Key design strategies for pandemic resilience
The COVID-19 pandemic has killed more than 2 million globally and sent many more into hospital care. It has caused people to defer seeking care, temporarily shuttering surgery centers and causing many hospitals — already with narrow margins — to implement layoffs or furloughs, or even to shut down.
Infectious diseases are increasingly likely to arise and become more widespread in the future due to climate migration and the growing spread of zoonotic diseases, and the environments of care must be a part of the solution. Creating facilities that can maintain operations during a pandemic is essential.
Health care facilities need to be safe and demonstrate safety to foster public trust and a return to care. Without this, there will continue to be a monumental impact on the health care delivery system and patients seeking care for conditions like heart disease, cancer, diabetes or a knee replacement.
To help meet this challenge, a guide was created by an interdisciplinary team of architects, engineers, clinicians and medical planners from HKS, a top global architecture firm; Arup, a top international engineering firm; and the American Society for Health Care Engineering (ASHE), the largest association dedicated to optimizing the health care-built environment, with feedback in interviews from professionals across the nation.
“The Pandemic-Resilient Hospital: How Design Can Help Facilities Stay Operational and Safe” addresses design for long-range airborne infectious diseases and leverages synergies between infectious disease care and overall health care priorities, with the goal of creating a flexible and resilient hospital campus.
Interviews with front-line clinical, administrative and executive staff informed the design strategies. However, its authors recognize that no one strategy or modification has been a panacea, and each facility needs unique approaches based on its foundational infrastructure.
This article and accompanying graphics were excerpted and edited from the guide, which can be accessed in full through the resource box on page 26.
Seven principles
The guide’s seven principles for pandemic-resilient health care design offer core considerations, providing a variety of solutions based on a facility’s unique situational needs:
- Versatility. In addition to meeting pandemic needs, the design must work for everyday use and noninfectious patient care to be financially viable.
- Surge ready. The design should support an increase in patients and patient severity on the existing footprint.
- Supports well-being. Pandemic care is extremely stressful on staff, patients and families. The design should support spaces for respite, recovery and well-being.
- Clean air and surfaces. The design should reduce the transmission of infectious particles, while also supporting ease of maintenance and cleaning of air and surfaces.
- Isolate, contain and separate. The design should facilitate the separation of infectious patient care to keep the rest of the patient and staff population safe and support continuity of operations.
- Flow. The design should support clear channels for circulation and flow to support safe movement and minimize transmission risk.
- Digital/physical. Planners must design innovative, appealing spaces and places that allow for seamless transitions from the physical to the digital realm.
Levels of planning
Though not meant to be a one-size-fits-all solution, the guide is emblematic of how the design of space can help facilities to maintain operations during a pandemic involving long-range airborne transmission from various levels:
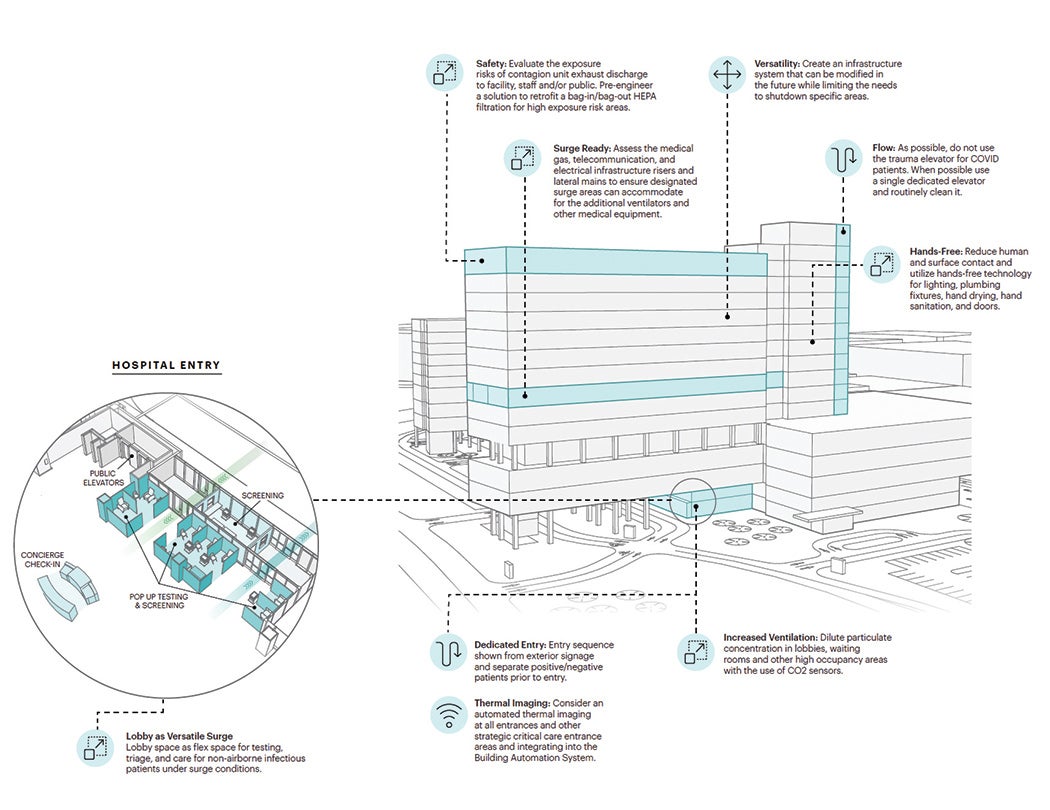
Campus and system level. At a campuswide level, considerations need to be given to how a patient arrives, is screened and tested, and is admitted to the hospital. There needs to be clear signage and communication at a campus level to facilitate this process.
Resources
Regarding patient transportation in most hospitals, one of the primary paths of travel tends to be from the emergency department (ED), where patients are first assessed and discharged or admitted. Buildings and units that have a shorter and more direct path of travel from the ED warrant greater consideration for designated infectious disease care.
Operational considerations such as bed capacity and staffing needs must be considered when choosing the location for a dedicated infectious disease unit.
Technology highlights at the campus and system level include:
- Robust infrastructure, such as remote telecommunication and electrical infrastructure extensions to quickly accommodate temporary setups for testing, triage and entry sequence.
- Flexible wireless nurse calls, such as “rapid response” kits that can easily expand and extend the existing nurse call system to serve temporary triage and bed units.
- Location tracking, such as campuswide real-time locating systems, to contact-trace patients and staff members, and quickly identify and monitor exposure risks as well as assist in patient flow optimization, nurse call automation and equipment tracking.
- Staff resourcing utilizing integration resourcing tools to help allocate proper staffing, sustain operational efficiencies and provide greater flexibility by allowing caregivers to float across departments and buildings when there are shortages of staff.
Building level. At a building level, considerations need to be given to how an infectious patient can receive care safely and separately from noninfectious patients with their surgical, imaging, dietary needs and more. As planners think about patient transportation, they need to ensure separation of flows however possible.
Highlights at the building level include:
- Versatility by adding intentional details like pop-up temporary walls or fitting in clear dividers to separate infected patients while ensuring that life safety and HVAC concerns are considered.
- Designated surge spaces for testing, triage and care that can incorporate necessary medical gas, telecommunication and critical power to support the surge conditions but be used for standard-care purposes.
- Support for the well-being of patients and virtual/physical interaction with loved ones.
- Support for the well-being of staff through locations of respite where staff can safely relax, both within and outside the units.
Unit level. Most hospitals that were interviewed had established at least one dedicated unit for COVID-19-positive patients. Many projects currently in design have modified their plans above mandated minimums to increase their future operational flexibility. This includes an increased percentage of isolation rooms and/or universal design rooms, which quickly can shift from acute to critical care.
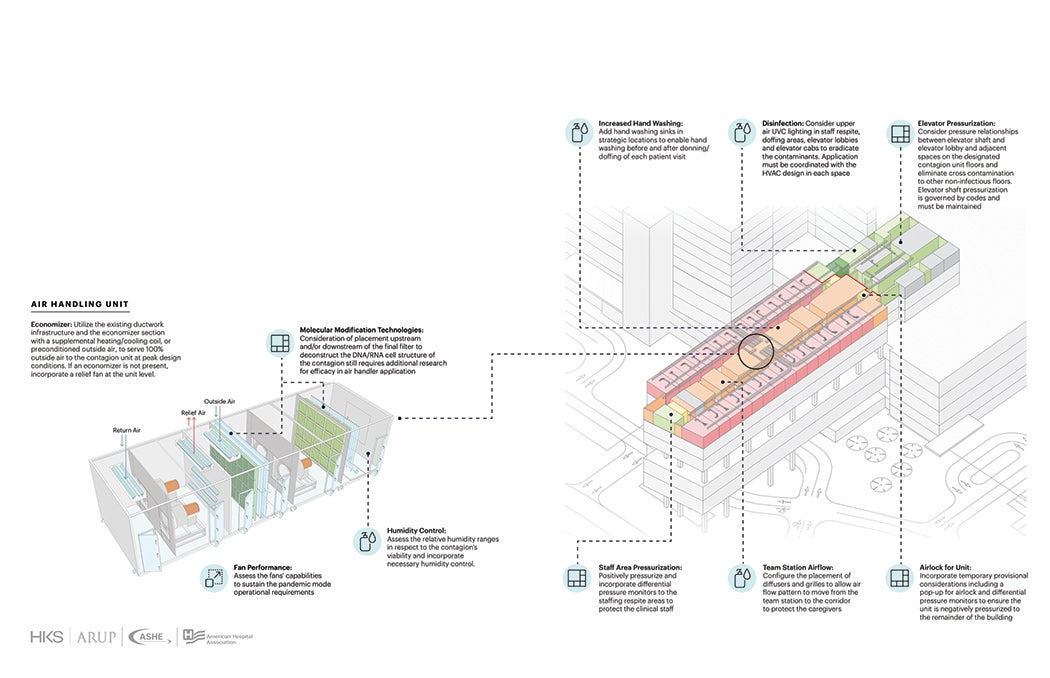
A key component of the unit is to utilize the existing ductwork infrastructure and the economizer section with a supplemental heating/cooling coil, or preconditioned outside air, to serve 100% outside air to the contagion unit at peak design conditions. If an economizer is not present, a facility should incorporate a relief fan at the unit level.
In normal unit mode, special consideration is given to areas that will need high future flexibility; and in pandemic unit mode, the built-in flex spaces are converted to new uses such as materials staging, and donning and doffing.
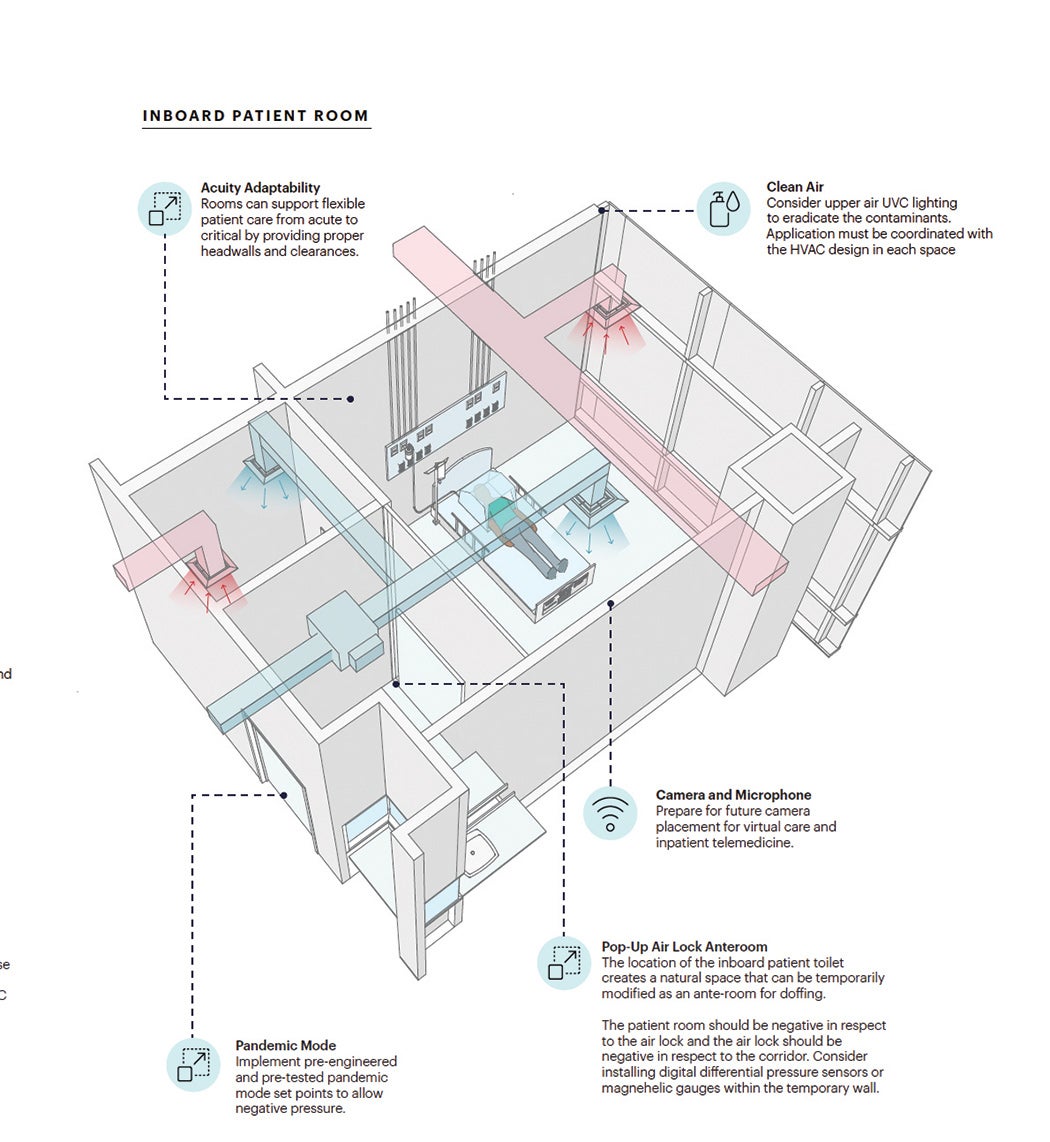
Room level. At a room level, planners need to consider how a room could quickly and safely flex into an isolation room, and adapt to provide higher acuity care, while keeping both the staff and patients safe. This includes clearly marked donning and doffing zones at the door to the patient room with convenient access to personal protective equipment (PPE).
Different room configurations offer trade-offs in flexibility to support pandemic care. A bathroom adjacent to the corridor can create a natural area for a flex anteroom but the bathroom exhaust creates a negative pressure in respect to the patient room, in which case a bathroom on the external building wall can serve to better isolate infectious particles. However, either room type can be transitioned into an isolation room.
Ideally, hospitals would like to follow existing code but, during the pandemic, many facilities needed to limit the number of times that staff members had to go into the patient rooms, and thus use often-scarce PPE.
Many hospitals have passed cords under the door to access equipment like IV pumps without entering. This needs to be done through a multidisciplinary team with leadership and management, and there needs to be clear visibility to the patient from outside the room.
Highlights at the room level include:
- Treating the contagion source directly and shrinking the containment zone to allow the caregiver to be outside of the highly infectious and most susceptible area.
- Providing convenient access to PPE, clear donning and doffing spaces, and patient visibility without having to enter the room can help staff safety.
Key takeaways
Ultimately, the interdisciplinary team that authored the guide offered the following key takeaways for health care organizations to consider:
- Continuity of operations and care is critical to the health care system and the health of patients, and the design of health care facilities can help support this.
- Designing for flexibility, from acuity to isolation level, or the use of multipurpose or flex spaces, is essential in health care design going forward.
- Interventions at the facility level must consider the role of ventilation, power, medical gas and plumbing as a part of any solution to address infection control and pandemic response.
- The solutions to this challenge will look different for each facility.
Key HVAC planning considerations
The hospital air distribution system plays a critical role in protecting front-line essential workers and isolating infectious patients from standard, noninfectious hospital operations. Risk-based, quantifiable targets should be established for the indoor air quality with the goal of reducing the contaminated particulate concentration and increasing the dilution percentage at the patient, room and building levels.
Wherever possible, facilities should treat the contagion source directly and shrink the containment zone to minimize risk to the bedside caregivers, reduce possibility of migration and effectively address the contagion.
Following are key HVAC considerations for infrastructure investment to facilitate safe operations during a long-range airborne transmission pandemic. Risk mitigation measures should be evaluated based on performance specific to each individual hospital application and is not meant to be prescriptive:
Ventilation (system level). Increase outside air to maximum design availability as well as exhaust to outside to increase the contaminant dilution percentage.
Total air changes (system level). Increase total supply and return/exhaust air to infected areas to reduce contaminated particulate concentration.
Air treatment (room and system level). Remove, capture or eradicate the contaminant locally or centrally with filtration and/or molecular modification technologies.
Pressure control (room and unit level). Incorporate negative pressure relationships where isolation from its adjacent space is required.
Airflow pattern (room level). Configure placement of diffusers and grilles to allow air to flow from clean to less clean to protect the clinical staff.
Disinfection lighting (room-level). Utilize upper air (indirect) ultraviolet (UVC) lights in patient rooms and other strategic locations in concert with a complementary HVAC system to kill airborne pathogens that remain in the room. Consider direct UVC lighting for transient spaces.
Key service line considerations
While the bulk of “The Pandemic-Resilient Hospital: How Design Can Help Facilities Stay Operational and Safe” focuses on inpatient environments, the authors recognize that many other spaces help to create a pandemic-resilient hospital. Following are lessons learned across hospital service lines:
Surgical. Because operating rooms (ORs) are central to operational solvency, hospitals have paid special attention to the perioperative spaces, creating designated ORs with anterooms for COVID-19-positive patients separated from the rest of the surgical areas. For perioperative spaces, some new facilities have decided to eliminate all open bay prep and recovery spaces in favor of a three-walled solution, while increasing the number of four-walled isolation bays.
Imaging. For imaging, facilities have screening and masking protocols for all patients. Some facilities have increased the separation between patients by creating gowned-waiting cubbies (three walls with a curtain) or designated four-walled family waiting with a door. These interventions were not only to address COVID-19 but also seen as benefits to patient satisfaction and the ability to have mixed-gender gowned waiting.
Emergency department. The emergency department (ED) offers the first line of defense for most facilities. Many EDs have expanded into adjacent parking lots or lobbies to increase triage and testing, and to separate patients to limit infectious disease spread.
Support services. Support services have always been critical, but now this is even more true — everything from turnaround time of testing to the cleaning of care spaces and the movement of critical supplies, personal protective equipment and clean supplies. These are often considered back-of-house processes, but they are on the forefront of being able to maintain and operate efficiently.
Registration and pre-admission testing. For registration and pre-admission testing, most facilities have expanded their use of online systems paperwork, and many have worked to create individualization of spaces or do more in-room/in-bay registration.
Vaccine storage and distribution. Existing COVID-19 vaccines show a need for extremely cold temperatures for storage. Large-scale vaccination of staff can take place through employee health.
Excerpted and condensed from “The Pandemic-Resilient Hospital: How Design Can Help Facilities Stay Operational and Safe” by HKS, Arup and the American Society for Health Care Engineering.