Eight best practices
 Virtually all health care facilities managers understand that their hospitals benefit significantly from high-performance energy management and control systems, many of which require advanced technological features.
Virtually all health care facilities managers understand that their hospitals benefit significantly from high-performance energy management and control systems, many of which require advanced technological features.
Of equal importance are the mechanical-electrical systems controlled by the energy management and control systems. An effective energy management program occurs when both mechanical-electrical systems and their controls are managed in a complementary manner as a single system.
Often, energy efficiency measures become the glue that combines energy management and control systems with mechanical-electrical systems to achieve successful financial outcomes related to an energy management program.
Energy efficiency makes sense on multiple levels, not the least of which is that health care facilities are big energy consumers. The Energy Information Administration’s most recently completed Commercial Building Energy Consumption Survey showed that large hospitals — defined as those at least 200,000 square feet in size — accounted for two percent of the country’s commercial floor space, yet consumed 4.3 percent of the total delivered energy used by the commercial sector.
Facility managers know that significant savings can be achieved through investments in better air-handling systems, improved meter and monitoring systems, lighting modifications, variable-frequency drive (VFD) motor controls, demand-side management techniques, high-efficiency chillers and a variety of measures enumerated in the U.S. Green Building Council’s Leadership in Energy and Environmental Design criteria and standards.
But managers also need to remember that top management executives make decisions to invest in these improvements because someone has made a persuasive business case in support of the expenditure, not because someone has made a persuasive technology case to invest.
Best practices
So, what do facility managers need to do to get their investment proposals over the goal line? Here are eight best practices managers should adopt when developing a business case for investing in a comprehensive energy strategy:
1. Create a concise, well-constructed proposal that zeroes in on the plan’s attractive return on investment and does not focus excessively on the proposal’s technological attributes.
As technology-intensive facilities that operate around the clock, hospitals and other health care facilities tend to consume twice as much energy as typical office buildings.
The Environmental Protection Agency (EPA) says that health care organizations spend nearly $8.8 billion (in 2008 dollars) on energy each year to meet patient needs. Every dollar a health care organization saves on energy has the equivalent impact on the operating margin as increasing revenues by $20 for hospitals or $10 for medical offices.
Industry analysts have also found that health care organizations that implement aggressive energy efficiency measures can outperform competitors by as much as 10 percent in net operating income.
To effectively convey the bottom-line benefits, engineering and operations professionals should thus present a clear, concise business case for their recommended investments by using data-base graphics in their presentations. This helps decision-makers make quantitative comparisons among upgrade options.
In addition to including a section that identifies funding sources for the investment, it is essential to devise a cost-benefit analysis that quantifies the payoff on the investment. The analysis needs to take into account a calculation of the payback period, as well as other variables.
Presentations also need to be kept short and to the point. They often represent just one item on a full, executive committee agenda. If facility engineers squander too much of their limited time extolling the technical virtues of an energy investment, they may see lose the attention of their audience of institutional decision-makers.
 |
|---|
| Elena Ress, an engineer with ConEdison Solutions, on the roof of Largo (Fla.) Medical Center, where the company provided energy services. |
2. Explain that the investment will reduce owner risk.
In every health care setting, applying the principles of effective energy management can and will have a positive impact on reducing risk to clients and staff. The deployment of sophisticated and efficient equipment promotes the safety of patients, personnel and visitors. In addition, aging facility infrastructure, strained patient-care units, underperforming building systems and other operational gaps help run the risk of non-compliance with environmental and public safety mandates.
Inadequate lighting will diminish the institution’s capability to perform any range of medical functions. And people can trip and fall. Poor ventilation can impact the spread of disease. With proper air flow and efficient filtration, ventilation performance can be improved dramatically, thus reducing risk to a hospital. Effective and modern HVAC systems to control temperature and humidity reduce negative impacts on processes and procedures that require consistent temperature and controlled humidity levels. And the availability of reliable, back-up generation to preserve operations can take on a life-and-death urgency.
3. Demonstrate how an upgraded energy management system enhances the healing environment and improves the comfort of patients and other occupants.
Proper energy management has a positive effect on the performance of medical procedures and helps support the health and safety of patients and hospital personnel.
VFD controls, for example, enhance the patient environment by reducing temperature fluctuation, thus improving patient comfort.
Good lighting aids in diagnosis and treatment throughout the medical facility. Overall poor quality of lighting creates an environment that is neither optimally efficient nor beneficial to the operation of the hospital or the performance of its employees.
Humidity and temperature levels can be impacted by building management systems. If these systems operate correctly, humidity and temperature will be maintained at a safe level that encourages good internal air quality (IAQ).
Correct building pressurization and air filtration also support the healing environment and enhance safety. Properly controlled and operating HVAC and control systems protect building occupants and equipment from exposure to unwanted germs, dust, dirt and other concerns associated with effective infectious control and poor IAQ.
In one instance, a large hospital overcame a 20-year-old issue with temperature and humidity control in an operating room, which had persisted despite repeated attempts to solve it. The answer involved a novel energy recovery solution that also allowed the central energy plant to operate significantly more efficiently.
In another case in Florida, a vendor team overcame a significant patient and occupant comfort problem with a solution that also saved energy through improved central plant primary pumping and controls. The solution effectively addressed substantial air-handling distribution and control issues.
4. Where possible, cite independent sources or bring in outside experts who can provide guidance and data that demonstrate the financial benefits of the investment.
Both government and private sources offer facility managers tools that will add financial meat to the bones of a technology-oriented pitch. Personnel from the EPA's Energy Star Partner program — institutionally eager to help facilities meet Energy Star standards — can provide guidance and data. Moreover, once a project earns the Energy Star ranking, the institution instantly improves future access to private and public financial assistance.
On the private side, health facilities commonly tap the services of a qualified energy services company (ESCO) to devise major energy investment initiatives. ESCOs are expert at calculating the financial payoff of these projects.
Plus, as more of these projects are undertaken on a energy-savings performance contract basis, ESCOs are not just calculating or projecting the energy payoff, they are guaranteeing the payoff. Such guarantees obviously appeal to financial decision-makers.
5. Before preparing a presentation, meet with a top institutional financial executive to identify and assess prospective sources of financing.
Prior to a presentation, it is essential to do some smart institutional homework by meeting with one or more of the institution’s top financial officers. This is important for two reasons.
First, the finance officer will help facility managers understand the current institutional mindset with respect to capital spending. What sort of benchmark payback period is usually targeted? What kind of cost-benefit impacts have been tolerated by the health center when prior, similar investments were approved? What other established investment criteria exist, such as discount rates or other factors?
Second, the financial executive will understand internal funding possibilities. He or she will explain how the facility normally covers the cost of energy-related and other capital expenses. Institutions may have funds set aside, for example, for infrastructure investments, or dedicated budget lines for equipment purchases.
The financial officer — having hands-on experience with the health care center’s investors and lenders — will also be helpful in surveying the landscape of external funding possibilities. If a project involves an energy savings performance contract, both the in-house financial executive and the cooperating ESCO can help identify the most cost-effective way to underwrite the initiative.
6. Research past energy usage and spending and project future usage and spending.
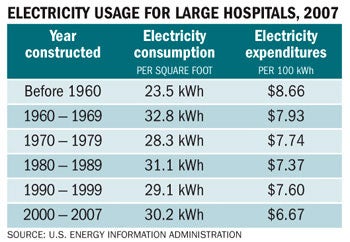 |
|---|
| The most-recently available data from the Energy Information Administration shows that per-square-foot electricity consumption in hospitals larger than 200,000 square feet has generally been trending downward in newer facilities since the 1960s. |
To help ensure a credible presentation, managers need to build a business case that takes into account both the history of past energy usage and projections of future usage and future fuel costs.
While records of prior energy spending should be relatively easily to obtain, factoring in future spending patterns will require that the facility manager incorporate a sensitivity analysis into the presentation. This clearly demonstrates that the overall cost-benefit analysis has taken into account such uncertainties as future changes in energy prices.
Even if fuel costs are projected to decline, a robust proposal can persuasively show that the investment is still worth making by including all components that go into energy and operating costs.
The presentation should also incorporate a forthright analysis of the costs and benefits associated with any prior energy investments made by the health care facility.
7. Use language that corporate executives understand: speak in terms of dollars and risks, and focus on the investment’s contribution to the institution’s financial viability and long-term financial strength.
Commonly, facility management professionals and corporate management simply speak in two separate languages — and use different jargon — when they think about their respective work responsibilities. While the facility engineer focuses primarily on technology, maintenance and performance, a senior level hospital manager instead emphasizes financial factors and the impact of an investment on the institution’s bottom line.
As emphasized above, facility managers aiming to persuade institutional management to make a large engineering-related investment must be able to frame their proposals in an economic and budgetary context. Already conversant in tech-speak, the manager also needs to come across as conversant in finance-speak.
In the midst of a presentation, the facility manager cannot afford to be caught flat-footed by questions from the board about budgetary considerations such as discount rates, net present value and internal rate of return. Know what these terms mean and be ready to comfortably incorporate them into the pitch.
8. Show how the plan promotes compliance with regulatory requirements.
Among the most important components of effective and environmentally appropriate facility operation in the health care industry is the accreditation that results from the Joint Commission.
One of the critical elements of accreditation is the environment of care, which incorporates all of the comfort and safety issues that are affected by — and enhanced by — energy management and the efficient operation of energy equipment.
Moreover, all hospitals must have a reliable and redundant back-up system to keep the energy flowing. These requirements usually call for redundancy levels ranging from 30 to 50 percent. A sophisticated energy management system facilitates demand shifts that save money and enhance redundancy.
A competitive environment
Especially in today’s environment of shrinking reimbursements, an energy manager’s budget request needs to compete against many other highly compelling alternatives, such as staff recruitment, salaries and benefits, investment in new and sophisticated medical equipment, insurance and other such costs.
For an engineer to effectively persuade a financial manager of the need to make a major energy management investment, the case needs to be framed in terms of the expense’s investment value, and not simply in terms of its technical merits.
To win approval, energy management proposals can and must clearly make sound financial sense and show long-term, business value.
Andre’ LeBlanc is director of operations at ConEdison Solutions, Valhalla, N.Y. He can be reached at LeBlancA@conedsolutions.com.




