ASHE research highlights the field's response to COVID-19

The COVID Response Tactics Sharing survey project tracks the response of health care facilities and third-party collaborators during the pandemic.
Image from Getty Images
The COVID-19 crisis has forced the world to pause business as usual, and to invest valuable time and talent to prepare our nation’s health care facilities. While disease experts released up-to-the-minute guidelines as they struggled to understand how the new, novel virus transmitted itself, health care facilities professionals used this information to problem solve around HVAC air balancing and patient flow solutions. This race to ensure that America’s health care facilities were prepared to treat the influx of very sick patients resulted in huge expansions of patient care space, due in part to collaboration and innovation within the field.
For some areas of the country, the first surge has come and gone but threatens to reappear. This stressful state has contributed to health care facilities professionals’ desire to be able to compare their own surge experience with others and to gather lessons learned for the future. The American Society for Health Care Engineering (ASHE) COVID Response Tactics Sharing (CRTS) survey project gathers these data, synthesizes them into actionable learnings and quickly shares them back with the ASHE community.
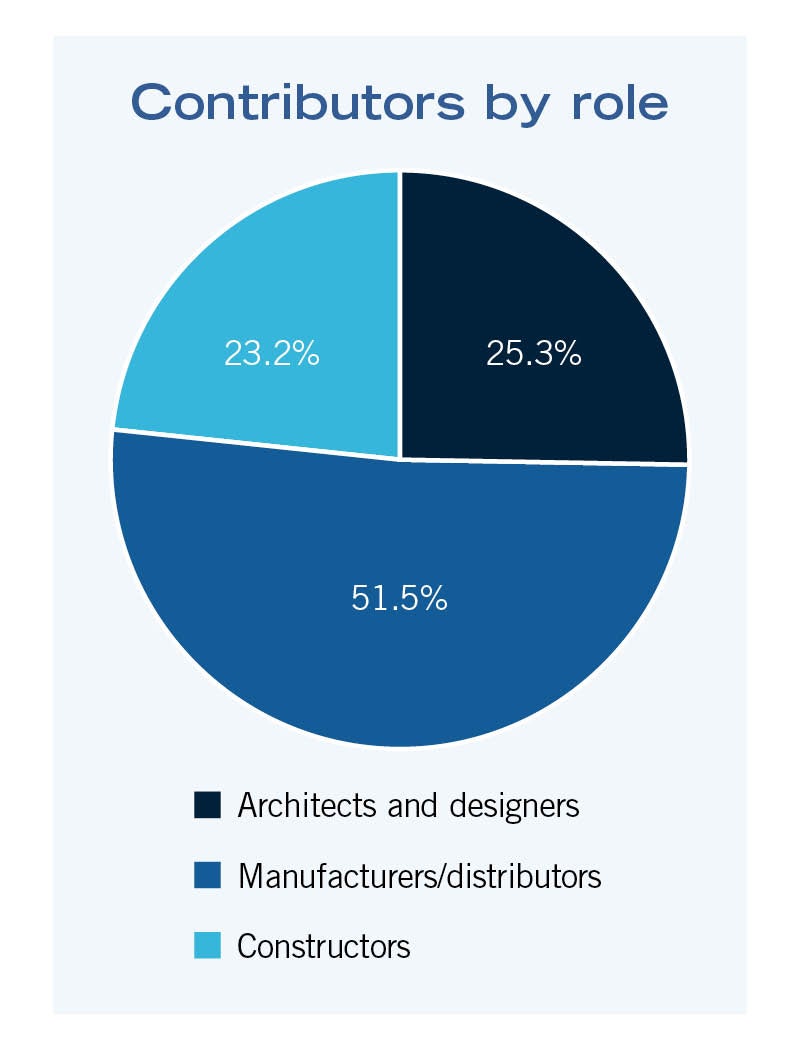
ASHE launched the CRTS in June of 2020 and, as of this publication date, has more than 1,220 respondents from several different health care facilities fields (facilities management, sustainability, education, designers, architects, construction, manufacturing/distribution and infection prevention).
This article, the third in the CRTS report-out series from ASHE, explores the COVID-related perspectives and contributions of partnering professionals, including the architects and designers, constructors and manufacturers/distributors that collaborated with health care facilities to innovate, adapt, design, and build health care spaces and products needed to address the crisis. This group represents 20% of the entire CRTS pool. An earlier report focused on facilities managers and future reports will explore these additional role contributions.
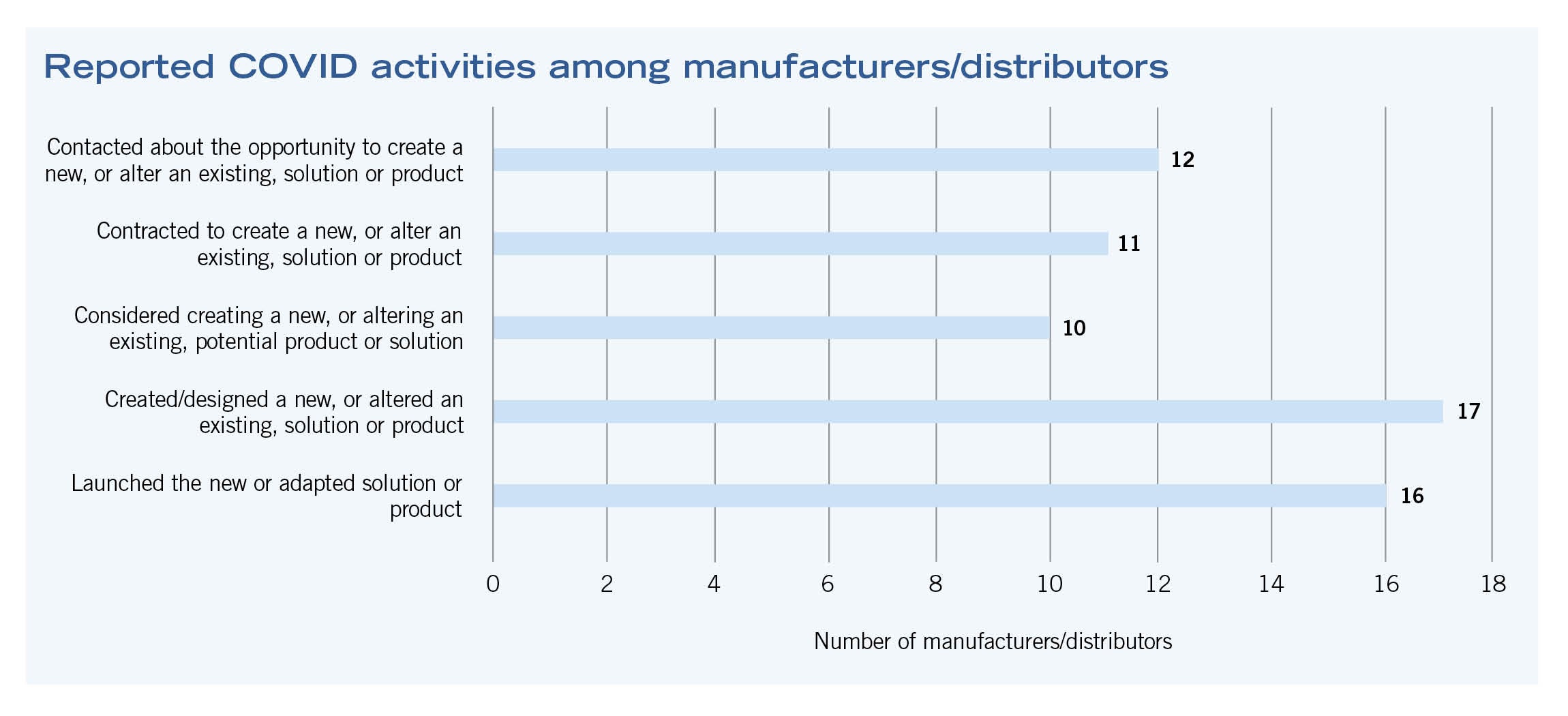
Manufacturers and distributors
Manufacturers and distributors contributed time and talent to COVID response efforts. Approximately 40% of manufacturers were either contacted about creating or altering an existing product or solution, or considered creating or altering an existing product on their own. Thirty-two percent of manufacturers actually created or altered new products. Of those that created or altered COVID-crisis specific solutions, 94% launched their products or solutions.
Some products and innovations mentioned were “surge for demand” KN-95 masks, touchless faucets, flooring solutions for alternate care sites, new approaches to pipe joining that do not require welding (and consequently shorten construction time), a “near UV” light innovation for operating rooms that could potentially provide 24/7 disinfection and an ion machine, which claims to “mitigate the COVID virus … through the distribution of ionized air evenly throughout the space.”
Manufacturers and distributors also described collaborative activities to assist facilities managers, including expediting and assisting the installation of equipment used to supply oxygen and medical air to patient areas, deploying complete modular power distribution systems for temporary COVID facilities using existing inventory, launching a modified version of a surge management forward triage system, introducing new systems of oxygen delivery in nontraditional spaces, and donating personal protective equipment (PPE).
Manufacturers and distributors described the “overall need to change marketing tactics” during this time due to understandable restrictions against vendor visits to hospitals. They also underscored the importance of having direct relationships with manufacturers and alliance partners, which allows for the integration of products from multiple companies into a singular COVID-response solution.
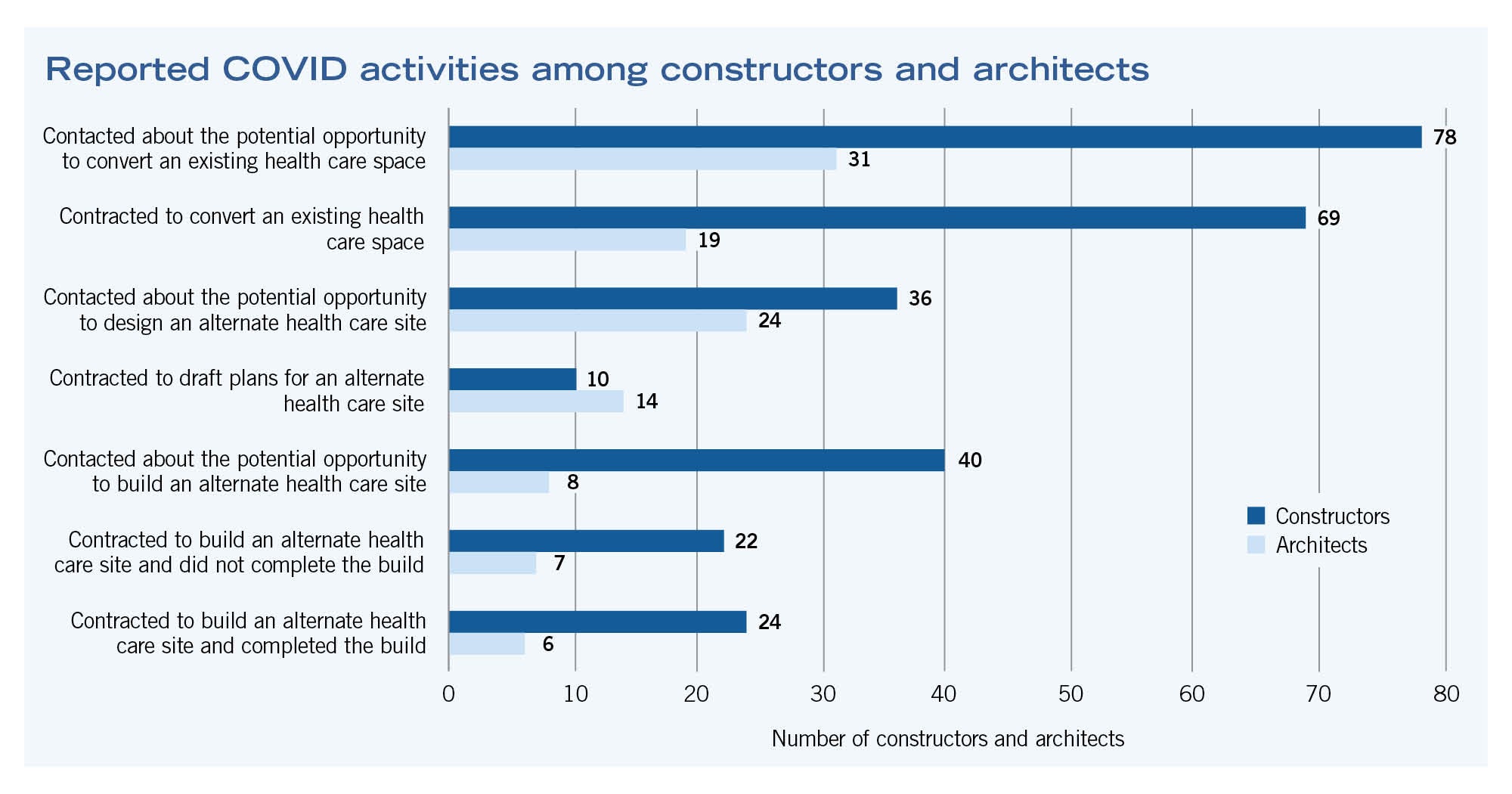
Architects and constructors
The most common COVID crisis-related activities for architects and constructors is represented in the bar graph on page 22. Architects also described other crisis-related activities, including evaluating existing site capacities and patient flow to accommodate patients, designing cohorted patient units, telehealth spaces and “COVID patient care” shipping containers, and engaging in capital project planning and adjustment due to COVID.
Other commonly cited construction activities included air scrubbing/filtration, HVAC cleaning services, access control and PPE monitoring, power washing and disinfecting areas in hospitals, and patient flow and distancing management through the installation of temporary barriers.
COVID has changed how health care facilities are designed and built. Both architects and construction respondents repeatedly cited design-build collaborations, stating that they substantially reduced time to launch. Thus, the remainder of this article combines case examples for both groups.
Respondents were also quick to describe how even the process of health care construction has changed due to the crisis. Eric Pagels, senior project manager for health care at Hagerman Inc., explained that patient and construction team safety are paramount. He described what many other organizations have said is now standard practice: the restriction of all noncritical sales calls; strict implementation of mask-wearing protocols; daily prescreening of tradespersons; and weekly, 10-minute, safety-education focused “Toolbox Talks.”
Pagels also explained how the crisis has delayed some construction projects. For example, a new patient tower built for Goshen Health in Indiana required significant additional approvals and planning to execute utility tie-ins to the central plant. Design professionals also encountered delays finalizing redesign layouts of an existing space due to access restrictions on a floor housing COVID patients.
Pagels explained that these delays have always been expected; however, flexibility and careful advanced planning on the part of the health care constructor is even more important, given the additional risks and requirements of working in health care during the COVID crisis. He repeated the vice president of Goshen’s tenet, “We are not a hospital on a construction site. We are a construction site on an entire health care campus.”
This crisis has also amplified the importance of HVAC and emergency evacuation system design. Pagels describes another project in which a building, designed two years ago but currently under construction, had an impromptu design change to sectionalize supply and exhaust ductwork enabling the isolation of the coronavirus in patient areas.
Similarly, Joe Salama, owner and founder of S-Works Construction, describes an innovative, newly designed emergency evacuation system. Facilities managers from Inova Health and an architecture group designed the bariatric emergency slide system. This system does not require electricity but allows nonambulatory patients of all sizes to be physically transported downstairs. The project jumped in the capital funding process because of its effectiveness.
Collaborations benefit from preexisting alliances and advanced planning. Michael Doiel, AIA, senior vice president and director of project delivery at HDR Architecture Inc., explained how advanced planning and the existence of a previously formed outpatient collaborative enabled the design and facilitated construction and timely deployment of 26 forward triage tent pairs for Advocate Aurora Health.
The collaborative consisted of an architect, engineer, builder and five trade partners. Before the pandemic, they had planned, designed and constructed 31 outpatient centers across Wisconsin and Illinois and, after the pandemic struck, the health care organization’s COVID task force quickly mobilized the group, and the forward surge tents were completed within two weeks.
The tent systems were deployed at all Advocate Aurora ED entrances as triage area “sorting” and “upper respiratory” tents. Patients passed through these tents and were assessed (Tent Area 1) and stabilized, if necessary (Tent Area 2). Non-COVID patients were directed into the emergency department. COVID-positive patients were isolated and transferred into hospital inpatient units. Doiel shares that one strategy for quick emergency response lies in having a preassembled team with a preexisting master agreement ready to mobilize.
Collaborations must be flexible enough to meet patient needs. Several projects focused on meeting the needs of vulnerable populations, particularly those that cannot easily quarantine, such as students and the homeless.
Karl Sonnenberg, a partner at ZGF Architects, described how the team converted an abandoned Veterans Affairs (VA) clinic in Eugene, Ore., to serve as a temporary clinic and overnight facility. This project, a collaboration among the United States Army Corp of Engineers (USACE), Turner Construction and ZGF, relied on seven-day-a-week crews, double shifts and no in-person design meetings to proceed from notice-to-proceed to certificate of occupancy in 20 days.
Design included a four-pod, 42-bed unit (allowing for patient cohorting) with shared private toilet/shower rooms and incorporated an entirely new water system, major HVAC, and low voltage, security and fire life safety upgrades. Especially notable were the quick reactions and teamwork displayed by the design-build team and the authorities having jurisdiction (AHJs) in the city of Eugene and Lane County, Ore.
Officials allowed both a temporary variance to the code governing building occupancy (the former VA clinic was a B occupancy), permitting patient overnight stays and the use of some partition types that were combustible (since initial use was classified as temporary). Sonnenberg added that regulatory officials “could have made things impossible. [They] saw what was important and worked with the project team.”
This same goal was paramount for the DLR Healthcare Group and their team when they paired with internal multidisciplinary health care and justice/civil teams to design and construct a large tent structure to treat COVID patients. The tent structure housed 200 prefabricated pod units configured to negative pressure and allowed families to quarantine together.
In addition, the group, led by the owner’s internal team and consisting of multiple contractors managed by the construction management team, repurposed an existing medical education facility to house beds for less acute COVID patients, including the provision of piped oxygen (O2) to every bed.
DLR Group was part of the design team with the responsibility of code analysis, assessment of plumbing fixture counts, coordination of mechanical-electrical-plumbing trades and oversight of construction. DLR group facilitated the development of the “change of use” documentation for the AHJ (to a temporary surge use: I-2 occupancy), coordination of appointments at each bed location (e.g., headwall and screening), routing of O2 piping, coordination of emergency power locations, temporary lavatories and toilets, and development of documents for the AHJ review.
When asked to reflect on what might be COVID’s largest lessons for health care design, Phil LiBassi, senior principal and global sector leader for DLR Healthcare Group, described two concepts that were running survey themes.
First, he stressed the importance of being able to quickly decide which resources were needed, and then to find a route to obtain these resources. For example, many respondents discussed how entire projects were delayed because they had problems obtaining air handlers. Second, he sounded the call for a shift of focus in the health care design field when he answered, “In a hospital, work takes place at the bedside … not in the lobby, waiting room or lounge. The top priority should be to address the needs associated with treating increased acuity-level patients by including O2 capacity, telemetry, and negative air pressure and dialysis provisions in designs.”
The USACE, Omaha, Neb., district, launched one final case example of design-build innovation. The team included ECC, Hensel Phelps, Davis Partnership Architects, Fentress Architects, RMH Group and Mason Engineering, and collaborated to design and build a 2,000-bed alternate care site (ACS) in Denver’s Colorado Convention Center that housed stable-condition, COVID-positive patients before fully discharging them to their homes. The project was designed in two days and fully constructed in 14 days.
The structure included 10-foot by 10-foot patient rooms located adjacent to nursing stations. Each exhibit hall had several centrally located patient care stations that supported 20 beds each, with enclosed supply and support rooms, including a small pharmacy fed by the central pharmacy on another level of the convention center. Modular patient showers were installed in each exhibit hall as well as separate staff donning and doffing areas to allow staff access to break areas and modular showers.
Ann H. Adams, the principal and health care architect at Davis Partnership Architects, described a particularly challenging code issue that required innovation and design change. The local AHJ would not allow for the typical modular curtained solution used by other ACSs throughout the country. Instead, the team was required to use drywall and steel studs. In addition, the team installed six miles of copper O2 piping, a 13,000-gallon oxygen tank, a nurse call system and emergency power with a 500-kilowatt generator to meet patient needs.
The fast-paced project completely framed 2,000 beds before the space was rescoped to finish with 1,243 beds. “Our team had an amazing amount of respect, communication and trust among our team members, including the USACE,” Adams says. “While it was an incredible amount of work in a very short period of time, we really had fun, in a crazy way.”
Innovative and collaborative
America and America’s health care system still struggles with the COVID crisis and will most certainly continue to struggle for the next several months. However, the COVID crisis, by its sheer disruption and impact, has forced the nation and the health care facilities field to become more innovative and collaborative than ever.
ASHE’s CRTS report-outs aim to illustrate some of these innovations, as well as lessons learned. ASHE thanks all who have participated in this project. Facilities management professionals can still participate in the research by completing the CRTS survey online.
In addition, facilities management professionals who have already taken the survey but wish to update their responses because they have experienced new surge activity can contact ASHE’s researcher at ashe.research@aha.org.
Lisa Walt, Ph.D., is senior research analyst at ASHE. She can be reached at lwalt@aha.orglwalt@aha.org.