize a more robust intelligent lighting control panelboard that provides benefits like lower installed cost, more reliable operation, increased energy savings and a typical payback of less than two years.
 |
| Occupancy sensors can help health facilities professionals achieve significant energy savings as well as energy code compliance. |
There are several things that distinguish an intelligent lighting control panelboard from a typical lighting panelboard. Intelligent lighting control panelboards have a controller and motorized circuit breakers that can be remotely operated by the controller. While a standard controller typically turns lighting on and off based on the press of a button, a schedule or a photocell input, controllers in intelligent lighting control panelboards feature logic and connectivity options unavailable just a few years ago. Today's controllers can easily be integrated into building management systems using open protocols, such as Building Automation and Control network (or BACnet), over an Ethernet network.
Once integrated, controllers can share information, prioritize inputs and even employ logic to execute lighting control based on a combination of inputs, from button presses to HVAC controls and even security. Taking connectivity one step further, today's most advanced controllers feature an embedded Web server that allows the controller to be accessed over the Internet from anywhere in the world.
Additionally, some Web-enabled controllers have the ability to e-mail facility managers or owners when predetermined events occur, such as circuit breakers tripping or lighting circuits achieving a predetermined amount of operational hours. Having the ability to remotely determine when lighting should be replaced, or when to send an electrician to troubleshoot an electrical problem, is more than a convenience—it's a time and money saver.
Controllers also coordinate commands from other lighting control devices, like occupancy sensors. Such sensors are installed in areas where occupancy isn't predictable, turning lights on for a preset period of time when someone enters and off when that person has departed, usually within 30 minutes. Occupancy sensors typically employ either passive infrared (PIR) or ultrasonic technologies, or a combination of both, to avoid the false turnoffs that were characteristic of earlier designs. Another example of such devices are daylight or light-level sensors, which measure ambient light levels and automatically switch breakers or relays on or off to maintain a constant light level. They are typically installed in areas with large windows that allow large amounts of natural light.
Individual controls like keypads and touch screens have improved in style and functionality and offer a stylish alternative to traditional control devices. Keypads replace typical wall switches and activate individual lights or other room components, such as blinds, and can also be used to adjust HVAC levels for increased comfort.
They can feature light-emitting diode (LED) indicators that provide illumination and status feedback. Touch screens provide programming options to create preset lighting scenes that can activate automatically and control other systems, like audiovisual components.
Added benefits
These lighting control technologies can be applied across the gamut of spaces in a new hospital or health care facility to achieve diverse goals, such as patient comfort and safety, reasonable return on technology investment and reduced costs. But another goal is compliance with state and local energy codes. Perhaps the two most relevant codes and standards related to lighting control are the International Energy Conservation Code (IECC) and the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE)/Illuminating Engineering Society (IES) Standard 90.1.
Typically found within the building code of a health care facility's municipality, these two standards provide specific direction on the usage of multiple types of lighting control. For example, the latter requires automatic lighting control for all nonresidential buildings more than 5,000 square feet, including usage of time schedules or occupancy sensors.
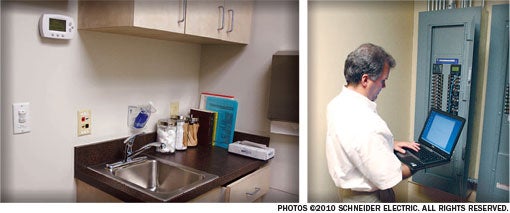 |
| LEFT Wall switch occupancy sensors can save energy that would otherwise be wasted to light unoccupied rooms or spaces such as exam rooms. RIGHT Intelligent lighting panels can be accessed on-site or remotely to configure the panelboard or access real-time data. |
Another example is the state of California's Title 24 energy code, which requires not only automatic shutoff controls, but also daylight control. Numerous states and municipalities have instituted their own energy codes, many of which are modeled on Title 24.
Application of lighting control technologies in a new hospital or health care facility is typically determined by a consulting or specifying engineer. But the conversation can be driven by health facility owners and managers and their desires, which is why it's crucial for health facilities professionals to present as much feedback as possible about how specific areas within a new health care facility will be used.
Appropriate solutions
Individual spaces can be divided into two types—front-end and back-end—each with nuances that suggest appropriate strategies and appropriate technologies. Their characteristics include the following:
Front-end areas. Front-end areas like lobbies, atriums, hallways, common areas, cafeterias and occasionally nurses' stations often have some natural light, which creates the opportunity to shed electrical loads through daylight sensors but also through occupancy-enabled bi-level control.
Thus, if nobody is present, artificial lighting automatically drops to 50 percent through either switching (i.e., shutting off some lights outright) or dimming (i.e., using a dimmable ballast and a control mechanism), with all changes coordinated by the controller in an intelligent lighting control panelboard. Dimming is usually the preferred choice for bi-level control because reduction of artificial lights is often gradual, imperceptible and, consequently, less disruptive.
In patient rooms, giving patients control over their lighting and HVAC preferences can be perceived as comfort control, but it allows nurses to attend to other work, which ultimately lowers the cost of health care by making them more efficient. In such cases, commands from keypads or touch screens made by patients are sent to the controller in an intelligent lighting control panelboard. Additionally, if the control is connected to the facility's building automation system, HVAC setbacks can be executed as well.
Application of lighting control in the parking structure and exterior perimeter areas can be challenging. Most parking structures have lights on 24/7 due to safety concerns, which can't be debated.
However, daylight-harvesting sensors can be installed around the perimeter of an above-ground parking structure to turn off some lights during the day via the controller in an intelligent lighting control panelboard. For exterior perimeter lighting, an astronomical time clock built into the controller can turn lights on precisely based on the time of the year. Photocells can be deployed as overrides in case storm clouds roll in.
Back-end areas. Schedule- and occupancy-based control are the core technologies in a lighting control strategy for back-end areas, which are typically invisible to patients and visitors.
Administrative offices, for example, usually have a large area with many workstations, and are typically in operation during normal business hours of 8 a.m. to 5 p.m. In such cases, schedule-based control will turn on all lights shortly before 8 a.m. and off again at a preset time after 5 p.m. Overrides for a set period of time, such as two hours, provide flexibility for those working late or coming in early, although occupancy sensors also can be used for such situations.
Such a strategy for administrative areas can add up to significant cost and energy savings. Application in a common office building can result in 10 to 15 percent overall energy savings; that savings can be accrued in the administrative areas of a hospital or health care facility, even though those areas occupy on average
20 percent of an entire complex. But that still translates to a 2 to 3 percent overall energy savings.
A combination of schedule- and occupancy-based lighting controls also can be leveraged in areas like loading docks and laundry facilities. They have their own business hours that will dictate a lighting schedule, but occupancy sensors can turn lights on for a preset time during off-hours. Storerooms and closets can operate almost exclusively via sensors.
Finally, lighting control even can be carefully applied to surgical areas. Lighting and, by extension HVAC, can be scheduled to turn on 30 minutes before a procedure or turned on remotely from a facility manager's workstation or by a nurse. The savings come from not having to light and heat an unoccupied area for a significant time.
Driving the discussion
The benefits of lighting control can only be gained through understanding all options and ensuring they are part of a facility's energy management strategy.
Health facilities owners and managers must consider these options when selecting lighting control systems for new or renovated hospitals.
Eddie Hickerson is a training and customer support manager with the Lavergne, Tenn.-based Installation Systems and Control business segment of Schneider Electric North American. He can be reached ateddie.hickerson@us.schneider-electric.com.
| Sidebar - Improving an existing system |
| Existing hospitals and health care facilities can benefit from the energy savings generated by today's lighting control technologies, all of which have a typical payback period of roughly two years or less. An important first step is to commission an energy audit, which will provide insight into many energy and cost savings opportunities, not just lighting. For example, an audit may note that a health care facility does not have adequate lighting control in its administrative areas or medical buildings, which can be easily addressed with a schedule-based lighting control system, via an intelligent lighting control panelboard that can be a like-for-like replacement of an existing lighting panelboard. However, if a health care facility does have a schedule-based lighting control system, it almost certainly will require retrocommissioning, especially if the system has been in place for more than five years. Whatever lighting control schedules were developed originally are probably either obsolete or possibly overridden. Either way, the full gamut of energy savings is most likely not being captured, and a retrocommissioning effort will address this and also verify that the system is still operating optimally. Another important key is occupancy sensors. Wall-switch occupancy sensors for storerooms, closets and patient bathrooms take only a few minutes to install, but can offer immense energy savings because they help ensure lights won't be left on for hours. |
| Sidebar - Achieving smart, functional lighting |
| The Joint Commission's Standard EC.02.06.01 states that the organization must establish and maintain "a safe, functional environment" and among its Elements of Performance is a requirement that "lighting is suitable for care, treatment and services." Like all other Joint Commission requirements, there can be consequences for noncompliance, which is why there can be a tendency on the part of ownership and management of new hospitals and health care facilities to maximize lighting upon initial occupancy. Doing so means lighting won't eventually be the source of an accreditation survey problem down the road. However, this strategy does little to aid the energy efficiency of the facility or complex and, ultimately, increases the cost of health care. Working with a consulting engineer to develop and execute a lighting control strategy can help shore up these concerns. However, as part of that strategy, health facilities owners and managers should document lighting control usage to show how it maintains a safe and functional environment and ensures that lighting is suitable for care, treatment and services. How documentation is developed is up to the facility, but it could include information such as the following: Annually reviewing and updating that documentation to verify that conditions haven't changed is also important. |




