Making room
 While predicting the outcome of health care reform in the United States is growing ever more difficult, it is well-known that many emergency departments (EDs) will be forced to handle increasing patient demand, further constraining already scarce resources.
While predicting the outcome of health care reform in the United States is growing ever more difficult, it is well-known that many emergency departments (EDs) will be forced to handle increasing patient demand, further constraining already scarce resources.
Frequently, operational improvement plans are implemented in an effort to increase ED capacity. These plans focus on improving throughput and maximizing the productivity of ED staff, medical equipment and physicians. At the same time, much less attention has been devoted to understanding and optimizing productivity of the space in the ED, the hospital's second most costly resource.
By ensuring that health facility initiatives are consistent with, and supportive of, operational improvement strategies, EDs have a greater probability of maximizing their capacity than if either facility or process improvement initiatives were implemented without consideration of the other.
Size, configuration and intradepartmental support areas within the ED should be designed based on programmatic priorities, operational processes and productivity goals of the department and organization.
Flexible use planning
The trend in hospitals that are adding new inpatient beds is to build private rooms with the majority of rooms having similar design, medical equipment and supplies to offer flexibility and enhance patient safety. A similar approach can be implemented in the ED.
Standardization of examination rooms provides flexibility, allowing the ED to make the best use of its existing physical capacity while promoting efficiency and quality. Historically, a certain number of ED exam rooms have been identified and outfitted as specialty rooms, such as a gynecological room, ophthalmology or ear, nose and throat (ENT ) room, cast room or behavioral health room. These dedicated specialty rooms accommodate the necessary fixed equipment, or lack thereof in the case of behavioral health rooms, to care for that specific patient population's unique needs.
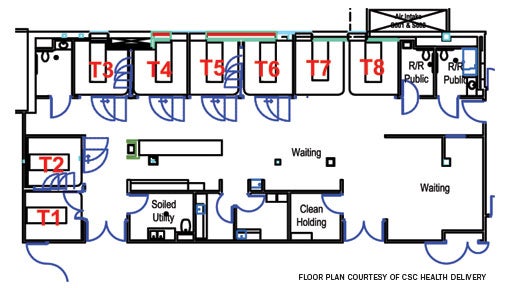 |
| The design of the advanced triage and treatment unit provides for patient triage in rooms T7 and T8, as well as six additional exam rooms, supplies and medical equipment for the treatment and discharge of nonemergent and emergent patients. |
However, in some EDs, the volume of patients requiring the unique setup these rooms offer is low, resulting in poor utilization of these spaces. If an ED makes these rooms available only to specialty patients, it will commensurately reduce its overall capacity and these specialty rooms may remain empty for long periods of time. While it is not an attractive alternative, many hospitals will utilize these specialty rooms for general ED patients and subsequently relocate these patients to other treatment rooms when the specialty room is needed.
To accommodate patients with special medical needs while still maximizing ED flexibility and capacity, many organizations design and equip almost all of their ED treatment rooms to handle most medical conditions. Equipment used to treat these specialty conditions that was previously fixed in dedicated rooms must now be mobile and readily accessible to the staff when needed.
While some equipment must still remain fixed, such as the boom in the trauma room or the chair in the ENT room, other equipment and supplies used to treat specific medical conditions can be located on mobile carts and brought into any room as needed. Examples of mobile equipment and supplies include gynecology equipment, casting supplies, slit lamp and vision machine.
In addition, most treatment rooms can be designed to be nearly identical so the orientation of the room, as well as the location of supplies and medical equipment, is consistent. The standardized room design, together with mobile specialty equipment, can greatly improve the throughput and efficiency of care delivery in the ED, which in turn can significantly increase capacity.
ED-based behavioral health treatment rooms have substantial design requirements to ensure the safety and well-being of patient and staff, making these rooms more difficult to modify to accommodate the general ED patient. Depending on the anticipated volume of behavioral health patients, an organization can determine an appropriate mix of dedicated and "swing" behavioral health rooms for its ED.
Dedicated behavioral health rooms leave nothing accessible with which patients could harm themselves. For example, the rooms have no exposed gases, suction, nurse call apparatus or chairs and are most often outfitted with door locks for security and a camera so the patient can be observed. It is possible though difficult to care for a general ED patient in a room designed primarily for the safety of behavioral health patients.
On the other hand, a "swing" behavioral health room is usually equipped with a full headwall, sink, telemetry monitoring, nurse call, suction and oxygen behind a "garage door" that can be raised to expose the medical equipment and gases needed to care for the general ED patient. While the swing room provides flexibility, each organization needs to assess its own patient volumes and programmatic priorities when deciding the appropriate proportion of dedicated and swing behavioral health rooms.
Allocating support spaces
The location and allocation of intradepartmental ED support spaces and equipment impacts staff travel time to retrieve items needed to care for patients. ED staff is frequently required to leave the patient treatment room to retrieve these supplies and equipment.
The distances traveled for these items can theoretically affect patient throughput and timeliness of care. In addition to the distance itself, a caregiver is likely to encounter distractions when he or she leaves the treatment room for any reason, thus increasing time away from the patient and negatively impacting throughput and patient care. Therefore, organizations are increasingly moving supplies and equipment closer to the patient, which addresses these concerns but may create others.
For example, while many health care managers believe that optimal patient care requires stocking the most commonly used medical supplies and linen in each exam room, there can be significant facility implications for storage, as well as operational impact on the service responsible for re-stocking the patient rooms.
An ED treatment room that accommodates two supply carts or storage cabinets should be programmed around 150 square feet, which is much larger than the typical ED treatment bay. The room design needs to accommodate the carts in a location that enhances ED staff workflow and provides accessibility to staff performing the restocking functions.
However, even with the majority of supplies in the ED patient rooms, it is often desirable to have less-frequently used supplies and linen stored in a location outside the treatment room. The challenge is to ensure that the correct amount and location of support space is available to allow the ED to maximize its ability to enhance patient throughput and, therefore, potentially increase capacity.
 |
| LEFT A decentralized nurses' station located in an ED is sized to accommodate workstations and computers for nursing staff and physicians. RIGHT A rapid admission unit is designed to support the admission process, initial nursing evaluation and some treatments for patients waiting for an inpatient bed. |
Whether equipment and supplies are stored in one central location, several smaller decentralized locations, within each exam room or in any combination, the organization must evaluate the operational and facility implications. It is important to first develop optimal workflow processes, then physical requirements and associated costs of the desired support space configuration before proceeding with facility design.
Also affecting throughput and patient care in the ED is the efficiency of services rendered to patients by individuals who are not part of the ED staff, which can add a significant amount of time to the overall length of stay. Providing access to appropriate work space and resources within the ED, to respiratory therapists, cardiology staff, consulting physicians and others who routinely provide care to ED patients, enable these care providers to work more efficiently within the ED.
Organizations are incorporating additional computers, telephones and other devices to support the workflow needs of non-ED staff and to encourage these individuals to complete their work in the ED rather than moving to another location.
In addition, diagnostic exams can lengthen a patient's ED visit, especially when the modalities are not located within or proximate to the ED.
From a health facility perspective, locating frequently utilized diagnostic services and equipment within the ED, near the ED or easily accessible to the ED can assist patient throughput. Interdepartmental and intradepartmental adjacencies of frequently accessed services should be an integral part of space planning in a hospital renovation or new construction project.
Finally, due to their lack of patient privacy and confidentiality as well as other reasons, using hall beds is not a preferable option. EDs should not plan to use hall beds as a primary means to meet their capacity needs, but should utilize hall beds only in situations where no other option exists to address extraordinary patient demand.
However, given the increasing patient volumes that many EDs are experiencing on a regular basis, and the time required to implement certain process and physical changes, the ability to accommodate hall beds on a temporary basis can be a legitimate, interim consideration.
Advanced triage and treatment
Advanced triage and treatment units come in many operational and space varieties, depending on the needs of the organization and the space that is available within or near the ED. The design and operation of the advanced triage and treatment unit provides for the handling of nonemergent patients and also some types of emergent patients using approved protocols when treatment rooms in the main ED are not available.
Most commonly, these units utilize physician and/or midlevel practitioner coverage during peak hours to treat and release nonemergent patients and to initiate diagnostic testing and treatment of emergent patients. The advanced triage and treatment unit can also serve as more than a typical "fast track" because certain emergent patients can receive full treatment and be discharged from this type of unit if a treatment room does not become available in the main ED during the course of care.
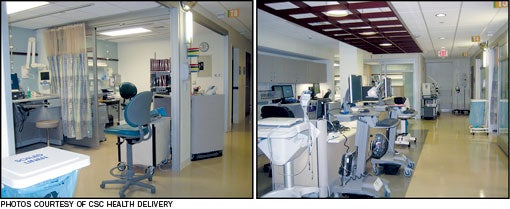 |
| LEFT An advanced triage and treatment unit created from a nursing unit is located proximate to the ED and features a triage desk and intake area where patients present upon entering. RIGHT The same unit with mobile PCs that registration staff use to register and discharge patients from the bedside. |
Because both nonemergent and emergent patients may be treated and discharged home or admitted from this unit, the advanced triage and treatment unit will provide surge capacity for the ED.
The size, configuration and equipment in the advanced triage and treatment unit depend on the volume and types of patients to be treated in the unit and the space available. Because one of the objectives is to start the workup and treatment of emergent patients, the treatment rooms and core support areas should be equipped as in the main area of the ED.
A nursing unit located near the ED could function as an advanced triage and treatment unit because the type and configuration of space closely matches the needs of the advanced triage and treatment unit. By providing physician or midlevel practitioner coverage in the unit and the needed space, medical equipment and supplies, care for the emergent patient can be initiated sooner. This will improve throughput and capacity along with the overall quality of patient care.
External improvements
ED capacity is driven not only by throughput within the ED but also by throughput within the organization. When inpatient beds are not available to accept ED admissions, those patients often remain in the ED for extended periods of time. The resulting bottleneck often compromises throughput and available ED capacity. This ultimately can lead to going on diversion.
By providing appropriately outfitted and staffed patient space outside the ED to accept patients who are in need of an inpatient or observation bed, ED patient treatment rooms can be made available sooner, thus increasing ED capacity. Effective operation of these units for patients awaiting admission relies upon developing efficient processes and protocols in addition to creating appropriate facilities.
Creation of a unit outside the ED for admitted patients waiting for an inpatient bed can free up ED capacity. It also can provide a location to initiate the registration and inpatient nursing admission process and potentially start treatment. These units are frequently called rapid admission units (RAUs).
Similar to the advanced triage and treatment units, RAUs have the same space and medical equipment requirements as an inpatient unit, including cardiac monitoring capability. RAUs have the added benefit of increasing patient satisfaction because a patient who previously might have been placed in an ED hall bed to wait is now housed in a unit specifically designed to expedite the admission process and begin care. When the patient is eventually placed in an inpatient bed, the burden on the inpatient nursing staff is greatly reduced because the staff in the RAU has begun or completed the admission process.
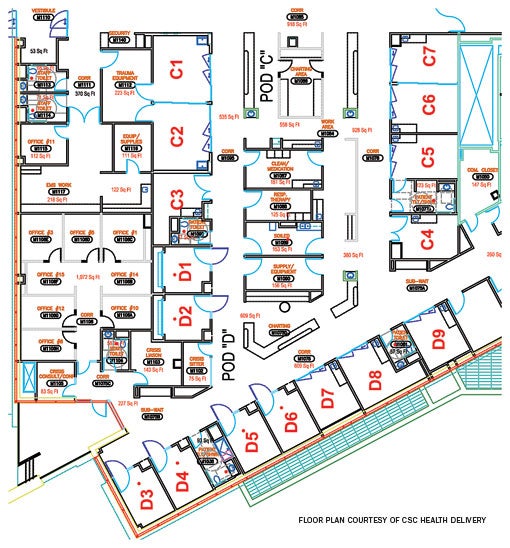 |
| Rooms D3 to D6 are designed as behavioral health rooms, while rooms D1 and D2 are configured as behavioral health swing rooms. The headwall in the swing room is behind a garage-type door that can be raised, easily converting it into a treatment room for general ED patients. |
The availability of private inpatient rooms may also reduce the time the patient is waiting in the ED for an inpatient bed assignment by allowing for timelier placement of the admissions. Gender, infectious disease and other patient-specific considerations that complicate patient bed assignments with semiprivate rooms are no longer relevant with private rooms. As with the RAU, private patient rooms may enable the organization to expedite admission of ED patients, thus turning over ED treatment rooms more quickly and increasing capacity with the same number of beds.
Carefully evaluate options
While there are many process improvement and facility initiatives available for increasing ED capacity, each organization must carefully evaluate options in view of its unique circumstances to arrive at the best decision for its emergency department.
ED physical resource initiatives that are in alignment with and in support of process improvement opportunities will give health care organizations the greatest likelihood of success in meeting capacity demands now and in the future.
Steve Straka is principal and Debbie Jacobs is manager at CSC Health Delivery, a health care planning practice based in Oak Brook, Ill. They can be reached at sstraka@csc.com and djacobs24csc.com, respectively.
| Sidebar - Operational and technology fixes |
| A number of operational and technology fixes are available to improve wait times and overcrowding in busy emergency departments (EDs). They include the following: • Redesign ED workflow to reduce handoffs, bottlenecks and delays in testing and results reporting; |
| Sidebar - Matching acuity to the setting |
| Strategic initiatives can be implemented to reduce the capacity demands on the emergency department (ED) by relocating less-acute patients to a more appropriate setting and thereby making more treatment rooms available to those who need emergent care. They include the following: • Implement financial incentives for providers to see patients in a primary care or other less-acute setting; |




