Successfully navigating an accreditation survey

One of the most important pre-survey activities is conducting building tours.
Image by Getty Images
The days when health care facilities knew when a survey was going to occur are no more. As they should, facilities professionals now live in a time when staff must do the right thing all the time and not just as a preparation for a survey.
Because accreditation surveys are here to stay, it is important for health care facilities to prepare for and manage the survey as efficiently as possible. A surveyor should take pride in providing guidance to health care facilities professionals to achieve efficient and productive surveys, especially when it comes to managing the care environment.
Reducing deficiencies
Accreditation surveys should be opportunities for a health care facility to shine and show the great care and service that is provided daily. Following is stepwise guidance on navigating the survey process to help reduce deficiencies:
Guiding a survey. It should be safe to say that all accrediting organizations (AOs) provide a survey activity guide. This is a playbook for health care facilities to use when preparing for a survey. The AOs will provide health care facilities with information ahead of time on how they will survey the facility. Many times, the AOs will provide information on the type of documentation that will be reviewed so that facilities professionals can have it prepared ahead of time. This prevents health care organizations from being disorganized and unprepared. In other words, the answers to the test are provided, so facilities professionals should study accordingly.
Pre-survey activities. There are a lot of pre-survey activities that facilities can take when it comes to the care environment. One of the most important is conducting building tours. Facilities professionals should get out and see what is going on in the building.
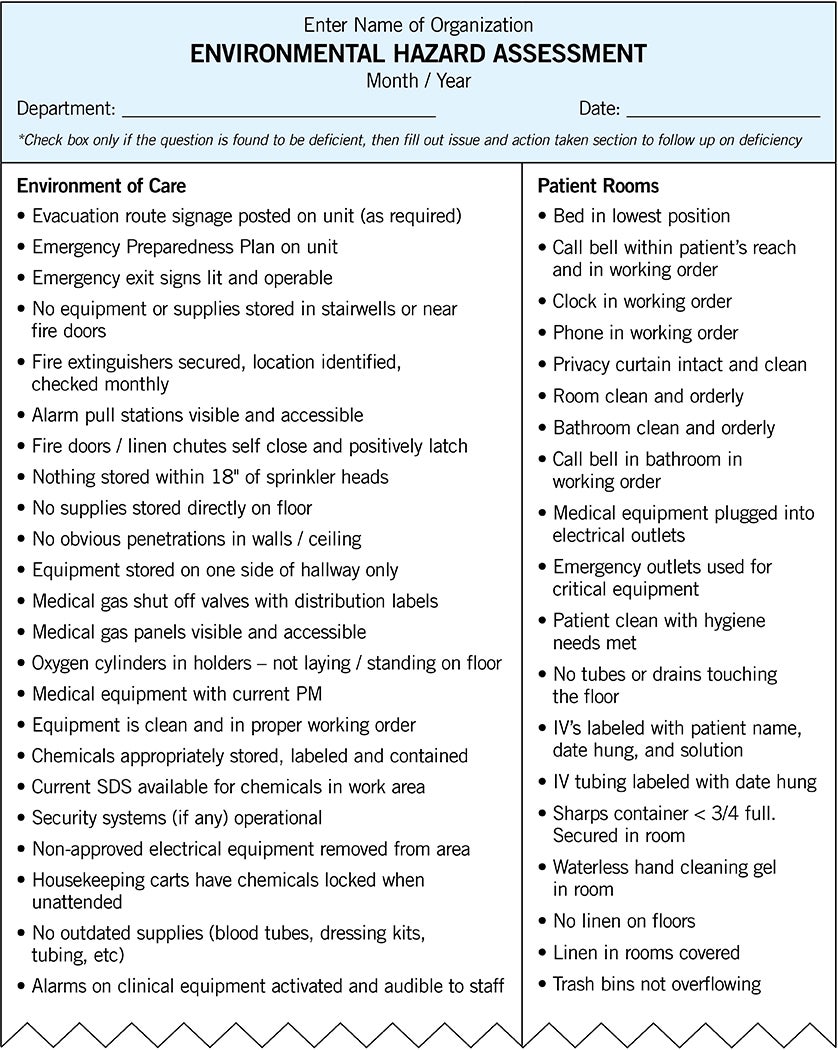
A best practice is to get a group of individuals from different disciplines within the organization to help on the building tours. For example, a team might include representatives from plant operations, infection control, security, biomedical, nursing services and information technology (IT). These individuals should be trained on what to look for in the environment and be provided with documentation tools that can be used to provide real-time information on the state of the care environment. This information then can be used to develop corrective action plans and ensure that deficiencies get corrected.
Typically cited during a survey is not completing an inspection, test or maintenance activity within the appropriate time frame. The easiest way to meet the time frames is to put them on a calendar. Many organizations have large calendars on the wall with the required due dates of the specific tests. Other health care organizations will have an alert issued from an electronic device such as a phone or computer. Organizations that have work order systems will have an alert provided electronically there as well. Organizations should choose whichever way works best. They should just make sure the dates are not missed. It’s a low-hanging fruit during a survey that can be avoided.
It also may be worth having a “visitor” come to the facility and perform a mock inspection. For example, imagine a guest being invited to a house and, in preparation, the owner of the house cleans it. Then, when the guest arrives, they’re such close friends that they are able to point out something in the house that is either broken or dirty. The owner can’t believe it and tells the guest they walk by that area every day and never even noticed it. Mock inspections are a great way to help health care facilities prepare for a survey. Staff walk around the facility all the time and will sometimes become numb to the surroundings. An outside set of eyes can always be helpful.
Monitoring for success. Now that an organization has decided on one of the suggested pre-survey activities, what’s next? Organizations that are most successful in managing pre-survey activities report and monitor the activities through the organization’s quality assurance and process improvement (QAPI) programs. These organizations will use the QAPI reporting process to monitor compliance with inspection, testing and maintenance reports.
As building tours are conducted, corrective actions are developed. These corrective actions are tracked and reported for completions to ensure that items are corrected. The reporting will allow the organization to track issues with which they struggle on a routine basis. In other words, why are these occurring, and how can they be eliminated?
The best example is the all-too-familiar unsealed penetrations through fire and smoke barrier walls. Which is the first department that gets blamed for unsealed penetrations? Most organizations will say the IT department. The process starts by tracking how often unsealed penetrations are found when conducting the building tours. Then, an assessment is conducted to determine why these are occurring. For example, if the assessment determines that the IT department caused 75% of the unsealed penetrations, the organization will take this information and work with the IT leadership to come up with ways to eliminate this problem. Then a process is developed and implemented.
The organization continues doing the building tours and sees a significant reduction in the unsealed penetrations, and that is now reflected in the QAPI program. This is a great way to eliminate the number of unsealed penetrations to create a safer environment, and use the QAPI program to help monitor and eliminate deficiencies.
During the survey. Now that all the pre-work (normal everyday activities) is completed, the organization receives notification that the survey team will be arriving momentarily. There are no worries because the organization is prepared. The survey team shows up, and the organization starts the opening conference. All the introductions are made, and it is time for the life safety portion of the survey.
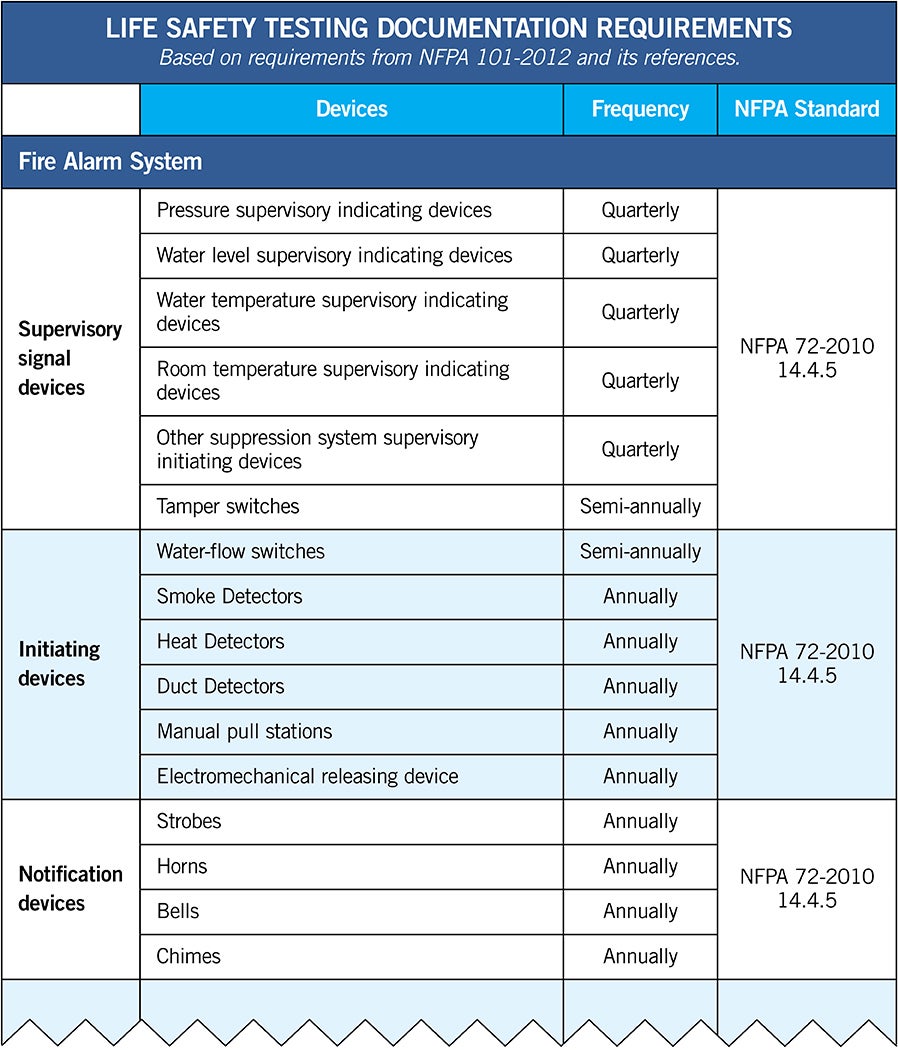
Traditionally, this starts with the document review of testing and operation of systems such as emergency power, fire alarm, fire sprinkler and medical gas. From the point of view of a surveyor, the document review sets the tone for the entire survey.
This demonstrates the importance of having a successful document review. However, there is no regulation that states how the documentation is presented. Health care facilities will provide this information in one of two ways: paper or electronic. Each method has best practices and pitfalls that must be considered by health facilities professionals.
- Paper documentation. As previously noted, the AOs provide a list of documents they will expect the organization to provide. From an AO’s perspective, organizations are required to maintain and provide documentation for an accreditation cycle per the Centers for Medicare & Medicaid Services (CMS).
While organizations must maintain the documents for three years, it is suggested that an organization provide to the surveyor only a 12-month track record of documents, then have the additional 24 months available if the surveyors feel it is necessary.
The best way to present the documentation is in the same order that the AO has requested or that is listed within their standards. Surveyors will typically have a checklist they will be using to document their results. It will probably be in the same order as what was provided to the health care facilities. By placing the documents in the same order, it makes the review flow better when a surveyor asks for a document, and it is immediately available because the organization knows what will be asked for next.
A typical organization will provide the documents in a binder. If a test is required annually, facilities professionals should keep the most current document in the binder. If it is a quarterly test, they should keep the last four quarters. If the organization has a test that is required outside of a 12-month time frame (e.g., a five-year test), the facilities professional should keep the most current document in the binder, even if the document was created outside of the past 12 months. It can get a little frustrating when the record is requested and staff must try and find out what year it was performed, then find the right binder.
A whole other discussion could be had about the information the surveyors will be looking for on each document. For the purposes of this article, the emphasis is on the presentation of the documents. It makes the rest of the survey flow much better.
- Electronic documentation. Some health care facilities have their testing records stored electronically. Typically, these documents are presented up on a screen for the surveyor to examine. Similar to the paper-based approach, the electronic presentation needs to be simple. Instead of binders, the organization will have electronic folders to keep the documentation. Each folder should be named like the binders. An example of this system includes:
- Folder: AO’s standard number for emergency power.
- Folder: Monthly generator test.
- Folder: Calendar year.
- Folder: Month (January to December).
- Place each testing record for the given month in the folder.
When presenting the electronic documentation, the organization will need to make sure it is in a font and size that can be easily read from a distance.
Whether the organization chooses to present the documentation via paper or electronically, it is recommended that the organization perform a test presentation frequently. Most organizations will receive the documents, place them in a binder or computer, and then not look at them until a surveyor asks for them.
When performing a dry run on the document presentation, the organization should have different personnel present at different times. The reason is that if only one person knows where the documents are and how they are laid out, there is a chance that particular individual is not available when the document review occurs.
Having multiple people trained on how to present the documents will give the organization a better chance of success during a survey. Another frustration during a document review is asking for records and the staff not knowing where to find or access the information because the primary individual is not available.
Building tour. After the document review comes the building tour, when the surveyor walks the health care facility. A common question is, “What exactly do the surveyors look for?” Most surveyors look at everything. The best source for health care facilities professionals to reference when trying to figure out what surveyors look for is the CMS K-tags.
These tags for health care occupancies can be found on the CMS form 2786R, Fire Safety Survey Report. This will provide a list of what surveyors are looking for. Each surveyor may do their building tours a little bit differently than others but, in general, they all look in the same places. A general but incomplete overview of the areas they will go to includes:
- Fire alarm control panel.
- Emergency power supply systems (e.g., generator, automatic transfer switch and master alarm panel).
- Bulk oxygen systems.
- Fire pumps/sprinkler risers.
- Fire department connections.
- Medical vacuum pumps.
- Mechanical spaces (e.g., boiler, chillers and electrical rooms).
- Patient care areas.
Knowing ahead of time where the surveyors will focus will help organizations prepare those spaces to always be survey ready.
Post-survey activities
After the survey, the organization receives the report from the AO and develops a corrective action plan to correct the deficiencies. When developing a corrective action plan, facilities professionals should make sure that the organization is addressing the issue that was deficient and not trying to change the world. Many organizations develop a corrective action plan that is unattainable and unsustainable.
When the AO returns in three years for the next survey, they will be reviewing the organization’s previous report and action plan. AOs are required to monitor for generational findings. These types of findings have been cited previously and a corrective action was provided showing the health care facility corrected it. Then when the AO returns, the same issue is still being cited. The best way to prevent generational findings is by monitoring the corrective action plans.
An overview of CIHQ and its services
The Center for Improvement in Healthcare Quality (CIHQ) is a Centers for Medicare & Medicaid Services (CMS)-approved deeming authority for acute care hospitals. CIHQ’s accreditation program is designed to ensure that hospitals comply with the Medicare Conditions of Participation (CoP) and improve the quality of care, treatment and service in their communities.
CIHQ offers the Healthcare Accreditation Certification Program (HACP), which is dedicated to demonstrating competency in select fields of the regulatory environment. Currently, the HACP program encompasses a broad knowledge of the CMS CoP for acute care hospitals, and the federal survey and certification process. The HACP-PE (physical environment) certification demonstrates an in-depth knowledge of regulations addressing the physical environment in acute care hospitals.
CIHQ offers Center of Excellence (CE) programs designed to recognize hospitals that meet or exceed national standards and evidence-based guidelines in the care, treatment and service provided to their patients and staff. CE programs are available to any hospital regardless of their accreditor. Programs include those for long-term acute care, rehabilitation services, rehabilitation services for stroke care, respiratory therapy, environmental health and safety, nursing services, palliative care and emergency services.
CIHQ standards and requirements are mirrored after the CMS CoP and their interpretive guidelines. Hospitals that are accredited by CIHQ receive standards and regulatory interpretation; notification of changes to standards and regulations; unlimited access to the electronic resource library; unlimited access to the comprehensive reference library; complimentary access to their monthly audio conferences; discounted rates to the annual CIHQ Accreditation & Quality Summit; unlimited access to the continuing education center; and various types of staff training presentations.
Billy Kinch, MHA, HACP-PE, is the lead facilities specialist for the Center for Improvement in Healthcare Quality, McKinney, Texas. His email is wkinch@cihq.org.