Building information modeling plays bigger role in space management
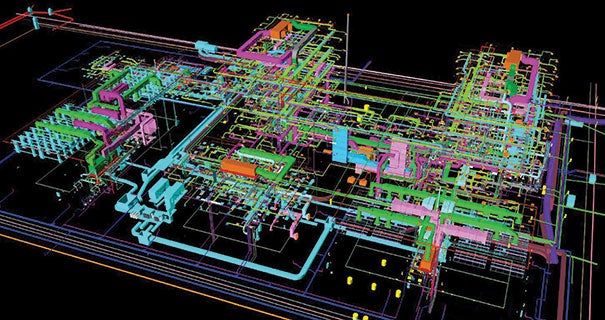 |
| IMAGE COURTESY OF VIEW BY VIEW A BIM-generated mechanical-electrical-plumbing design model preloaded with maintenance data can assist with infrastructure life-cycle management. |
Unless you’re one of the fortunate exceptions, the days of doing more with fewer staff is a permanent way of life for hospital facility departments in light of the Affordable Care Act (ACA) and potential reductions in reimbursements.
To make it more complicated, facilities directors must keep multiple and varied systems running smoothly in buildings that are aging and often on the same campus as new or renovated facilities. Mergers and acquisitions add more facility and building systems to the mix, making operations and management even more complicated.
While design and construction of new hospitals usually get the fanfare, the cost of these buildings pales in comparison to that spent on operations, maintenance and management, which may run up to 85 percent of a building’s total life-cycle costs, according to a report by leading design and construction software maker Autodesk, San Rafael, Calif.
There are additional challenges. According to a report by the National Institute of Standards and Technology, all U.S. commercial buildings waste an estimated 23 cents per square foot in life-cycle costs due to inadequate interoperability of data starting with the design and construction phase of a project through occupancy.
While no panacea, the latest building software and analytics programs can help to control costs and help buildings to run more efficiently by providing useful, streamlined data to facilities staff. Mobile devices and the instant accessibility to equipment information and work order adjustments can contribute to operational efficiency.
Benchmarking has emerged as a useful analytics tool as health care operations focus on improving the patient experience and community health, and lowering the cost of care, says Todd Wilkening, director of facilities, Ridgeview Medical Center, Waconia, Minn.
Benchmarking 3.0: Performance Criteria for Health Care Facility Managers, which is offered by the Health Care Institute (HCI), a partner of the International Facility Management Association, Houston, can help to determine the link between facilities operations and patient care costs, an emerging trend, Wilkening says.
“The greatest area for improvement is to help facilities managers understand the cost of business at a micro level,” he says. “We’ve done a good job over the years of finding the cost to operate the total building, whether it’s measuring by full-time equivalent or by square footage.
“But, now we’re looking in terms of the output of patient care. It’s opening our eyes to processes related to patient care and how we can understand more opportunities that affect care in a positive way. This has led to discoveries of hidden opportunities related to how the efficient use of assets can improve patient care,” Wilkening says.
HCI’s Benchmarking 3.0 delivers Web-based data reports in real time as well as executive summary reports, so facility managers can effectively communicate important operations and management data to health care leadership, Wilkening says.
The program also generates real-time automated dashboards and compares performance criteria internally or against other similar facilities, in addition to a multitude of other operations information.
Benefits of BIM
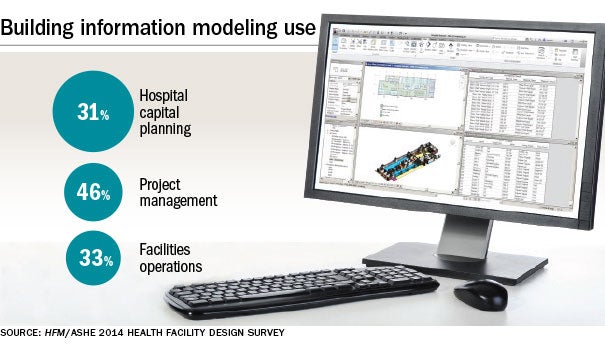
While building information modeling (BIM) typically is known for its time and cost benefits for new design and construction projects, it also is starting to play an important role in building management and operations for new and existing facilities and their space management.
Chuck Mies, business development manager, health care and education, Autodesk, says BIM is valuable for calculating square footage precisely and in half the time of other methods. The information is critical for determining Medicare and Medicaid reimbursements and the department’s rightful share of those funds, he says.
“The initial entry point for BIM for existing facilities is space management,” he says. “It’s a very simple low-fidelity model — doors, walls, windows, floors, ceilings — the architectural envelope at a level of sophistication just enough to calculate square footage.”
A white paper from Autodesk titled “Using BIM for Space Chargebacks in a Healthcare Facility” states that while the level of reimbursement related to facilities costs varies, it can amount to millions of dollars. Some hospitals reported that facilities account for as much as 20 percent of their total reimbursement.
Rich Mitrenga, business development manager, operations and maintenance, Autodesk, says BIM can be especially useful for management of hospitals designed with the software, because it is populated with data from the building model used for the design. BIM can then track, manage and control building systems ranging from mechanical equipment to door locks to lighting.
“That data then can be transferred to the systems that track, manage and control building systems and assets,” Mitrenga says.
Michael DeLacey, principal of design, engineering and operations technology consulting firm Microdesk, Nashua, N.H., is a proponent of BIM for its ability to cut through clutter generated at new project close outs.
While traditional close-outs can produce boxloads of shop drawings and other paperwork related to the job, BIM provides a virtual model with facility details that will help with future operations and maintenance. For existing hospitals, the ability to calculate square footage is an important benefit that can be built upon if renovations or additions are made.
Going mobile
Another key to operations efficiency is the ability to get maximum production from facility staff, and new technology continues to support this need. Bob Biggio, vice president of facilities and support services, Boston Medical Center, has used a mobile device app developed by Magic Software Enterprises that enables him to issue and update work orders while his techs are working on its expansive campus.
The app, which is an extension of the FMWorx work order system already in place, increases the efficiency of hospital technicians who may need to be reassigned to other tasks after they are in the field.
The app also streamlines the communication process so that requests for temperature changes in a patient room or department are routed directly to the facilities staff rather than to a control center that would then relay the call, Biggio says.
Wireless technology and the ability to monitor remotely such critical equipment as refrigerators, freezers and incubators used to store tissue samples or blood reflects a trend that is expected to grow, says Alex Shair, solutions manager of life sciences business, Siemens Industry Inc., Buffalo Grove, Ill. Wireless offers other benefits in addition to monitoring environmental parameters.
“Another advantage of a wireless solution is that when those pieces of equipment move around, you’re still able to monitor the temperatures,” he says. “People want to know the temperature in that refrigerator or freezer, but also where that asset is located.”
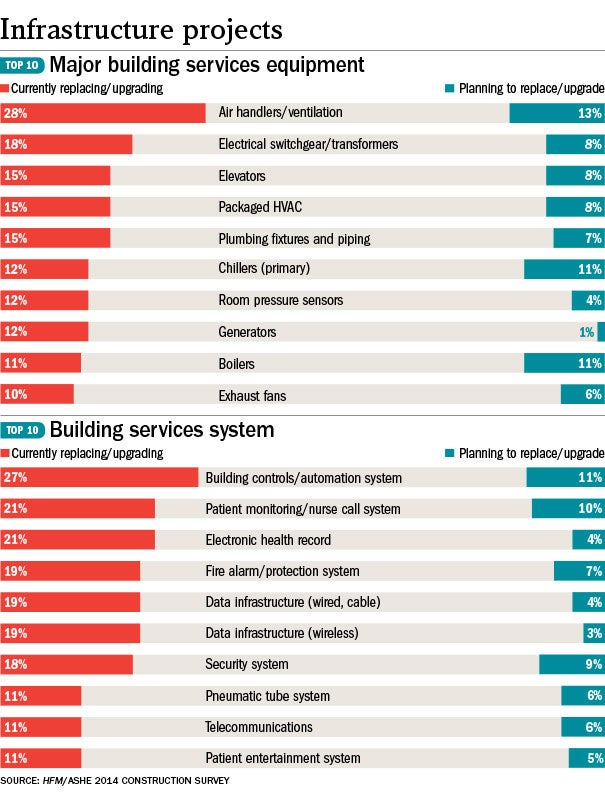
Aging infrastructure poses another difficult challenge as health care systems expand, renovate or merge with other organizations. The result is a mix of disparate systems ranging from the latest technology to those more than 30 years old, says James Winstead, director of health care and life sciences, Schneider Electric, Carrollton, Texas. Again, technology offers a solution.
“Cloud-based building analytics is a comprehensive statistical tool that can provide trending down to the device level,” Winstead says. “It will facilitate ongoing commissioning, continuous audits, fault detection to turn data into actionable information and simplify managing new and old systems together.”
Analytics increase staff efficiency by eliminating unnecessary scheduled maintenance and replace that with condition-based maintenance, he says.
“If you’re doing analytics at a level at which you’re trending the performance of individual devices, you can focus on when the equipment requires maintenance rather than reacting on a time-sensitive schedule,” he says.
A building analytics system that provides performance data from multiple systems and facilities requires a financial investment, but can be funded from operational efficiencies and staff efficiency while positively impacting patient satisfaction, Winstead says.
“Aggregating this data with analytics ultimately will help you make better decisions rather than speculate about what action to take,” he says. “If you make decisions around comfort, you’re going to impact patient satisfaction. And if you drive those scores up, you’re potentially going to impact reimbursement.”
Predictable problems
Tom Schiller, president and founder of AutomaTech Inc., Plymouth, Mass., partnered with GE Intelligent Platforms to develop a cloud-based, mobile-accessible building analytics program called FacilityConnex that delivers predictive maintenance information.
Continuous performance monitoring and related data produce a predictive maintenance strategy rather than a typical broken-and-fix or scheduled approach to the work, he says. It not only leads to more efficient use of facility staff, but also generates more comprehensive information about equipment performance.
“You may have an air handler where there is simultaneous heating and cooling going on. It’s a very difficult thing for somebody to recognize unless they’re looking at the trends as to how their equipment is running,” Schiller says.
“Our analytics perform a historical-based comparison and tell facility staff what is happening and give them an alarm notification,” he says.
Data can be helpful, but also create more work if they are not useful or there’s an overabundance, a common problem with some building automation systems, Biggio says.
Steve Dodd, commissioning advantage center of competency, Siemens Industry Inc., says his company is aware of that problem and has made it a priority to simplify information generated by its automation system.
“We’ve experienced, more than we can count, the number of times data were so immense facility managers couldn’t get their arms around them,” Dodd says. “We have developed standardized reporting that makes it understandable and for the key areas of facility operations.”
In assessing the future of operations efficiency, Biggio believes it’s more about optimal use of information and less about technology.
“It is about gathering data and using them in a way that is actionable by the facilities staff,” he says. “It also is about standardizing the type of data and the way data are collected in the facilities industry. Finally, it is about integrating systems so that you can realize the benefits and power of the first two.”
Once those are accomplished, hospitals and other health care facilities can gain further operational efficiencies, he believes. “The possibilities are really astounding.”
is senior editor of Health Facilities Management.