Built for savings
 While many experts are predicting health care construction will continue on a level plane in 2012, don't tell Kip Edwards that building activity is calm.
While many experts are predicting health care construction will continue on a level plane in 2012, don't tell Kip Edwards that building activity is calm.
The vice president of development and construction for Banner Health, Phoenix, is coordinating 185 active projects at his system's 22 locations, ranging from chiller and roof replacements, to high-tech cath lab and operating room renovations, to new additions and patient towers.
But, in a health care environment buffeted by reduced funding and future uncertainty, it's no surprise that short- and long-term costs are key in determining whether any project advances.
"We manage our project budgets to the scope that's approved and resist the urge to keep adding to it just because there might be money available there," Edwards says. "The other thing we're doing is being more cautious and methodical about what gets funded because we have limited capital available."
Smart design
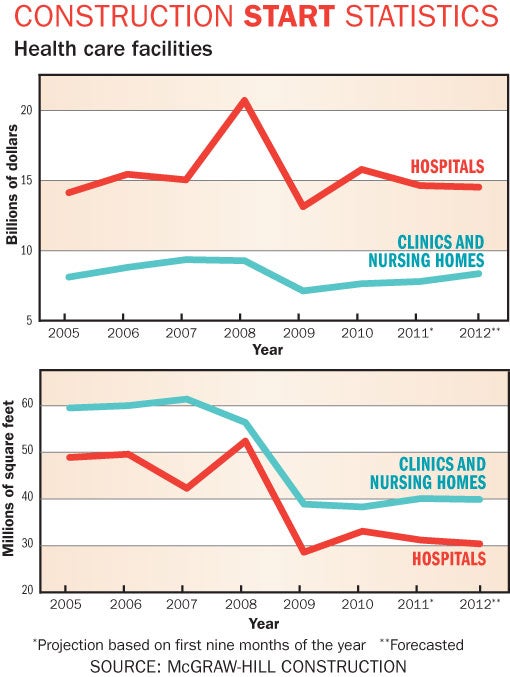
Triggered by the economic meltdown and credit crisis followed by uncertainty surrounding health care reform, the construction crash of 2009 put many big and small projects on hold as organizations checked their portfolios, rewrote their long-term plans and put a sharp pencil to subsequent building projects.
Those sharp pencils have stayed out as health care construction stabilized at a lower level of activity, forcing planning, design and construction professionals to prove their worth to health care organizations by squeezing costs and increasing efficiencies, according to Joe Sprague, FAIA, FACHA, FHFI, principal and senior vice president at architecture firm HKS Inc., Dallas.
Describing what he calls "smart sizing," Sprague says efficient designs can reduce a project's size by 20 percent, saving construction costs and operational costs as well. "I think what it boils down to is every design must have utility to it and an outcome that produces favorable results," he explains. "So by designing smart you need less capital and also spend less on the operational side since design is only about 4 percent of the cost of running a hospital amortized over the life of the building."
Elements of this approach, which may complement a health care organization's adoption of Lean operation principles, include an appraisal of the functional program and the work flow in the facility's planning stages, paying careful attention to reducing travel distances, increasing flexibility and eliminating unnecessary space.
"You're really looking at an analysis of the design that reduces the requirement for space and potentially requires less staff," says Sprague, who is also president of the Facility Guidelines Institute, publishers of the quadrennial Guidelines for Design and Construction of Health Care Facilities. "In patient rooms, for example, we have minimum clearances in the guidelines for areas around the bed and where you're able to locate the bed to maximize those clearances without impeding the function of the space."
Indeed, Banner's Edwards believes that patient rooms and operating rooms are both likely to halt their decades-long, square-footage growth spurt, though he adds that technology demands make it unlikely they will shrink to 1980s' levels.
Kirk Hamilton, FAIA, FACHA, EDAC, professor of architecture at Texas A&M University, College Station, draws on his days as a practicing hospital architect to present a compelling vision of what can be achieved under such constraints.
"A project I had some years ago was a small hospital in Utah that was going to be abandoned because it didn't meet the seismic requirements and it was too small to make money," he remembers. "Ultimately, they didn't want to abandon the community so they said, 'OK, we will replace it, but it has to be the most efficient hospital that we've ever seen.'"
With the goal of making the net-to-gross ratio of space for every department as lean as possible, Hamilton's team eliminated departmental barriers and combined them.
A multimodality suite was planned for the hospital instead of separate suites for endoscopy and surgery, for instance, and a multimodality diagnostic center was designed to include imaging and cardiology. Similarly, exam rooms for the diagnostic center also would be used by the emergency department.
"Ultimately, 36 departments in the existing facility became 12 in the new building, which changed the operational costs because it changed the management and salary structure," Hamilton sums up. "It became one of the top-performing hospitals in the system, which was a big shock since the small ones aren't supposed to outperform the big ones."
Moving beyond space design to infrastructure elements, integrating such information technology assets as electronic health records, diagnostic equipment and even telemedicine in a way that improves clinical flow and allows for future flexibility and expandability is also an important way to save long-term costs.
"If hospitals are committing to build a project, they don't want to hear that they're going to have to completely renovate just because they may have new modes or new pieces of equipment coming in later," comments Andrew Quirk, senior vice president for Skanska USA Building Inc.'s Healthcare Center of Excellence in Nashville, Tenn. "They're looking to build assets that are flexible enough to change with technology."
Sustainable, energy-saving systems are another way health care organizations can achieve savings through their infrastructure and design choices, he adds.
"I think this is one of the next big opportunities to add to the bottom line in the health care industry," Quirk says. "When you're building an addition or renovating a space or upgrading your chillers and boilers, you can make some key decisions that will actually save significant amounts of money and have a very short return on investment."
Finally, experts say, potentially costly changes in the Centers for Medicare & Medicaid Services' preventable readmission policies have put pressure on everybody on the design team to up their game as they may influence infection control, medical errors, and slips and falls.
Construction performance
The key to turning these plans into a cost-effective reality, of course, is an efficient construction management process. And, in this, too, health care planning, design and construction professionals have redoubled their efforts.
"Health care organizations want to know what measurable value you're going to bring the team, such as incorporating Lean principles into the design and construction process," says Skanska's Quirk. "So, one of the things we look at is construction efficiency — how quickly we deliver projects, how we can affect quality of projects — all with the idea of maximizing the organization's investments and getting them to generate revenue faster."
Construction professionals agree that bringing value to the construction process requires assembling the project team early. In fact, many recommend adopting an integrated project delivery (IPD) process to bring architects, contractors, facilities staff and even major subcontractors around the table to provide "design assist" services, work through any potential problems and eliminate potential wasted effort before construction begins. If a formal IPD process is not possible due to legal concerns, some say a "functional IPD" or "IPD lite" approach used in conjunction with another delivery process also can be helpful.
An added benefit of bringing the team together early is minimizing duplication of design by handing off the design documents at the right time, according to Jim Eaton, vice president at McCarthy Building Companies Inc., Atlanta. Having team members involved earlier provides a clearer understanding how complex the construction professionals need to be with their design documents before they are passed along, he says.
All agree that an important tool in any planning effort is building information modeling (BIM) software, which has become an industry standard over the past several years.
"It certainly doesn't replace the need to have hands-on mock-ups, but the visualization aspects of BIM are important for the team to get a sense of what they're going to end up with," says Brian Garbecki, P.E., LEED AP, vice president and Healthcare Center of Excellence leader at Gilbane Building Co., Providence, R.I. "It's immensely useful in the Lean project delivery process."
Beyond providing help in spotting design conflicts, BIM also helps the project team plan work sequencing and monitor construction progress, experts say. On the architectural side, it also helps C-level executives visualize the finished project and allows hospital staff to understand the patient-flow plan better.
BIM also plays a role in the health care design and construction industry's recent moves toward more prefabricated design and infrastructure elements, in which headwalls, mechanical-electrical-plumbing packages, exam rooms and bathrooms, masonry panels and even entire curtainwalls are pre-built in a controlled environment in a nearby facility and brought to the construction site for installation.
In addition to accelerating construction schedules and reducing labor costs, a prefabrication approach also can improve quality and reduce costly change orders or requests for information, according to HKS' Sprague, who's recently used the strategy at the 925,000-square-foot Capital Health Medical Center – Hopewell in Pennington, N.J., and the military's 947,000-square-foot replacement hospital at Fort Hood, Texas.
As BIM adoption moves down the project management chain, other advantages will become apparent, according to David Stokes, principal consultant, KLMK Group Inc., Richmond, Va.
"One of BIM's shortcomings right now is that fabricators for sheet metal and piping have their own software that talks to their machines for milling and cutting," he says. "When you can plug the BIM software right into the fabrication software, that will be a new level of efficiency."
Another strategy playing a bigger role in the construction process as teams try to keep costs down is the Lean practice of "pull scheduling" milestones backward from the planned completion date.
"Some of the things that we're looking at are just how we schedule a project," says McCarthy's Eaton. "We're utilizing pull scheduling pretty extensively to involve the last person in the process on the construction side as much as possible to remove waste, whether it be materials or man-hours."
'A very exciting time'
These cost-saving strategies are not limited to hospitals, but also may translate to the ambulatory facilities and physician group practice buildings that frequently are rising to the top of the construction manager's planning schedule in the wake of health care reform and the birth of the accountable care organization, experts say.
Indeed, given the questions surrounding the future configuration of the health care organization and the effects of the baby boomer wave, these methods need to be flexible to survive any contingency.
"It's a very exciting time to be in health care and I think we're dealing with a much more sophisticated C-level when it comes to their appreciation of the built environment," Sprague concludes. "The design and construction team is very challenged to be on top of the latest thinking, current technologies and operational concepts."
Mike Hrickiewicz is editor of Health Facilities Management.




