Technology for today
 To support hospitals as they move into a completely paperless environment with digital record keeping, remote access of patient information, bedside patient charting and integrated operating rooms, the data center has become the critical tool in communications. But, as the use of high-tech equipment expands, so must the data center.
To support hospitals as they move into a completely paperless environment with digital record keeping, remote access of patient information, bedside patient charting and integrated operating rooms, the data center has become the critical tool in communications. But, as the use of high-tech equipment expands, so must the data center.
Creating a proper master plan that fulfills a hospital's goals with the right systems and equipment is critical to the effectiveness of the data center's operations.
A well-planned data center goes beyond current needs with its scalability, the capability of being easily expanded or upgraded on demand. Considering that the average life of a piece of electronics equipment is four years--and new equipment often has faster processors requiring more power and cooling--it's easy to see the necessity of future flexibility.
Assessing the mission
Understanding scalability is a large part of planning a better hospital data center. Equally important is realizing the result of the ubiquitous use of technology. A business need is revealed, which leads to a technological response, which identifies a new need, and so on; we've established a continuum of increasing reliance on technology resulting in mission creep.
Solving this problem begins with the hospital's business mission validation. What are the current and proposed business missions supported by the data center? In most cases, a single data center is required to support multiple business missions, with their own unique requirements and associated impact on systems. Understanding and validating the business mission will enable a design professional to evaluate systems that can be deployed to support the mission. What level of reliability does the hospital need now and what tier are they going to need?
Determining the concept
 |
| Health care data centers serve as a critical communications tool, linking hospitals, staff, patients and insurance companies. Photo by Dave Whitcomb/RTKL |
Data center design is a balancing act between future flexibility, minimizing costs and maximizing reliability. Accurately judging the level of reliability required is integral to planning, especially because patients' well being, not just information, are depending on data centers.
Reliability is usually expressed with "N" equaling need--the quantity of components necessary to support the mission. An everyday example to illustrate this terminology is the tires on a car. It needs four tires, but with the spare tire there are five. Therefore, a car's tires can be referred to as N+1. If a driver has a second car in case all the tires blow out at the same time, the system is 2N. And if both cars have spare tires, it's 2(N+1).
The Uptime Institute (www.uptimeinstitute.org) translates these concepts into a tier rating system for data centers. Tier I has no redundancy--it's just N. Tier II adds N+1 components for the uninterruptible power supply (UPS), generators and mechanical systems. With Tier III, although only redundant component is active at any given time, there is dual-corded (two power cords) electronic equipment connected to two separate UPS systems, two emergency generator sources and two paths for chilled water. Finally, a Tier IV data center has two completely separate systems, each with N+1 redundancy.
With clinical computing systems, hospitals almost always automatically need a Tier III or IV facility. For many, a "dual active" approach--two mirrored, active servers separated from each other and supported by a slightly less redundant infrastructure--may be most effective. This approach can provide more reliability to the end user at a lower price point, because the cost of redundancy grows exponentially as the tier ratings rise. Using this concept, hospitals may also be able to use an old data center as a second active backup site to support the most critical applications.
Programming the space
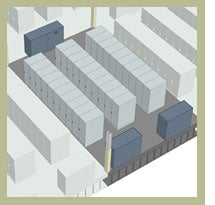
 |
| Compartmentalization of critical communications equipment can help maintain a high level of security by limiting human contact. Diagram by RTKL |
Examining how a hospital is using its current facilities and equipment can help determine future growth needs for servers, networking and storage, as well as provide an estimate of the expected cooling load and power requirements. Through programming, system needs are reviewed and addressed in a series of interactive work sessions with the data center user and facilities staff. Next, the design team can do space test-fits and develop systems options that support the program and business mission. This is where scalability comes in. Understanding current and future needs, and also understanding how mechanical and electrical systems can be designed with growth in mind allows for better cost control.
An example of one of the programming decisions affecting data center design and performance is the level of separation and compartmentalization. Central to data center security is the limitation of user contact with the critical communications equipment, since human error is the cause of most data center failures. Many hospitals choose a departmental server compartment concept to help keep less-qualified people who still need equipment access off the main floor.
Showing intent
Each system choice will generate certain ideal dimensions and limits within the data center. For instance, if a computer room air conditioning (CRAC) unit is selected, it is important to know that a CRAC can only push cold air 40 feet under the raised access floor. Therefore, once systems and space options are selected, the basis of design can be established. This process documents the systems and design intent--a critical step in explaining to third parties why certain decisions were made.
The culmination is a schematic design called a "C-level" report--a document that the hospital's CEO, CFO and CIO can review in order to understand how the team arrived at its recommendations and why the plan needs to be implemented.
Applying the process
This whole process proves successful in meeting the needs of health care corporations.
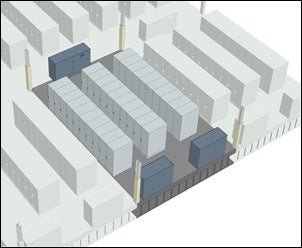
 |
| A 10-year plan clearly dictated future requirements at Johns Hopkins Hospital in Baltimore. Photo by Dave Whitcomb/RTKL |
Baltimore-based Johns Hopkins Hospital's information systems were expanding from insurance processing and accounting to include picture archiving and communications systems (PACS), digital pharmacy and digital communications. The solution based on the business mission validation determined a one- and three-year need for a Tier III facility, and a five- and 10-year need for a Tier IV facility.
The programming phase revealed that in addition to the need for more reliability, there would be a four-fold increase in anticipated power and cooling requirements over the 10-year business plan. With a scalable solution, Johns Hopkins Hospital immediately needed a Tier III data center to support 100 cabinets at two kilowatts (KW) per cabinet, and a Tier IV data center with double the capabilities in 2015. The mechanical and electrical solution met the immediate requirements, but is expandable, without an outage, to accommodate the future needs.
Under the direction of Mary Hayes, Johns Hopkins Hospital director of data center services, the emphasis was on viewing data center requirements from a business mission perspective. This allowed the team to focus the design on critical elements over the lifetime of the facility and avoid costly and unneeded data center capabilities on day one. In addition, significant future retrofit expenses were eliminated by including components that allow for a cost-effective future expansion.
A link to the future
Today, a lot is riding on the performance of hospital data centers. Not only do they have to balance size and power usage, but they also have to maintain reliability in order to keep hospitals functioning properly.
The budget is critical and choices will drive how effectively a hospital operates and communicates. Those that position themselves securely will be able to succeed both financially and clinically, ensuring that the data center will effectively link hospital staff, patients and insurance companies well into the future.
R. Stephen Spinazzola, P.E., LEED AP, is the vice president in charge of the Applied Technology Group at RTKL. He can be contacted at sspinazzola@rtkl.com.




