A new front door
About this articleThis feature is one of a series of quarterly articles published by Health Facilities Management magazine in partnership with the American College of Healthcare Architects. |
A hospital's emergency department (ED) often is referred to as the facility's "front door" because of the large number of patients who arrive through that department. But the challenges surrounding the ED have been well-documented, such as door-to-doctor time, extended length of stay, burden of uninsured patients who use the ED as a doctor's office, and the difficulty of accessibility from shifting population centers.
Regardless of location, statistics reveal that the need for emergency medical services will continue to grow. Recognizing the impact the ED has on the financial success of the hospital, would having more front doors improve the bottom line and help address problems that plague hospital-based EDs?
Freestanding emergency departments (FEDs) allied with major urban medical centers and health systems are dotting the landscape in many outer-ring suburban and rural suburban markets. Considering the growth of FEDs over the past several years, it is apparent that hospitals and health care systems are recognizing the benefits of FEDs to their portfolios and have a successful business plan to support this trend.
Defining the FED
An FED can be defined as a "stand-alone hospital specializing in emergency services" or a "provider-based department of the main hospital," which is the focus of this article. This distinction is important because of how each is viewed by the Centers for Medicare & Medicaid Services (CMS).
In simple terms, an FED functioning as a provider-based department is part of a health care system that is anchored by one or more acute care hospitals, and is distinguished from other emergency medical services such as retail-based clinics and urgent care centers because it offers all of the features of a hospital-based ED. Some of these features include 24/7 operation, imaging and laboratory services, and transport to an acute care hospital for patients who require admissions.
There are many variables when deciding where to locate an FED and how to integrate it within the surrounding community. When evaluating possible options, the design team must study:
- site selection — accessibility, visibility and expandability;
- collateral programs — additional programs that can be collocated with the FED to help amortize initial cost while creating a viable business model;
- community service — synergies within the community that support health care initiatives;
- pitfalls — potential obstacles.
Growth areas
FEDs have experienced increased growth in population areas such as outer-ring suburbs and rural settings. While each has occurred for different reasons, both require a unique, long-term strategy while providing access to emergency medical care. Some considerations include:
Outer-ring suburbs. As population growth occurs in outer-ring suburbs located off interstate highway loop systems, the increase in population can support the FED, which can become a feeder for the major urban medical center. In some cases, such as in Rust Belt cities, the growth of outer-ring suburbs has represented population shifts from urban and inner-ring suburbs. On the other hand, in high-growth areas such as Southern states, this can represent overall population growth.
The site should be in close proximity to interstate interchanges. The functions that occur at a freestanding ED are best suited to major retail and commercial centers. The site could be master-planned to accommodate incremental expansion, ultimately resulting in a comprehensive medical campus that would include acute care beds. Allowance for a helipad and consideration of the helicopter flight path, adjacent residential zones and emergency vehicle and service access also should be considered.
Primary care, specialty clinics and an ambulatory surgery center are programs that closely align with the same consumers who would use the FED. Laboratory and imaging departments required for FEDs also are used to support these functions, thus amortizing the cost and use of these core processes across more than one function. Other systems have developed alliances with health and wellness programs, such as those operated by the YMCA, leveraging the concept of a healthy lifestyle.
Many local governments have seen the advantage of developing services on a shared, regional approach. In the case of the FED, collaboration between the health care provider and the public safety departments of local communities encourages a synergy that supports the efforts of both. In an effort to have local health care services and emergency services, local and regional communities often will work to facilitate successful developments. In one project, a design team explored including a dispatch center that would serve several municipalities using the facility.
As with any developing area, available sites, site acquisition and improvement costs for upgrading greenfield sites can vary significantly depending on existing conditions. Careful evaluation of items such as zoning limitations, wetlands and environmental conditions should be part of early project analysis.
Rural settings. Unlike the outer-ring suburbs, rural areas and especially states that are sparsely populated or vast in scale suffer from a reduction in acute care hospitals, some of which closed due to inability to maintain a viable operational model. Site selection, collateral programs, community service and pitfalls should be evaluated on a case-by-case basis. In many instances, the role and function of the critical access hospital fulfills the need for emergency care.
Specific issues
In addition to location and integration issues, FEDs present a variety of more-specific facility programming and design issues. Some key ones include:
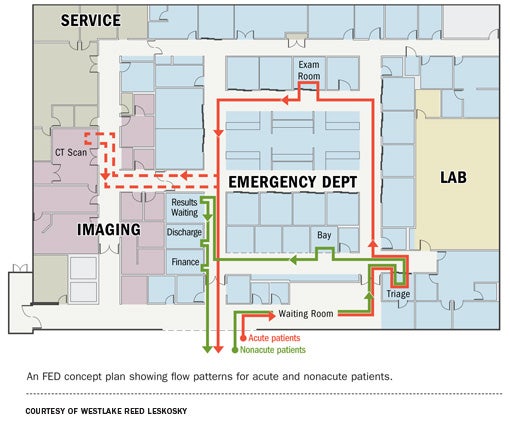
Emergency, imaging and lab program. The program for the FED should be based on projected visits per year. Historically, FEDs have a length of stay that ranges from 30 to 60 percent faster than the average for a hospital-based ED, which is slightly more than three hours. While these improved statistics may be affected by acuity of patient mix, an evaluation of the patient throughput process and an efficient design can help facilitate a reduction in length of stay.
Considering these assumptions, the number of exams rooms should be based on an average of 1,800 to 2,000 visits per year per room. Recognizing the increased volume of low-acuity patients, consolidating the reception-triage-evaluation area into a fast-track or split-flow configuration facilitates processing low-acuity patients. This can be designed in an open bay configuration.
In many cases, FEDs have between 12 and 16 exam rooms, open bays at 25 percent of the exam room total and a two-bay trauma room. For the exam room design, consideration should be given to a universal, same-handed room. A variation on this theme would be adjustments for bariatric, behavioral or sexual assault nurse examiner treatment rooms. Most EDs of this scale employ a racetrack configuration, with the nurse-physician-charting station in the center. It is crucial that the patient flow and exam room configuration take precedence when developing the layout.
Imaging should be directly accessible to the ED core and at minimum should include a standard radiology room, computed tomography room, ultrasound and related support functions. To maximize the use of the procedure rooms, the imaging space should include induction and patient preparation, changing, gowned subwaiting and patient toilet rooms. The laboratory space should be outfitted with adequate equipment and staffing to provide the necessary testing for the anticipated patient population and test type. With both imaging and lab, a minimum program is required to handle volume in the ranges noted, regardless of the number of exam rooms.
Core processes. Core processes and support functions such as office spaces, staff support and ED operations beyond the Facility Guidelines Institute's (FGI's) Guidelines for Design and Construction of Health Care Facilities requirements should be evaluated. Ingress and egress of materials, supplies and waste should be explored with the health care system to determine the impact on core processes such as respiratory therapy, environmental services and the lab, which may require additional storage space.
Depending on the frequency of deliveries, adequate loading dock, receiving and breakout space may be impacted as well as the storage of used linen, waste and red-bag waste.
Helicopter transport. The key issues to address with the helipad are location and function. The two options for locating the helicopter are the rooftop or the ground. If the helipad is used as a permanent parking space, and for refueling and servicing, it most likely will be ground-based. If this is the case, special provisions may be required pending local zoning requirements and specific project needs. If the helipad is rooftop-based, provisions for an elevator must be addressed in the design. In either case, the path of travel and transport requirements should be evaluated during the design phase.
EMS coordination. The health care system and design team should engage the public safety departments in all localities that will be served by the FED. Preferred access points and routes through the site, coordination of on-site security and local police, size and type of emergency vehicles and provisions for emergency medical services (EMS) personnel should be addressed.
Infrastructure. While minimum code requirements for mechanical, electrical and information technology (IT) systems are outlined in the FGI requirements, site-specific and owner-specific operational considerations should be explored early in the design process. Areas to examine include redundancy of systems, emergency power provisions and emergency preparedness plans.
Requirements can range from keeping the freestanding ED fully operational during an emergency event to closing the facility and diverting patients to other sites within the system or region. IT needs and space provisions for a freestanding facility may be different from those of a hospital-based ED supporting an entire building. Adequate space for medical gases and mechanical and electrical equipment rooms varies depending on preferences and needs. The placement of air handling units should be considered in relation to exhaust, intake and site factors such as the loading dock, ambulance bay and helipad location.
Site considerations. Distinct entrances for ambulatory patients, ambulance, decontamination, staff and service should be defined clearly. Access to these points of entry should be intuitive and clearly marked through the use of signage and lighting to define these entrances. Parking for such services normally have a practical demand of 4.5 to 5 cars per 1,000 gross square feet of building.
While outpatient facilities located on hospital sites require that 10 percent of parking space comply with Americans with Disabilities Act requirements, freestanding EDs do not. As with any construction project, the local governing body should be engaged early in the design process to ensure adherence to local planning, zoning and design requirements. Points of concern surrounding FEDs often center on the increased volume of traffic, ingress and egress of ambulance and ground-based transport, and the location and operation of the helipad.
Allowing expansion
Finally, one key to successful operation beyond the opening date is a design that will allow for expansion.
The freestanding ED at the Cleveland Clinic Twinsburg (Ohio) Family Health & Surgery Center was sized to handle an initial patient volume of 17,000 visits per year, which it already has exceeded since its July 2011 opening.
Fortunately, as part of a 190,000-square-foot Leadership in Energy and Environmental Design Gold-certified facility that is master-planned to expand to an acute care hospital, the FED as well as the imaging department and ambulatory surgery center were constructed to meet an institutional classification by its construction type and design.
On the other hand, improvements being considered for another freestanding ED currently in design phase that would improve the capacity without increasing the size include expanding the nurses' station and physician work zone to allow visibility to all patient rooms. This would be accomplished using a split-flow model to accelerate the treatment of less-acute patients, and allowing for more space of EMS squad equipment and reporting space.
An effective option
While FEDs are not the answer to all of the problems facing hospital-based EDs, they are an effective option for expanding the reach of urban-based acute care hospitals and bringing accessible care to their patients. By reaching to the outlying communities, health systems can expand their brand and reach by expanding the hospital's front door.
Philip LiBassi, AIA, ACHA, is principal at Westlake Reed Leskosky. He can be reached at pliba@WRLdesign.com.
| Sidebar - Regulatory considerations in FED design |
| In 2008, the Centers for Medicare & Medicaid Services responded to the growth of the freestanding emergency department (FED) market via a memorandum outlining the differences between "provider-based department of the main hospital" or "stand-alone hospital specializing in emergency services." The design team should be familiar with these requirements because they call for items related to the operational procedures that ultimately will affect the space program, design needs and engineering requirements for the building. Operational procedures require that provider-based, off-site FEDs are permitted if they can demonstrate compliance with the hospital Conditions of Participation (CoPs) and provider-based regulations at 42 Code of Federal Regulations (CFR) 413.65. In essence, regardless of location, the medical staff, core processes, quality and oversight must be commensurate with that of the hospital-based emergency department (see 42 CFR 482.1 through 482.57). In a similar fashion, if there are any additional services, such as surgery, these services must comply with applicable CoPs. A good example of an operational process that impacts design is patient transport (42 CFR 482.55(a)(2)). This process can be handled by ground transport, air transport or both. Another important distinction for the design team to note is that the provider-based approach allows for the emergency preparation plan to be tied to the whole system approach, and would mitigate the need for redundancy of utilities and systems required if the facility is a stand-alone hospital, thus reducing the first cost of construction, and helping to avoid hospital-grade construction. Although redundant systems are not required, the project team may determine that a redundant system is desired. A prime example would be the extent to which services are connected to the emergency power generator. In the initial planning phases, the design team should explore these operational issues (e.g., emergency preparedness plans and long-term strategic plans). |





