An innovative space for proton therapy

Inside the treatment rooms, large-scale graphics and soft, integrated lighting provide a positive distraction and create a comfortable environment for patients.
Image courtesy of Gresham Smith
One of the most significant advancements in combating cancer has been in the field of proton therapy, which in the past few years has benefited from startup companies and clinical innovations to create delivery systems that are lighter, leaner and less capital-intensive while providing highly effective care to a wide range of patients with limited side effects.
Using protons to treat cancer had been hailed as a groundbreaking milestone as the first commercially viable centers began to be developed around the country in the early 2000s. A precise form of radiation therapy, proton therapy destroys cancer cells without extensive impact on the surrounding healthy tissue.
The process of generating protons requires a significant amount of energy and results in a high level of radiation. High-energy cyclotrons or synchrotrons are used to accelerate protons, increasing their speed and energy to generate the proton beam. This proton beam, carefully controlled and shaped, is then modulated along a beam line directed toward one or more treatment rooms.
Within these treatment rooms, a pencil-beam scanning nozzle attached to a rotating gantry is employed, enabling precise “painting” of the tumor target with protons. This level of precision allows for the customization of treatment plans to ensure the maximum therapeutic effect while minimizing damage to adjacent organs.
Given this cutting-edge technology and high degree of precision, it’s not surprising that some proton therapy facilities may face complications during planning, design, construction and even operations.
Groundbreaking milestone
In 2013, the newly constructed McLaren Proton Therapy Center of the Karmanos Cancer Institute in Flint, Mich., was facing several issues. As the date approached for its originally planned opening, the center encountered setbacks. Its two primary technology partners — responsible for the cutting-edge equipment required to safely deliver this advanced form of radiation therapy to hard-to-treat cancers — had both gone bankrupt.
What’s more, approval from the Food and Drug Administration (FDA) for patient treatment had been delayed, and at the heart of the whole process, the three-story gantry that modulates the beam and rotates it around the patient to target tumors from different directions encountered technical issues that slowed patient treatment times, necessitated additional staff and increased maintenance demands.
The technology required to create the protons is incredibly complicated, precise and carefully controlled, and the building and systems supporting the technology need the same level of precision in their design and coordination. Because the accelerators generate radioactive neutron particles during the process, the accelerator vault, beam line and treatment rooms are heavily shielded to safeguard patients and health care providers, incorporating concrete walls and ceilings that range from 4- to 12-feet thick.
The gantries that rotate to deliver the beam to a stationary patient are custom-made and three stories tall, as well as heavy, expensive and complicated to install and maintain. The beam line is modulated with magnets that control intensity and allow the beam to alternate between treatment rooms.
Additionally, the treatment rooms contain sophisticated imaging and positioning equipment to control the location of both the beam and the tumor.
In most technology-related projects, when things don’t work as intended, there are usually resources to turn to — an expert, a vendor or maybe a supplier. That was not the case for this first-of-its-kind proton center. The finished installation of the equipment at McLaren failed to produce a high-quality beam to the point of treatment. It was determined that the manufacturer’s gantry design was insufficient, leading to extensive maintenance downtime, and the organization’s technology partners were unable to help.
Compounding these challenges, the center was experiencing high demand, compelling it to extend operating hours, sometimes until 10 p.m., to meet the needs of its patients. Although delivering treatment at the newly opened center was inefficient from a financial perspective, it was very effective from a patient-care perspective. Once it was up and running, McLaren was reluctant to interrupt service for repairs.
While the gantry in the first treatment vault had been successfully rebuilt before the center opened, the second vault’s gantry consistently required maintenance and recalibration to keep it working. A viable solution was imperative to sustain services at the current level, and it had to be financially feasible within the business constraints of a nonprofit organization.
Resourceful team
Fortunately, McLaren possessed a resourceful team and a pool of expert caregivers, researchers and technicians among its staff. They embarked on an ambitious and entrepreneurial program to solve problems, explore options and test solutions.
The center was originally designed with two patient treatment vaults; a third vault was left unfinished for future expansion. McLaren’s Dan Medrano, corporate vice president of facilities, and Vahagn Nazaryan, Ph.D., executive director of the McLaren Proton Therapy Center, looked for ways to outfit the third vault for patient care.
While it had been designed for the same gantry system as the other vaults, using that manufacturer again was a non-starter. There were no other suitable existing gantry systems available to procure and install. They considered a gantry-free design with just a fixed beam, but discarded this option because it would limit the types of tumors they could treat at a time when they were starting to see more varied and complex cases.
One option was to engage outside consultants and fabricators to design, engineer and manufacture a custom gantry system. While that seemed like an obvious solution, it would have significantly impacted their cost and schedule. Encouraged by McLaren’s corporate and clinical leadership to embrace an entrepreneurial spirit, the project team pushed forward with other ideas. Having gained expertise in the technology, they considered designing and building their own gantry system. However, their analysis determined that, along with delaying the schedule, this approach would have added an unacceptable level of risk to the enterprise.
The ideal solution would need to deliver care to a variety of patients, open within a reasonable implementation schedule, operate at an acceptable level of patient throughput and still provide a return on their investment.
Proton therapy technology providers had been grappling with the same challenge, prompting McLaren to investigate the latest generation of delivery systems. For instance, instead of rotating the nozzle of the beam around the patient using a three-story-tall gantry weighing 100 tons, some new systems were exploring the concept of keeping the beam fixed while rotating the patient to face it.
Several manufacturers were testing equipment for this, and McLaren joined forces with the British firm Leo Cancer Care, which has a U.S. office in Middleton, Wis. Leo’s delivery model involved having the patient sit upright in a special treatment chair, utilizing a sophisticated positioning system and a built-in computed tomography scanner to move the patient and align the tumor with the fixed beam’s path. Together, they were able to refine Leo’s prototype to accommodate their patients’ needs, align it with the existing beam line and utilize it in the shelled vault.
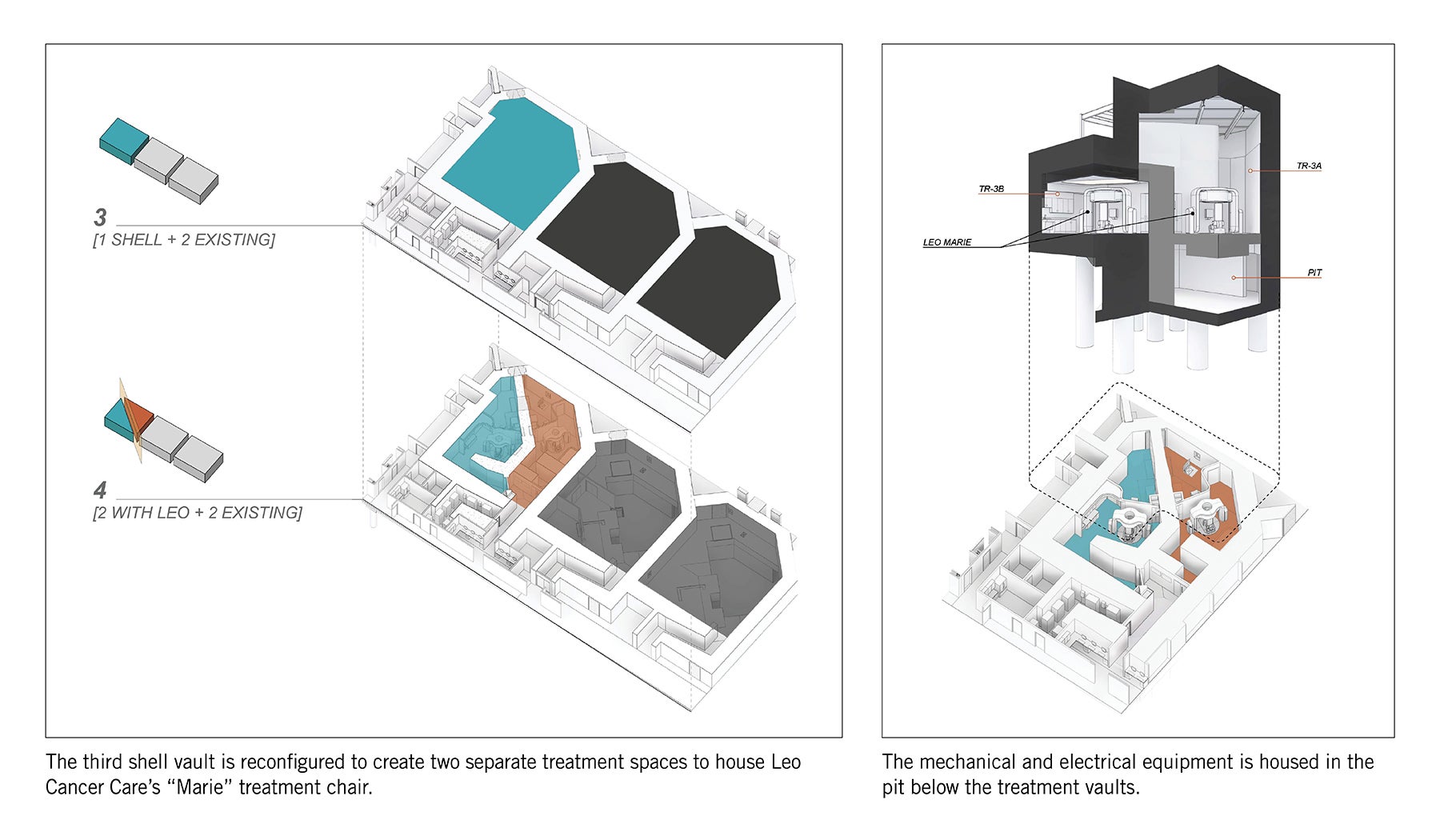
During the discovery process, it was proposed that if the proton beam line was split at the vault entry, two chairs could be installed in that space, increasing the overall patient throughput. The team projected that enough additional revenue would be generated to justify the renovations required to the existing vault.
Although the upright system was not initially embraced by the clinical staff — who were used to treating patients in a lying-down position — the advantages of the system gradually won them over. Setup is faster, fewer clinicians are required, and communication and eye contact with the patient is easier. Additionally, patients breathe more naturally, have less movement of internal organs and experience greater comfort. This approach also reduces agitation and increases patient engagement in their treatment. Further, pediatric patients appreciate seeing what’s happening in the treatment room and watching a game or movie on a tablet.
One challenge at the outset was that the chair system had not yet been installed in any center in the U.S., and the FDA still needed to approve it for patient use. More significantly, all the associated components needed to be coordinated and, in most cases, modified to make them all work together.
The McLaren team already experienced technical problems in the original installation where different systems didn’t match up, so an extensive program of review, coordination, exploration and analysis was implemented as design of this new system began. The architects modeled the space in 3D and provided virtual reality goggles to users, technicians and manufacturing partners so they could understand the spatial impact of their decisions. The dosimetrists were able to better understand what their workflow would be with the new technology, and the camera system designers could confirm that other equipment would not obscure their view.
Then a full-scale mock-up, including the installation of a functioning treatment chair, was built within an unused procedure room. Software was tested and revised. Structural supports for components were integrated within the architecture so the space could remain patient-focused. The process had to be highly collaborative as this unique technology was assembled for the first time, with the clinicians, engineers, technicians and architects all working together to apply their individual expertise and areas of specialty to the singular vision of optimized patient care.
With the decision made to proceed with the two chairs, three concurrent design tasks unfolded. The McLaren team, along with their new technology partners, began to develop the process to switch the beam at the vault entry between two fixed nozzles directed at independent isocenters. Simultaneously, McLaren and Leo started to refine the design of the Leo “Marie” chair, ensuring it fit onto the existing vault and beam isocenters.
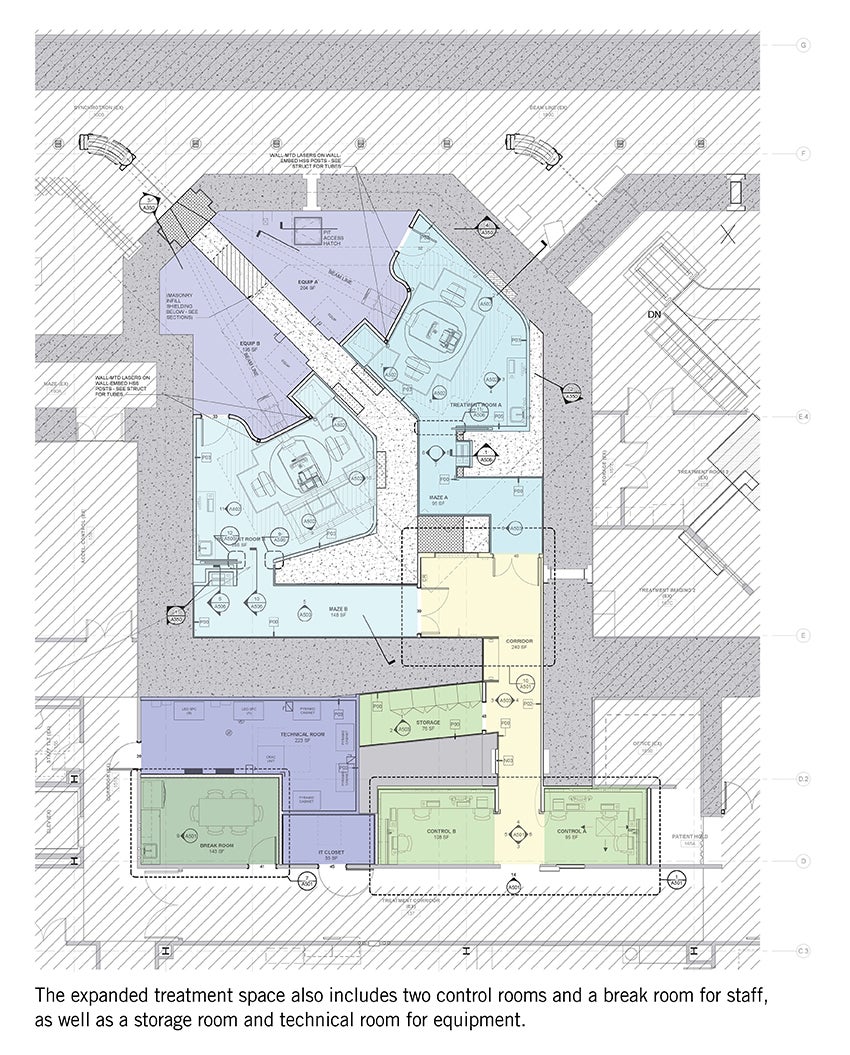
In the meantime, the architects and engineers began conceptualizing the revisions needed to convert a single, three-story vault into two vaults. This included designing a center shield wall, a second maze entry and a new basement mechanical room.
Additionally, the new delivery systems and increased patient throughput meant that support space for the additional technology, research, treatment planning and administration would be required. This led to an expansion of the entire complex. Much of the new space will be housed in a horizontal addition of the proton center while concurrently the adjacent cancer center is slated for a vertical expansion.
Throughout the process, risks and costs were continually evaluated. Ultimately, the business and clinical success of the unique project owes its success to the users, clinicians and researchers on staff, along with their trusted partners, who were able to understand the problems, envision solutions, select the right options and, finally, create technology that didn’t previously exist.
The proton center’s third and fourth vaults are under construction, and pending FDA approval, McLaren plans for the first of the Leo Marie chairs in the U.S. to be operational in the third quarter of 2024.
Entrepreneurial spirit
McLaren built upon a culture of entrepreneurial spirit among its own staff that guided and made significant input to the entire process. As Nazaryan says, “Health care systems don’t [typically] do efforts like this. Essentially, we are acting like an entrepreneur creating a new technology.”
Medrano recounts a reaction from one of their technical partners. “She heard our story and thought that we had put together some sort of ‘Frankenstein’ machine. Then she had the opportunity to visit us and see that we were a robust, highly efficient proton therapy center, operating at capacity. She told me, ‘If this had happened to us at our company, I don’t think we would have known what to do.’”
About this article
This feature is one of a series of articles published by Health Facilities Management in partnership with the American College of Healthcare Architects.Sandy Faurot, AIA, ACHA, LEED AP, is a vice president in the health care market at Gresham Smith, and Goran Vukovljak, AIA, LEED Green Associate, is project executive and senior health care architect at Gresham Smith. They can be reached at sandy.faurot@greshamsmith.com and goran.vukovljak@greshamsmith.com.