Operating and maintaining ventilation infrastructure

The guideline addresses health care HVAC systems as a comprehensive whole while providing consistency in the maintenance and operations of these systems.
Images by Getty Images
Over the last several years, one of the leading survey findings within the physical environment has been the control of ventilation systems throughout health care facilities.
As reported by both DNV Healthcare USA and The Joint Commission, a frequently cited higher-risk accreditation requirement is a failure to properly control ventilation systems to provide appropriate pressure relationships, air-exchange rates, filtration efficiencies, temperature and humidity within care areas.
These findings are common because facilities managers do not have a process to validate whether a ventilation system complies with the requirements of the appropriate American National Standards Institute/ASHRAE/American Society for Health Care Engineering (ASHE) Standard 170, Ventilation of Health Care Facilities, and that the requirements are being maintained per the applicable edition.
To help remedy this situation, subject matter experts have put the finishing touches on ASHRAE/ASHE Guideline 43, Operations Guideline for Ventilation of Health Care Facilities, which is accessible at ASHE's website.
The guideline, developed by ASHRAE in collaboration with ASHE, gives recommendations for the operation of heating, ventilating and air-conditioning (HVAC) systems that provide environmental control in health care facilities for the safety and comfort of facility occupants.
Complex decisions
To illustrate the difficulty deciding which edition of Standard 170 should be applicable to a given hospital’s HVAC system, the Centers for Medicare & Medicaid Services has adopted the 2012 edition of the National Fire Protection Association’s NFPA 99, Health Care Facilities Code, which references the 2008 edition of Standard 170 for new construction and renovations.
Additionally, most states have adopted editions of the Facility Guidelines Institute (FGI) Guidelines for Design and Construction of health care facilities, which includes minimum standards for designing and constructing new health care facility projects. The 2010 edition of the FGI Guidelines includes the 2008 edition of Standard 170. Yet 37 states have adopted later editions of the FGI Guidelines, which include later editions of Standard 170. This causes a conflict over which edition should be used for the design and construction of new health care physical environment spaces.
While determining the appropriate edition of Standard 170 to apply for new construction can be complicated because different editions can be included or referenced within adopted codes, this is a minor issue when compared to another problem — the application of a design standard to the operation of an existing system. While minimum design requirements are essential to properly design and size a ventilation system, these same requirements can cause an increased risk to patients if also used to operate a ventilation system within a health care facility.
For example, the design requirement in the 2008 edition of Standard 170 for operating room (OR) temperature is 68 F to 75 F. However, even the 2008 edition acknowledges that this temperature range may not be sufficient and provides a footnote (footnote o) to the requirements for ORs that allows the requirements to be exceeded if surgeons or surgical procedures indicate that the range is insufficient.
While this footnote is about being able to design the system appropriately for certain types of surgical procedures, such as those for burn victims or neonatal infants, it also tends to address the operation of an OR ventilation system because it addresses the surgeon in relation to these requirements. Many organizations use this footnote to address surgeon requests to maintain the temperature within the OR outside of the 68 F to 75 F design temperature range.
This clearly indicates that there are times when ventilation systems need to function outside of the design requirements. Hence the five-year effort to create Guideline 43 to help health care organizations that are challenged to meet unclear and sometimes conflicting HVAC standards and guidelines established by a variety of professional organizations.
Operational guideline
The intent is to provide an operational guideline for health care facilities that will work in collaboration with Standard 170. First and foremost, the Guideline 43 Project Committee focused on patient, staff and visitor safety and how to best enhance the healing environment. It is the intent of the guideline to provide guidance to operating personnel, thus providing consistency in the operation of health care ventilation systems.
The guideline addresses health care HVAC systems as a comprehensive whole while providing consistency in the maintenance and operations of these systems. The guideline encourages the optimization of HVAC systems and the resources they use through the application of a maintenance program, along with the appropriate application of alternative equipment maintenance and reliability-centered maintenance practices.
The guideline covers the implementation of a ventilation management program (VMP) through defining the responsible party and the minimum elements of a maintenance program, along with providing guidance on legacy systems, condition indicators, excursion variations and program improvement opportunities.
The guideline recommends a VMP based on the risk of harm categorized as either critically or generally ventilated spaces, reliability factors and risk of failure. Additionally, it lists baseline inspection and maintenance tasks for ventilation systems within health care facilities.
Guideline scope
The scope of the guideline applies to all health care facilities and contains guidance for operational parameters and preventive maintenance, based on the capabilities of the infrastructure and the risks incurred in the systems and spaces, including the needs of infection prevention to support asepsis during perioperative care or invasive procedures and for ancillary and support services (e.g. disinfection or sterilization of reusable devices and instruments).
Facilities leaders and their teams are part of a larger hospital team. The ability and methodology to accurately convey capabilities and responsibilities in both normal and emergency conditions should be established and maintained. Construction or maintenance has a significant impact on the function of the facility and puts hospital staff and patients at a greater risk. As such, well-understood policies and guidelines are needed.
The guideline recommends that a facilities leader and their team understand how each piece of equipment is being maintained and should continuously and consistently balance, at minimum, day-to-day unscheduled outages or repairs, scheduled regulatory and maintenance needs, ongoing building rehabilitation and construction projects, and long-term visioning and capital planning.
A decision can be made to follow different maintenance methods depending on the criticality of the equipment and the impact to operations during downtime. Further, understanding the energy and cost impacts should be considered and factored into maintenance decisions.
It also is important to consider the community impact when equipment is offline (i.e., planned) or has failed (i.e., unplanned) and the impact this has on the facility’s capacity and operations. Facilities leaders should accurately assess the needs of the facility, internally or with external support, to provide financial leadership with an evolving capital plan for replacing significant pieces of equipment.
A couple key sections of the guideline include:
Section 5 — Monitored Spaces. One of the important aspects of the guideline is to establish monitored spaces throughout the health care facility. The guideline recommends that ventilated spaces be categorized based on risk of harm. Section 5 provides guidance on critically and generally ventilated spaces.
The guideline establishes critically ventilated spaces as, “Those areas used for invasive or high-risk procedures, infection control isolation, or any space where loss of required airflow, temperature, relative humidity and/or pressure relationships could result in harm, injury or death to patients, visitors or staff.”
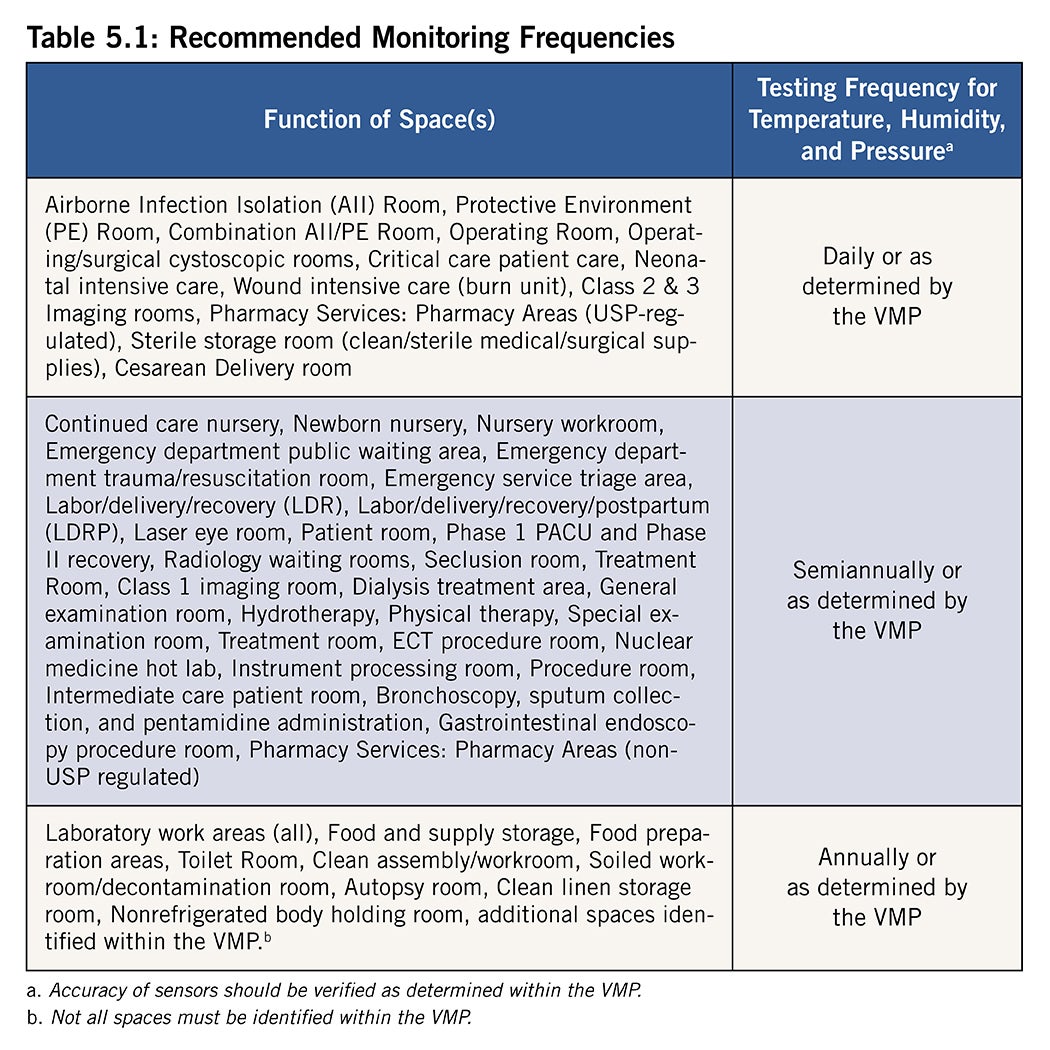
Additionally, operational functionality of a space needs to be periodically monitored and verified. Table 5.1 (see sample below) in this section lists the recommended testing frequency of the spaces and the space parameters.
The guideline also recommends the continued application of building management systems (BMSs) and computerized maintenance management systems for advanced monitoring and verification of condition indicators throughout a health care facility.
While the baseline recommendations listed in Table 5.1 are indicative of a more manual process, the use of BMSs and other automated methods is encouraged and can provide a more reliable and proactive response to excursions from established condition indicators.
The guideline recommends that the VMP should document monitoring and verification processes for monitored spaces.
Section 6 — Implementation. The guideline is intended for all health care building HVAC system owners and applies to all health care facilities. The recommendations are described in terms consistent with a minimal maintenance program. One of the first steps for implementation is to establish a responsible party.
The guideline recommends that health care facilities management organizations be responsible for implementing the VMP and designate a responsible party to oversee the development and implementation of a VMP plan through a multidisciplinary committee.
The VMP should document the capability of the HVAC systems to provide the intended thermal comfort, energy efficiency and indoor air quality required for the health care facility and document the needed HVAC requirements for each space. The VMP should include condition indicators by space function, such as temperature ranges, humidity ranges, pressure relationships, unoccupied turndown application, etc.
The guideline recommends that, at minimum, the VMP should contain the following elements:
- An inventory of items to be inspected and maintained. This list should include at least the manufacturers’ information, location, capacity, maintenance program identifier (if applicable) and other data agreed upon by the responsible party and implementing party.
- A maintenance plan. The maintenance plan should document the work to be accomplished at scheduled intervals on the inventory of equipment to be maintained. The maintenance plan should be developed specifically for the size, design, scope, criticality and complexity of the systems and equipment serving the facility. The plan should describe required tasks, the frequency of tasks and task schedule; identify the party responsible for performing the task; and specify the authorizing party, task completion and documentation procedure, plan monitoring procedures, and procedures for evaluation and feedback.
- Baseline inspection and maintenance tasks. The guideline recommends that frequencies of inspection and maintenance tasks for equipment and systems within the facility be developed and used to develop condition indicators. These indicators are measurements or observations of physical condition and delivery of thermal comfort, indoor air quality and energy efficiency that are learned during the performance of the related inspection tasks. The intent of the VMP is to monitor changes in the indicators over time and provide advance indication of pending equipment failures.
- An operational plan in the event of outages. The guideline recommends that the VMP include a prioritized listing of spaces, departments and services intended to be continuously operated in the event of outages.
- Operational air changes per hour, temperature, relative humidity and pressure relationships. The guideline recommends that the multidisciplinary committee consider ranges for air changes per hour, temperature and relative humidity. These ranges should be considered for existing and legacy systems and based on the safety of patients. A risk assessment process in collaboration with key stakeholders (e.g., leadership for the involved space(s), accreditation/regulatory and infection prevention and control) is recommended to develop alternate protocols.
Section 6 also provides recommendations for excursions. Under certain conditions, the relative humidity and/or temperature in health care facilities will vary from the VMP condition indicators. This section suggests protocols to follow in those situations, though alternate protocols could be developed and documented in the VMP. These protocols are best agreed upon in advance by the multidisciplinary committee to avoid the need for decision-making during stressful situations. Some of the recommended relative humidity excursion rates are provided in Tables 6.8.1 and 6.8.2 of the guideline.
Regarding temperature excursion rates, the guideline recommends that in any space where clinical needs or comfort may require room temperatures that fall outside the condition indicators listed in the VMP, the primary consideration should be the clinical needs of the patient. The secondary consideration should be the comfort of the occupants. The guideline recommends that variations in temperature not based on clinical needs or comfort may vary in the amount of +/- 5 F from condition indicators listed in the VMP for periods not longer than two hours per occurrence.
Finally, the guideline recommends a periodic review of the VMP. A review comparing maintenance program results with the program objectives and condition indicators is advised. The review should include measurements and observations collected during the evaluation period. The actual results shall be compared to the VMP desired outcomes and HVAC system performance. The comparison shall serve to evaluate the VMP performance.
This information should be used to develop a plan for improving the VMP. Program improvement actions should be mutually agreeable between the responsible party and the implementing party.
Consistent performance
The new guideline seeks to render obsolete the longstanding practice of using HVAC design standards as operational practice standards and resolve discrepancies between what is required by design standards and what constitutes nominal HVAC performance.
It is intended to apply to patient care areas, resident care areas and related support areas within health care facilities, and provides recommendations on acceptable temperature and humidity ranges, ventilation rates, operational parameters and preventive maintenance.
Ultimately, it will help facilities professionals address health care HVAC systems as a comprehensive whole while establishing a consistent standard for the maintenance and operation of these systems.
Related article // A look at the future of the new ASHRAE/ASHE Guideline 43
It is important to understand that ASHRAE/American Society for Health Care Engineering (ASHE) Guideline 43, Operations Guideline for Ventilation of Health Care Facilities, was written as a guideline and not a standard.
A guideline is a set of recommendations or best practices providing general advice on how to perform something, while a standard is a mandatory set of rules that, when adopted, must be followed precisely to be in compliance. Essentially, guidelines are advisory, whereas standards are enforceable rules. It has never been the intention to have Guideline 43 adopted as a standard; instead, the document has been developed to provide guidance on how to properly operate ventilation systems within health care facilities.
Similar to how the Centers for Medicare & Medicaid Services (CMS) has recommended handbooks and standards as reference documents for alternative equipment maintenance and water management programs, it is ASHE’s goal to have CMS recommend Guideline 43 as a guideline for ventilation management.
For example, Survey & Certification Letter 14-07-Hospital, dated Dec. 20, 2013, CMS stated, “Likewise an example of written guidelines for physical plant equipment maintenance may be found in ASHE’s [2014] document, Maintenance Management for Health Care Facilities. CMS welcomes identification of other recognized sources of recommendations for facility and equipment maintenance.”
By incorporating the recommendations within Guideline 43 and establishing a ventilation management program plan to operate ventilation systems, health care organizations will encourage accreditation organizations and CMS to accept Guideline 43 as the best way to operate ventilation systems within health care facilities.
Jonathan Flannery, MHSA, CHFM, FASHE, FACHE, is senior associate director, ASHE Regulatory Affairs, at the American Society for Health Care Engineering. He can be reached at jflannery@aha.org.