Evaluating the effectiveness of hospital fire drills
The requirement to perform fire drills in health care and ambulatory health care occupancies has been around for as long as most can remember. Although most hospitals will never experience a fire in their facilities, health care facilities staff still apply rigorous training protocols related to fire safety.
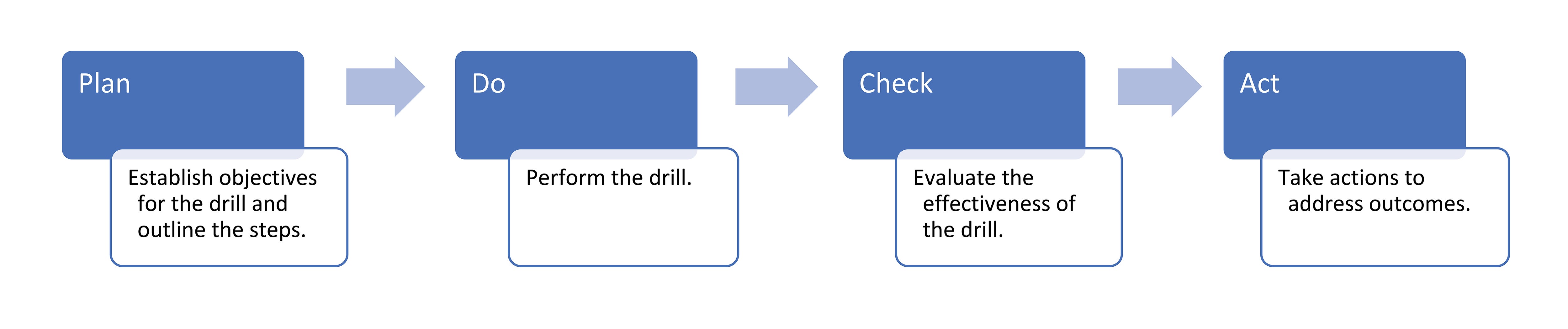
How does a health care organization determine whether an effective fire drill program is in place? How does a hospital continually improve a process it may never have to utilize in a real-world scenario? Applying the plan-do-check-act (PDCA) model, will formalize the process for continual improvement. How does this work?
Health care facilities shall have written fire control plans that provide training of staff in the areas outlined in the 2012 edition of the National Fire Protection Association’s NFPA 101®, Life Safety Code®, 18.7.2.2/19.7.2.2, which contains provisions for prompt reporting of fires; extinguishing fires; protection of patients, personnel and guests; evacuation; and cooperation with firefighting authorities, among other individual facility requirements.
In addition, NFPA 101-2012, 18.7.1.6/19.7.1.6, requires drills to be conducted at least quarterly on each shift to familiarize staff with requirements and expectations set forth by their facilities. When applying the International Organization for Standardization’s ISO 9001-2015 management system concepts, facilities are required to analyze the effectiveness of various processes.
Most facilities develop their fire drill process around NFPA 101 and include some type of scoring system. Depending on the parameters for the scoring system and elements for success, goals and objectives are established with defined criteria and benchmarking protocols.
For example, a hospital creates an evaluation form for a fire drill with 10 delineated benchmarks that include, but are not limited to, locations of fire extinguishers, closing doors to patient rooms and verifying timeliness of notification to a central monitoring center. Each delineated benchmark is scored at 10 points, and when the evaluation is complete, a total of at least 90 of 100 points is considered a passing score. The facility has three shifts in a day that are scheduled consistently this way for an entire year; therefore, a minimum of 12 fire drills are required to be completed, and the goal is to have at least 10 or 11 fire drills receive a passing score. When this occurs, the health care facility determines there is an effective fire drill program for the evaluated year.
When does continual improvement apply? The health care facility trends fire drill results over a defined period. When satisfactory results are consistently achieved, goals and objectives are changed or evolve to move up the level of success and/or evaluate newer or different benchmarks. Doing the same thing over and over is counterintuitive to one of the basic principles of continual improvement.