Cost conscious
 Today's health facilities professionals must factor in unprecedented oversight of every decision they make—not the least of which is deciding when and how much capital to invest in new or expanded facilities.
Today's health facilities professionals must factor in unprecedented oversight of every decision they make—not the least of which is deciding when and how much capital to invest in new or expanded facilities.
A rule of thumb suggests that for every dollar in capital costs, health care executives must plan on spending $3 to operate the facility and another $10 to staff it over the life of the building.
Thus, achieving efficiencies in the design of such complex building environments as medical care facilities is not an option today, it's a necessity.
Doing so effectively typically requires strict attention to three strategies from the very start:
- Maximizing the initial capital investment;
- Incorporating sustainable, high-performance approaches that enhance the long-term cost-benefit of operations; and,
- Optimizing staff efficiencies in the facility.
Maximizing capital investments
The health facility on the drawing boards today looks and costs nothing like the one planned 20 or 30 years ago. Too many organizations make the mistake of planning the ideal building only to quickly realize that it's not affordable. Then begins the process of stripping away everything determined to be unessential, often at the expense of initial project goals.
However, managers and design and construction teams are much better served by employing an integrated project delivery process. This incorporates the various stakeholders' underlying goals up front, aggregating their perspectives, requirements and expectations within the framework of the budget.
Target value design can then assign costs for each building system, with the design and construction experts pulling together a budget for the overall facility, eliminating dubious "wish lists" yet incorporating the essential goals of the institution from the beginning and along the way. The client's goals and expectations are aligned from the start without need for redesign at the end.
For integrated project delivery to truly pay off, there needs to be an agreement between the owner, architect and contractor to maximize the approach and decisions, both in the beginning and along the way. Each team member must share in the ownership of the outcome and the impact of decisions, scale, systems, and construction materials and methods.
Everyone must pull together to ask what's the best that can be produced for the budget available and whether it meets the expectations for the project, the patients and the community. Awareness that this approach is particularly effective in aligning expectations and achieving goals is growing.
One recent example is the development of a new suburban campus for Seattle's Swedish Medical Center. This project to build the Puget Sound's first new hospital in 26 years is both ambitious and complex, serving the growing east side of Lake Washington, in the community of Issaquah.
The team decided a phased approach would be most appropriate, given the immediate requirement for ambulatory care. Thus, bed space would come later in the phased development, after the physician practices had been established.
The plan also called for the facility to incorporate a strong sense of community, which was important to the project's stakeholders and their local citizen advisory group.
To accomplish this, the building was organized around a five-story atrium space. A single set of elevators was provided for outpatients and visitors to ease their wayfinding. The atrium takes advantage of an accessible courtyard from the "living room space" facing it. Retail spaces bring a noninstitutional feel to the space and an education center is intended to support both hospital and community-based programs.
The design and construction portion of the budget was managed to meet expectations within the framework of the financial structure.
For another facility, Seattle's Northwest Hospital & Medical Center, the architect and contractor originally devised a five-phase plan to renovate the emergency department at this growing campus.
Such a phased building program would allow some continuing emergency capability during construction. However, the plan came in higher than budgeted and there was no more money.
The team took another look at the campus and developed a new approach, converting an older, underutilized wing on grade that was not up to code but had potential. A new plan was agreed to that upgraded the infrastructure to current codes and added a canopy for ambulances and relocated the emergency department.
While this initially seemed like it would increase scope and complexity beyond the renovated emergency department, it ended up saving five months of construction and $500,000 in costs. An added bonus was that the redesign provided a licensed contemporary nursing unit to use as swing space while other units were renovated on the campus.
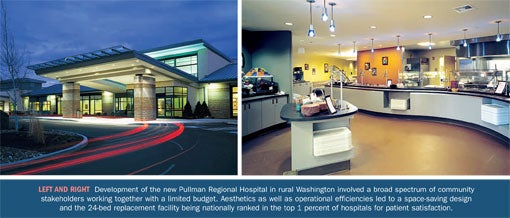
At Pullman Regional Hospital in the small agricultural and university town of Pullman, Wash., a new approach was needed following an aborted effort by a previous architectural firm that left the institution facing an impossible budget to replace its critical access facility.
A new firm was retained and the team brought a cost-appropriate solution to the leadership team within six weeks' time. The project required buy-in from a range of community constituents including the public hospital district's board of commissioners. There were many bases for the project team to cover, given the high local interest in developing a state-of-the-art health care facility on a limited budget.
Since the project was completed a few years ago, it has been ranked in the top 1 percent of hospitals nationally for patient satisfaction, according to Press Ganey Associates, South Bend, Ind.
Lowering operating costs
Given that operating costs for a health care facility run three times the capital cost over the life of the building, much attention needs to be given at the outset about ways to keep them in check.
Thinking through options to minimize infrastructure costs is always a design team's key challenge. The U.S. Green Building Council's Leadership in Energy and Environmental Design (LEED) certification, the Center for Maximum Potential Building Systems' and Health Care Without Harm's Green Guide for Health Care and other sustainable building systems are tied to this concept, offering the credentials and third-party endorsements that authenticate what's been achieved. And "green" building principles can be very helpful in guiding the process to achieve efficiencies in terms of both cost and sustainable development.
Beyond LEED and other green systems, health facilities professionals also can look at cost-benefit life-cycle strategies, utility rebates and other strategies to achieve real operational savings.
Many hospital developers have recently looked to Europe, especially Scandinavia, to see how facilities there are designed to cut operational costs. However, copying their techniques is problematic for U.S. builders. In Europe, for example, a window might be opened to warm or cool a room. In the United States, codes and construction techniques generally prevent such measures.
Swedish Medical Center's Issaquah hospital provides several workable examples in lowering projected operational costs. Building codes limited the facility designers' ability to devise a heating and ventilation system that could meet European hospitals' typical usage of 100,000 British thermal units (BTUs) per square foot per year. But, by installing enormous ducts and small fans that are less expensive to operate, the designers were able to increase the air volume while reducing the velocity of air.
Thus, the expected BTUs per square foot per year of a typical Pacific Northwest hospital of 265,000 was reduced to 150,000, saving significantly on operating costs in just this one area. In fact, the Issaquah facility overall is expected to use 43 percent less energy than other hospitals in the Puget Sound.
On the other hand, a "back to the future" approach was used in water management at the same new facility. Relying on a dependable well as an emergency water source eliminates the need for storage, reduces costs and helps the environment, as stored water does not need to be replaced to maintain its freshness.
Optimizing staff efficiency
Experts say that staffing represents up to 60 percent of all operational costs at a medical facility. Given the challenges to recruit and retain top staff, the health facility itself wears many hats in healing patients while providing a comfortable, efficient workplace for staff.
Architects are well-advised to create designs that optimize the most efficient work processes. These are, of course, the tenets of lean production, aimed at reducing waste in such areas as waiting times, inventory, unnecessary procedures and excessive motion. It's no surprise that project teams that have paid attention to these principles ended up with higher patient satisfaction.
One valuable approach to increasing efficiency in health care is process mapping. It involves a thorough outline of all the steps involved in a certain process and eliminating or redesigning redundant or unnecessary tasks. Once the process is mapped, the project team can create a layout, determining which spaces best go next to each other in support of the work processes, improving workflow.
A related means of optimizing staff efficiencies also can be found in service line design. It often involves grouping all the components of one service such as cardiology. An optimal design might recommend locating such functions as the cath lab, nuclear medicine and computed tomography scanner together, outside the traditional imaging department setting.
This concept can run against the traditional hospital organizational model of departments. But if a more decentralized solution will be more efficient, it will easily pay for the duplication of equipment.
A difficult challenge is to determine what services are best provided bedside or locally and which ones the patients must be moved to—no small decision in designing a large, urban medical center or even a small, rural facility.
In many instances, small, rural facilities face unique staffing issues. For example, at Morton General Hospital in Washington state, a critical access hospital, overnight nurse staffing levels typically included one registered nurse who had to monitor both patient rooms and emergency services. Placement of the nurses' station was crucial to maximizing sightlines and reducing unnecessary movement.
In another hospital where services were being centralized, a simple solution in the design of clinics and offices made clear sense: Put doctors' offices on the same floors as the base for the services they provide in the hospital, thus minimizing travel distance and optimizing time spent with patients.
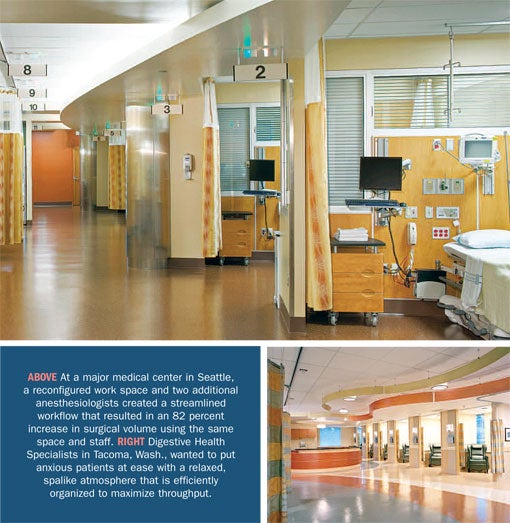
On a bigger scale, a large, urban medical center worked at renovating its outpatient surgery center. Streamlining workflows was an essential ingredient to holding staffing expense while improving throughput.
The changes required approval by state regulators as it did not meet the prescriptions of the code. But, with the addition of two anesthesiologists, the result has been an 82 percent increase in surgical volume, using approximately the same space and staff. Even with the burden of increased service volumes, staff and patient satisfaction in the unit are up. Most importantly, patient outcomes are superior.
Step back and look
Health facilities professionals committed to controlling the costs of capital, operations and staffing must step back and look at everything from both a narrow and wide perspective.
At the end of the day in most every case, processes and systems in a complex environment such as a hospital can be streamlined, saving money and improving the healing environment.
Phil Giuntoli is a principal who heads the health care practice at CollinsWoerman in Seattle. He can be contacted via his e-mail address at pgiuntoli@collinswoerman.com.
| Sidebar - Tips for architects working with hospitals |
| Architects would do well to listen to those most attentive to their ideas and approaches in designing health care facilities—their clients. Following are some tips for architects from veteran hospital executives: Involve the customer. Most health care organizations insist that architects remember that the customer is not the CEO, but the patient. Find ways to solicit patient input through patient committees, focus groups or advocates. Introduce new ideas. Building designers should challenge client thinking and bring to the table the best solutions from around the region, nation and world. Analyze the issues. Visit similar projects to see what's worked and what hasn't worked. Don't be afraid of some "re-dos" along the way to ensure the project comes out right. The flip side of this, however, is to carefully attend to project expenses by getting it right throughout. Remember who's responsible. All parties must work closely and frequently in person so that everyone involved agrees on the functionality, costs and other project dynamics. Hospital leadership must bring various internal constituencies to the table, build consensus and keep everyone aimed in the right direction. Finally, remember that form follows function. The optimal environment is one where the architects feel empowered to bring their best design, creative abilities and professional problem-solving to the fore. |
| Sidebar - Tips for hospitals working with architects |
| Designing health care facilities is a complex process and not one that can be done in isolation. Following are some tips to help health care organizations get the most out of their relationships with their architects: Bring the architect in early. Even if the health care organization has not fully committed to a new building project, experienced architects can help sort through the key initial considerations that will set the ideas on firm footing. Make the architect a part of the team. Deep organizational knowledge better equips an architect to design health care facilities that reflect the provider's values, goals and brand. Confidentiality is a byword in the architectural profession, so organizations should not be reticent to treat the architect as a trusted partner. Establish clear expectations. This is true for all elements of the project. Defining the ideal solution from the start enables the architectural team to aim high, then adjust and problem-solve Collaborate regularly. Once a project is under way, the working relationship needs to remain close, integrated and frank. Frequent in-person meetings and collective problem-solving almost always return a more satisfying project. Experience dictates that working more proactively with an architect can help health care organizations harness the architect's perspective and energy to get the most out of new and redesigned facilities. |




