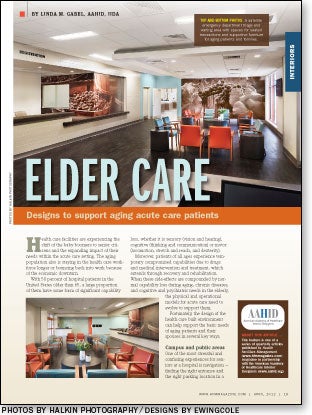
Elder care
 Health care facilities are experiencing the shift of the baby boomers to senior citizens and the expanding impact of their needs within the acute care setting. The aging population also is staying in the health care workforce longer or bouncing back into work because of the economic downturn.
Health care facilities are experiencing the shift of the baby boomers to senior citizens and the expanding impact of their needs within the acute care setting. The aging population also is staying in the health care workforce longer or bouncing back into work because of the economic downturn.
With 50 percent of hospital patients in the United States older than 65, a large proportion of them have some form of significant capability loss, whether it is sensory (vision and hearing), cognitive (thinking and communication) or motor (locomotion, stretch and reach, and dexterity).
Moreover, patients of all ages experience temporary compromised capabilities due to drugs and medical intervention and treatment, which extends through recovery and rehabilitation. When these side-effects are compounded by normal capability loss during aging, chronic diseases, and cognitive and psychiatric needs in the elderly, the physical and operational models for acute care need to evolve to support them.
Fortunately, the design of the health care built environment can help support the basic needs of aging patients and their spouses in several key ways.
Campus and public areas
One of the most stressful and confusing experiences for seniors at a hospital is navigation — finding the right entrance and the right parking location in a large health care campus setting, and wayfinding throughout the building itself once they are inside. To help ease this experience, designers should factor in the following considerations:
Exterior wayfinding. Many hospitals have created beautiful landscaping that unintentionally blocks visual access to key directional signage. It is critical to make sure that the view to signage is clear for both vehicles and pedestrians, and labeled with simple terms that are familiar and recognizable to the community at large. Pavilions named after donors may have great marketing appeal, but mean nothing to an elderly woman who is trying to find the emergency department (ED) or an outpatient center elsewhere on campus.
Designers should focus on the major hospital entrances that seniors use most — emergency walk-in, main entry and outpatient services. These entrances need to be distinct from each other, with convenient, designated parking that is obvious and visible in connection with the destination. Valet parking helps to alleviate the stress of parking and finding the way into the right building entrance, but many seniors under duress or with age-related mental issues do not feel comfortable handing over their keys to a stranger in times of crisis.
Interior wayfinding. Hospitals typically are designed to simplify wayfinding with long perimeter or central corridors connecting users to and from key destinations.
Oval-shaped hand and lean rails and resting points located along the path every 50 feet give support for both the physical and critical cognitive functions that may be diminished due to stress and anxiety.
Aging eyes need increased contrast in value between the floor and walls and indirect ambient lighting to reduce glare on transaction counters, floors and signs. Creating unique landmarks along corridors that combine art, color and short-term seating help imprint a memory of the path beyond just signage.
Exterior windows along main corridors provide access to daylight and time of day. However, direct sunlight creates glare and visually disturbing patterns on the floors and walls at certain times of the day for users with cataracts and mild dementia. Consequently, the daylight must be filtered appropriately with window shades. Many shade cloths are available to cut heat and glare, yet maintain views to the outside.
Destinations should be obvious as arrival points along paths through the use of changes in lighting, flooring and wall color and design. Clear views to identification signage and low reception desks that provide direct eye contact with a staff person also should be used.
The typically high transaction ledge with a lower area off to the side helps staff members conceal computers and paperwork and still meet universal accessibility guidelines, but it does not address the cognitive needs of seniors to easily identify and confirm with a person that they have reached the correct destination.
Consistently used bold colors; high-contrast, larger-sized and simplified font styles; and appropriate nonglare lighting make it easier for older eyes to read signs. Because the average resting line of sight lowers as people age, placing interior directional and destination signs at a lower height enhances the ability of seniors to identify and read signs.
Off-limit spaces. To keep the elderly on the right path, nonpublic corridors should be designed differently to deter them from taking a wrong turn. These choices can be disguised easily by painting staff entry doors and frames to blend in with the walls, and using different types and levels of lighting to help reinforce correct choices of paths and doors.

Emergency department
Going to the ED is a stressful and anxiety-producing experience for anyone, but particularly for the elderly, whose coping skills are compromised by age-related mental issues or traumatic events that brought them and their loved ones to the hospital. However, the ED experience can be eased greatly for seniors by introducing the following design cues:
Triage spaces. Most walk-in triage and waiting areas are designed with hard, sound-reflective surfaces, glaring overhead lights and large, open waiting areas with televisions to accommodate as many persons as possible within view of staff.
This environment can be extremely agitating to a person with vision and hearing loss, lack of balance, incontinence, cognitive decline and dementia. Hospitals now are training triage staff to quickly identify seniors who are displaying agitation or anxiety and work with patient advocates to transition them to quieter, smaller-scale waiting areas or private rooms to help restore a sense of calm.
To help reduce anxiety, triage desks can be modified with quieter, sit-down areas off to the side. The addition of sound-absorbing walls and ceiling materials, indirect lighting and smaller family-sized waiting area clusters within larger waiting areas will help to reduce negative environmental stimuli. These design changes, teamed with a fast-track model to move patients quickly into a private triage or exam room for bedside registration, will help provide a calming, supportive environment for the patient and family.
Private areas. Open bay cubicles are disorienting to elderly patients and their spouses — loud monitor alarms, overhead paging, other patients' distress, caregiver dialogue about other patients and observing care of others can increase their level of anxiety exponentially and may prompt flight or violence as a response to sensory overload. Elderly patients and their spouses with cognitive decline need both visual and acoustic personal space of a private room to calm fears and anxiety, reducing the need for medication or physical restraint during examination and treatment.
Toilet rooms. Many elderly patients and their spouses arrive with urinary tract infections or incontinence. Both conditions can bring on mental confusion and distress as well as trigger frequent visits to the toilet room. Locating senior-friendly exam rooms directly adjacent to toilet rooms or included as an en suite can help decrease anxiety for seniors and the confusion of wandering the ED in search of their rooms. Siting elderly supportive rooms near nurses' stations helps reduce anxiety of elderly spouses and enhances monitoring of wandering or distressed patients.
Inpatient units
Once an elderly patient and his or her spouse has passed the parking lot and main entry space or entered through the ED, he or she still must function comfortably in the inpatient unit. The following strategies can help in this mission:
On the unit. Elderly patients and their spouses both need visual connections to staff and distinct paths, boundaries and destinations to follow. Along these paths, ample use of handrails on both sides of unit corridors also is recommended.
As hospitals are starting to address the mental health needs in an integrated approach, a decentralized care model seems to work best for patients and their spouses with cognitive issues, so their fears of being lost or disconnected are reduced, and staff has a direct connection and home base nearby.
Such Planetree elements as patient-friendly care team stations, family-sized gathering spots, and quiet reading and computer areas in the unit are highly desirable, especially in semiprivate units. Similarly, loud overhead paging systems or nurse call systems should be avoided.
Large areas can be overwhelming to the elderly in unfamiliar surroundings. Many hospitals are providing easy access from inpatient units to small-scale family kitchens or cafes and safe, enclosed gardens for access to fresh air and daylight.
Private rooms. Aging patients may arrive with reduced agility, upper body strength, eyesight and hearing. They even may be suffering from dementia not readily apparent or flagged as a condition. Medical treatment, narcotics and lack of sleep or water can exacerbate their ability to understand what is happening. In extreme cases, they can become agitated, pulling lines out, striking out at caregivers or trying to flee.
Private rooms afford space for the spouse or family member to stay bedside 24/7, enhancing a patient's ability to cope with unfamiliar surroundings and routines. Rooms should provide space for the patient's and family members' independent functioning and mobility equipment and adequate clearances for patient handling equipment. Thermostat controls and light switches should be accessible from a standing or sitting position.
Patient room surfaces need to be easily cleanable to help prevent infections. Flooring also should be slip-resistant to help prevent falls. Eliminating transition strips at doorways between the toilet room and sleeping area and between the patient room and corridor helps to prevent trip and fall incidents for patients and spouses who shuffle when they walk.
Likewise, lever-style door hardware that does not require a grip or twisting action and surface-mounted doors that won't swing into the walking path of the user also are recommended. Contrasts between the walls and handrails enable visually impaired patients to identify and use them properly.
Patient room family zones need to be directly adjacent to the bedside, not at the sidewall or footwall only. For elderly spouses, a simple sleep sofa is safer and less confusing to get in and out of than a sleep recliner, and affords more flexibility in visitor seating. Patient support chairs and guest seating at the bedside should have arms and hand-grip extensions for proper support in and out of sitting and standing positions.
Amber light-emitting diode (LED) night-lights to support diurnal sleep cycles in the patient room, integrated into the handrails or as footlights, provide a safe visible passage to and from the toilet room. Similar night-lights should be incorporated into either the handrail next to the commode or as an LED wall fixture mounted between the commode and vanity to reduce sway velocity in sit-to-stand motion.
Beds with motion alarms linked to caregiver communication devices help care-givers know when at-risk patients are out of bed. Taken further, one long-term care facility recently was fitted with motion-controlled, linear amber LED fixtures around the bathroom doorway and inside the bathroom, providing patients and spouses with safe visible passage to and from the toilet room at night.
Bathrooms. Handrails in patient rooms that lead a patient to the bathroom also help patients navigate their way safely from the bed to the toilet and back.
Within bathrooms, clear floor areas on either side of the toilet for caregiver support help prevent patient falls and also support the needs of bariatric patients. Showers also should have clear areas for staff on both sides of a patient. Contrasting colors on the walls and floors compared with those of grab bars, toilets and sinks help seniors see and grasp support and plumbing fixtures easily.
Toilet and bathrooms should be brightly illuminated with wet location downlights in the shower and in the commode areas. Vanities should be illuminated with a decorative wall light mounted over the mirror, utilizing linear or compact fluorescent lamps of 3000 Kelvins and an 82 color rendering index.
A multidisciplinary future
The needs of elderly patients and their spouses in the acute care setting require a multidisciplinary approach that goes far beyond design issues.
In fact, some facilities are creating Acute Care for Elders (ACE) teams that partner geriatricians, clinical and nurse specialists, social workers and administrators to craft operational guidelines and staff education programs to evolve the culture of care for elderly patients.
Once this care model is fully developed, a design team can work with an ACE team to improve the built environment to ease wayfinding; provide familiar and easily understood safe surroundings; decrease confusion, anxiety and length of stay; prevent injuries and infections; and promote independence and well-being of the patient and family toward a smooth transition to home or post-acute care.
Such a multidisciplinary approach can improve the acute care environment for the aging population as well as for all patients, families and caregivers.
— Linda M. Gabel, AAHID, IIDA, is director of design for Mosaic Design Studio, Columbus, Ohio. She can be reached atlgabel@mosaicdesignstudio.com.
| Sidebar - Checklist of design elements |
| Efforts to upgrade acute care spaces to accommodate the growing ranks of elderly patients include a variety of interior elements that promote safety as well as alleviate fear and confusion. The following checklist summarizes those discussed in the article: Floor plan and furnishings
Hardware and controls
Lighting and color
|




